Back to Journals » Clinical Interventions in Aging » Volume 10
Hyperhomocysteinemia is an independent predictor of long-term clinical outcomes in Chinese octogenarians with acute coronary syndrome
Authors Fu Z , Qian G, Xue H, Guo J, Chen L, Yang X, Shen M, Dong W, Chen Y
Received 2 July 2015
Accepted for publication 17 August 2015
Published 15 September 2015 Volume 2015:10 Pages 1467—1474
DOI https://doi.org/10.2147/CIA.S91652
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Zhenhong Fu,1,* Geng Qian,1,* Hao Xue,1,* Jun Guo,1 Lian Chen,1 Xia Yang,1 Mingzhi Shen,2 Wei Dong,1 Yundai Chen1
1Department of Cardiology, Chinese People’s Liberation Army General Hospital, Beijing, People’s Republic of China; 2Department of Cardiology, Hainai Branch of Chinese People’s Liberation Army General Hospital, Sanya, Hainan, People’s Republic of China
*These authors contributed equally to this work
Objective: To evaluate the prognostic value of homocysteine (Hcy) in Chinese acute coronary syndrome (ACS) octogenarians.
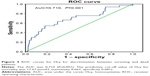
Methods: The study cohort comprised 660 consecutive ACS octogenarians who underwent coronary angiography. We classified the patients into three groups according to Hcy tertiles. Kaplan–Meier method was performed for survival and major adverse cardiac events (MACE) rates. Multivariate Cox regression was performed to identify mortality predictors. Receiver operating characteristic curve analysis was performed to predict the cutoff value of Hcy for all-cause mortality.
Results: The follow-up period was 28 (inter-quartile range: 16–38) months. Diastolic blood pressure, ratios of male, renal failure and old myocardial infarction in high plasma level Hcy (H-Hcy) group were higher than those in low (L-Hcy) and middle (M-Hcy) plasma level of Hcy groups (P<0.05). The Hcy level was positively correlated with uric acid level (r=0.211, P=0.001) and Cystatin C (Cys C) level (r=0.212, P=0.001) and negatively correlated with estimated glomerular filtration rate (r=−0.148, P=0.018). For the long-term outcomes, the cumulative survival rate of H-Hcy group was significantly lower than that of L-Hcy and M-Hcy groups (P=0.006). All-cause mortality and MACE of H-Hcy group were higher than those of L-Hcy and M-Hcy group (P=0.0001, P=0.0008). Hcy is an independent predictor for long-term all-cause mortality (odds ratio =2.26, 95% CI=1.23–4.16, P=0.023) and MACE (odds ratio =1.91, 95% CI=1.03–3.51, P=0.039). Receiver operating characteristic curve analysis indicated the predictive cutoff value of Hcy for all-cause mortality was 17.67 µmol/L (0.667, 0.681).
Conclusion: In ACS octogenarians, hyperhomocysteinemia is an important predictor for long-term all-cause mortality and MACE.
Keywords: acute coronary syndrome, octogenarian, homocysteine, clinical risk factors, outcomes
Introduction
Cardiovascular diseases are the leading causes of mortality worldwide and account for over 40% of all deaths in People’s Republic of China.1 In the past years, traditional risk factors contributing to a coronary heart disease event have been recognized and treated.2 However, despite predictive strategies, a great number of coronary heart disease cases remain unpredicted. Novel markers which can either anticipate or be associated with an incident coronary heart disease event have been introduced in recent decades.3 Homocysteine (Hcy) is one of them.4 Hcy is a nonessential amino acid that is known as a marker of endothelial injury.5 Elevated total Hcy is known to be able to increase oxidative stress, diminish vasodilation, stimulate the proliferation of vascular smooth muscle cells, alter the elastic properties of the vascular wall, and thus increase the risk for atherosclerosis.6,7 There is a positive association between total Hcy and coronary heart disease8–10 in general population of both People’s Republic of China and other countries.
The proportion of older population especially for octogenarians (age >80 years) increase quickly, and will grow to more than one in 12 by the year 2050.11 The increasing prevalence of coronary heart disease is associated with aging. Coronary angiography showed that the lesions of elderly patients were more complex, and the older patients presented higher comorbidity, poorer clinical outcomes, and higher all-cause mortality, compared with younger patients. The association of Hcy level with cardiovascular disease appears to be particularly strong in the very old, and Hcy level has even been shown to be a better predictor of cardiovascular mortality in this age group than models based on classic Framingham risk factors.12
However, the association between the level of Hcy and the stenosis of coronary artery, and the prognostic value of Hcy in long-term clinical outcomes are unclear, especially in octogenarians. The purpose of this study was to investigate the association between plasma Hcy and all-cause mortality, and long-term prognostic impact of plasma Hcy on Chinese acute coronary syndrome (ACS) octogenarians.
Methods
Study population
This single center study comprised 660 consecutive ACS patients (age >80 years) who had a complete clinical history of ACS, which was defined as unstable angina pectoris, non-ST-segment elevated myocardial infarction (MI) or ST-segment elevated MI,13 and who were admitted to our hospital and underwent coronary angiography from January 2006 to December 2011. All patients consented in writing to their participation in the study. The study complied with the declaration of Helsinki for investigation in human beings and was approved by the institutional ethics committee of the Chinese People’s Liberation Army General Hospital.
Data collection
On admission, every patient’s demographic characteristics, cardiovascular risk factors (such as diabetes, primary hypertension, hyperlipidemia, previous MI, previous stroke, chronic renal failure [CRF], and smoking), vital signs, information on laboratory data and examinations, cardiovascular medication were collected. Renal function was assessed using the baseline estimated glomerular filtration rate (eGFR). Impaired renal function was defined as an eGFR <60 mL/min/1.73 m2.14,15
Definitions
Hypercholesterolemia was defined as fasting serum total cholesterol level >5.5 mmol/L or use of lipid-lowering therapy at the time of the procedure. Hypertension was defined as blood pressure >140/90 mmHg or the use of antihypertensive medications. MI was diagnosed by raised creatine kinase MB greater than three times the upper limit of normal value. Diabetes mellitus was defined as hyperglycemia, requiring antidiabetic drugs or fasting blood sugar >7.0 mmol/L.
Coronary angiography
After admission, all patients underwent coronary angiography. An obstructive lesion causing ≥50% reduction of lumen diameter in at least one of the coronary arteries was defined as coronary artery disease (CAD). The lesion characteristics of coronary artery were recorded. The severity of coronary artery was calculated by Gensini score.16 The percutaneous coronary intervention (PCI) procedures were recorded.
Population grouping and follow-up
Our patients were divided into three groups according to Hcy tertiles. Regular follow-up was performed for all patients at a 6-month interval. Long-term clinical major adverse cardiac events (MACE), including all-cause death, MI, and repeat revascularization (repeat PCI or coronary artery bypass grafting), were collected and compared between the three groups.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences, version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables including age, heart rate, body mass index (BMI), blood pressure, eject fraction (EF), and laboratory data were expressed as the mean ± standard deviation or median (with inter-quartile range). The Student’s t-test was used if continuous variables were normally distributed, while the Wilcoxon two-sample test was used if continuous variables (such as Gensini score, C-reactive protein [CRP]) were not normally distributed. Categorical data were summarized as frequency. The chi-square test was used to compare categorical variables including sex, risk factors, ACS type, and medication. Correlation between plasma Hcy level and blood biochemistry indicators were performed using the Pearson correlation model. Survival rates of three groups were calculated according to the Kaplan–Meier method. Differences between survival curves of high plasma level of Hcy (H-Hcy), middle plasma level of Hcy (M-Hcy), and low plasma level of Hcy (L-Hcy) groups were tested by the log-rank test. A Cox proportional hazards model was used to identify predictors of all-cause mortality in ACS octogenarians. Odds ratios (ORs) were reported with corresponding 95% confidence intervals (CIs). The respective predictive cutoff values were constructed according to the receiver operating characteristic curves for Hcy for discrimination between surviving and dead patients. The areas under the curve were compared using Hanley and McNeil method, and the predictive cutoff value of Hcy for mortality was evaluated. All P-values were two-sided, and a P-value <0.05 was considered statistically significant.
Results
Baseline characteristics of patients
The baseline clinical characteristics of 621 (621/660, 94.09%) enrolled patients, who fulfilled the follow-up, were collected. Thirty-nine patients were lost during the follow-up because of wrong telephone number. Of the 621 patients, there were 451 men and 170 women. Patients were classified into three groups according to Hcy tertiles (<13.20 μmol/L, 13.21–18.28 μmol/L, and >18.29 μmol/L). The baseline clinical characteristics, medication, and treatment strategies of the three groups were shown in Table 1.
As compared with those in low (L-Hcy) and middle (M-Hcy) plasma level of Hcy groups, patients in H-Hcy group had higher diastolic blood pressure (DBP) and higher ratio of male (P<0.05), while there was no difference between other characteristics including age, heart rate, BMI, systolic blood pressure (SBP), EF, and Gensini score (P>0.05) (Figure 1). The ratios of CRF and history of MI were higher in H-Hcy group than in L-Hcy and M-Hcy groups (P<0.05). Among blood biochemistry indicators, plasma cystatin C (Cys C), uric acid (UA), and CRP concentrations were higher and eGFR level was lower in H-Hcy group than in L-Hcy and M-Hcy groups (P=0.001). In addition, no difference was found in medication use and treatment strategies between the three groups. No difference was found in ACS type (P>0.05).
  | Figure 1 Gensini score in three groups according to Hcy tertiles (<13.20 μmol/L, 13.21–18.28 μmol/L, and >18.29 μmol/L) (P=0.218). |
The distribution characteristics of lesions were similar between the three groups, and there was no significant difference between the three groups as to multivessel disease or number and distribution of target vessels. Stent implantations, including multistents and number of stents, were almost equal to one another (shown in Table 2).
The correlation between Hcy and blood biochemistry indicators
The UA level and Cys C level increased and eGFR level decreased with Hcy level (P<0.01). Further analysis indicated the Hcy level was positively correlated with UA level (r=0.211, P=0.001) and Cys C level (r=0.212, P=0.001), was negatively correlated with eGFR (r=-0.148, P=0.018).
Long-term outcomes
The duration of the follow-up was from 13 to 79 months (median, 28 months; inter-quartile range, 16–38 months). During the follow-up period, 18 patients (8.69%) died and 16 patients (7.73%) experienced reinfarction or revascularization in L-Hcy group, and the rate of MACE was 16.42%. Twenty-one patients (10.14%) died and ten patients (4.83%) experienced reinfarction or revascularization in M-Hcy group, and the rate of MACE was 14.97%. Forty-five patients (28.51%) died and 14 patients (6.76%) experienced reinfarction or revascularization in H-Hcy group, and the rate of MACE was 28.51%. The all-cause mortality and MACE rate in H-Hcy group were higher than those in L-Hcy and M-Hcy groups (P=0.0001, P=0.0008). However, there were no significant difference in the reinfarction and revascularization rates between the three groups (P=0.473) (Figure 2).
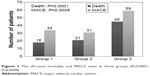  | Figure 2 The all-cause mortality and MACE rates in three groups (P=0.0001, P=0.0008). |
Figure 3 shows the Kaplan–Meier survival curves for all-cause death according to Hcy tertiles. The cumulative survival rate of H-Hcy group was significantly lower than that of L-Hcy and M-Hcy groups in the long term (P=0.006). H-Hcy group had a high risk of all-cause death.
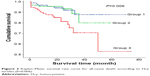  | Figure 3 Kaplan–Meier survival rate curve for all-cause death according to Hcy tertiles (P=0.006). |
Risk factors associated with mortality during follow-up
A Cox regression analysis was performed to determine the factors that were associated with all-cause death at the end of the follow-up. After being adjusted for general conditions including age, sex, heart rate, BMI, SBP and DBP, and EF, risk factors including diabetes mellitus, hypertension, hyperlipidemia, previous MI, stroke, and CRF, and blood biochemistry indicators including triglyceride, total cholesterol, low density lipoprotein-C, and fasting blood glucose, plasma Hcy concentration (OR=2.26, 95% CI=1.23–4.16, P=0.023) and Cys C concentration (OR=2.89, 95% CI=1.35–6.16, P=0.006) were the independent predictors for long-term mortality, plasma Hcy concentration (OR=1.91, 95% CI=1.03–3.51, P=0.039) and history of MI (OR=2.27, 95% CI=1.16–4.45, P=0.017) were the independent predictors for MACE.
Diagnostic power of Hcy for long-term mortality during follow-up
The respective predictive cutoff values were constructed according to the receiver operating characteristic curves for Hcy for discrimination between surviving and dead patients (Figure 4). The area under the curve was 0.710 (0.585, 0.796, P=0.001). The predictive cutoff value of Hcy for mortality was 17.67 μmol/L (sensitivity 0.667, specificity 0.681).
Discussion
In the present study, we have found that plasma Hcy concentration was an independent predictor for long-term mortality and MACE in ACS octogenarians after controlling conventional cardiovascular risk factors. Our study evaluated the effects of Hcy level on the clinical characters and coronary artery stenosis in ACS octogenarians for the first time, and showed a positive association between plasma Hcy level and Cys C and UA level, a negative association between plasma Hcy level and eGFR. The ratios of male, MI and CRF were higher in H-Hcy group. However, there was no relation between the coronary artery stenosis degree and Hcy level.
Hcy levels suggest a contribution of Hcy to cardiovascular diseases.17 H-Hcy are independently associated with the prevalence and extent of CAD.18,19 Hcy-lowering interventions should be used for preventing cardiovascular events occurrence.20 Although the association of Hcy level with cardiovascular disease appears to be particularly strong in the very old population and Hcy level has even been shown to be a better predictor of cardiovascular mortality in this age group than models based on classic Framingham risk factors,12 and elevated plasma total Hcy level was related to 30-day cardiovascular events in patients with acute myocardial infarction (AMI),21 there is still no consistent opinion about the relation between the Hcy level and long-term outcomes of coronary heart disease, especially for octogenarian ACS patients. In this study, the Hcy-ACS association in the octogenarian was independent of a number of risk factors, and the diagnostic power of Hcy for mortality was identified for the first time.
However, there were still some controversy opinions about the benefits from the treatments of folic acid and Hcy lowering. Some papers showed that folic acid and B vitamins treatments, despite significant Hcy lowering, did not reduce a combined end point of total cardiovascular events among high-risk women22 and the risk of recurrent cardiovascular disease after acute MI.23 These were not conflict with the conclusion of our research. First, the enrolled populations were different, our study was comprised of very old ACS patients, and other study was comprised of 60-years-old high-risk women; second, our result indicated the higher level of Hcy, the poorer prognosis, and we did not evaluate the lowering of plasma Hcy level with the prognosis.
The octogenarian ACS is a special population, accompanied with more traditional and novel risk factors and presenting more complex lesions, higher comorbidity, poorer clinical outcomes, and higher mortality. Few clinical researches were conducted on the risk factors of the prognosis in the very old ACS patients. Our earlier studies indicated that Gensini score was an independent predictor of long-term mortality in ACS octogenarians,24 and plasma Cys C level was an independent predictor for long-term mortality in ACS octogenarians with diabetes mellitus.25 In the present study, we performed a Cox regression analysis and adjusted general conditions and clinical risk factors, and showed the plasma elevated Hcy was an independent predictor for long-term mortality and MACE for octogenarian ACS.
In the present study, we found that the Hcy level was positively correlated with Cys C level (r=0.212, P=0.001) and UA level (r=0.211, P=0.001) in ACS octogenarians. These were consistent with some previous researches. As a member of the cysteine protease inhibitor superfamily, Cys C is synthesized by various nucleated cells and involved in the metabolism of Hcy. Cys C can inhibit Hcy degradation and increase serum Hcy level. Cys C could be a useful laboratory biochemical marker in predicting the severity of CAD and was associated with biochemical atherosclerosis markers Hcy.26 In patients with CAD, elevated Hcy was directly related to serum UA (P<0.001).27 Hyperhomocysteinemia had an OR for hyperuricemia of 1.7 for males and a significant association with hyperuricemia in screening subjects. The combined effect of these two factors accelerated atherosclerosis.28
Currently, the precise mechanism of hyperhomocysteinemia on the risk of coronary heart disease is not clear even for the prognosis, especially for the very old ACS patients. Hyperhomocysteinemia increased carotid intima-media thickness29 and as a prothrombotic factor, was related with platelet reactivity, which may be a possibly new challenge of aspirin therapy.30 Hcy increased arterial stiffness31 and impaired coronary artery endothelial function by increased increasing insulin resistance.32
In this study, we analyzed the relative indicators, and found no significant difference between H-Hcy group and L-Hcy group in fasting blood glucose, platelet, SBP and DBP. We found that CRP and Cys C were higher in H-Hcy group than in L-Hcy group. Our early study showed that CRP and Cys C were positively related in the very old ACS patients with diabetes mellitus. So we deduce that, in our study patients, H-Hcy may be accompanied with Cys C, promote the inflammatory reaction, and accelerate the prognosis.
Some limitations in interpretation of our study results should be kept in mind. Our study was a single center registry, so it offered observational data on nonrandomized patients. In addition, plasma Hcy level was measured on admission for a single point in the present study. As we did not know the serum Hcy levels during follow-up of 2 years, we were not able to consider this valuable information in our analysis.
Conclusion
All-cause mortality and MACE of ACS octogenarians increased with the level of plasma Hcy. Hyperhomocysteinemia was an important predictor for long-term mortality and MACE of ACS octogenarians. The predictive cut off value of Hcy for mortality was 17.67 μmol/L.
Acknowledgments
The authors thank the numerous physicians and study nurses who participated in data collection. This study was supported by the Chinese PLA Medical Science and Technology Youth Cultivate Project (fund number 2014QNP104) and Natural Science Foundation of China (fund number 81500269).
Author contributions
Zhenhong Fu, Hao Xue, and Geng Qian designed the study and drafted the manuscript. Jun Guo and Wei Dong collected and analyzed the results of clinical and laboratory data. Mingzhi Shen and Xia Yang analyzed the results of coronary angiography and evaluated the strategies of treatments. Lian Chen and Yundai Chen performed coronary angiography and PCI. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2095–2128. | ||
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. | ||
Wang TJ, Wollert KC, Larson MG, et al. Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham heart study. Circulation. 2012;126:1596–1604. | ||
Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–2639. | ||
Hayden MR, Tyagi SC. Homocysteine and reactive oxygen species in metabolic syndrome, type 2 diabetes mellitus, and atheroscleropathy: the pleiotropic effects of folate supplementation. Nutr J. 2004;3:4. | ||
Sen U, Tyagi SC. Homocysteine and hypertension in diabetes: does PPARgamma have a regulatory role? PPAR Res. 2010;2010:806538. | ||
Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338:1042–1050. | ||
Esteghamati A, Hafezi-Nejad N, Zandieh A, Sheikhbahaei S, Ebadi M, Nakhjavani M. Homocysteine and metabolic syndrome: from clustering to additional utility in prediction of coronary heart disease. J Cardiol. 2014;64(4):290–296. | ||
Schaffer A, Verdoia M, Cassetti E, Marino P, Suryapranata H, De Luca G; Novara Atherosclerosis Study Group (NAS). Relationship between homocysteine and coronary artery disease. Results from a large prospective cohort study. Thromb Res. 2014;134(2):288–293. | ||
Wu Y, Huang Y, Hu Y, et al. Hyperhomocysteinemia is an independent risk factor in young patients with coronary artery disease in southern China. Herz. 2013;38:779–784. | ||
Foot DK, Lewis RP, Pearson TA, Beller GA. Demographics and cardiology, 1950–2050. J Am Coll Cardiol. 2000;35:1067–1081. | ||
de Ruijter W, Westendorp RG, Assendelft WJ, et al. Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ. 2009;338:a3083. | ||
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. | ||
Zhang L, Zuo L, Xu G, et al. Community-based screening for chronic kidney disease among populations older than 40 years in Beijing. Nephrol Dial Transplant. 2007;22:1093–1099. | ||
Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–2944. | ||
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. | ||
Catena C, Colussi G, Nait F, Capobianco F, Sechi LA. Elevated homocysteine levels are associated with the metabolic syndrome and cardiovascular events in hypertensive patients. Am J Hypertens. 2015; 28(7):943–950. | ||
Schaffer A, Verdoia M, Cassetti E, Marino P, Suryapranata H, De Luca G. Relationship between homocysteine and coronary artery disease. Results from a large prospective cohort study. Thromb Res. 2014;134:288–293. | ||
Akyurek O, Akbal E, Gunes F. Increase in the risk of ST elevation myocardial infarction is associated with homocysteine level. Arch Med Res. 2014;45:501–506. | ||
Marti-Carvajal AJ, Sola I, Lathyris D. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev. 2015;1:CD006612. | ||
Ma Y, Li L, Geng XB, et al. Correlation between hyperhomocysteinemia and outcomes of patients with acute myocardial infarction. Am J Ther. Epub 2014 Nov 17. | ||
Albert CM, Cook NR, Gaziano JM, et al. Effect of folic acid and B vitamins on risk of cardiovascular events and total mortality among women at high risk for cardiovascular disease: a randomized trial. JAMA. 2008;299:2027–2036. | ||
Bonaa KH, Njolstad I, Ueland PM, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006;354:1578–1588. | ||
Fu Z, Xue H, Dong W, et al. Correlation between comprehensive evaluation of coronary artery lesion severity and long-term clinical outcomes in Chinese octogenarians with acute coronary syndrome. Heart Lung Circ. 2014;23:1125–1131. | ||
Fu Z, Xue H, Guo J, et al. Long-term prognostic impact of cystatin c on acute coronary syndrome octogenarians with diabetes mellitus. Cardiovasc Diabetol. 2013;12:157. | ||
Dandana A, Gammoudi I, Chalghoum A, et al. Clinical utility of serum cystatin c in predicting coronary artery disease in patients without chronic kidney disease. J Clin Lab Anal. 2014;28:191–197. | ||
Verdoia M, Schaffer A, Pergolini P, et al. Homocysteine levels influence platelet reactivity in coronary artery disease patients treated with acetylsalicylic acid. J Cardiovasc Pharmacol. 2015;66(1):35–40. | ||
Cohen E, Levi A, Vecht-Lifshitz SE, Goldberg E, Garty M, Krause I. Assessment of a possible link between hyperhomocysteinemia and hyperuricemia. J Investig Med. 2015;63:534–538. | ||
Lai S, Dimko M, Galani A, et al. Early markers of cardiovascular risk in chronic kidney disease. Ren Fail. 2015;37:254–261. | ||
Karolczak K, Kamysz W, Karafova A, Drzewoski J, Watala C. Homocysteine is a novel risk factor for suboptimal response of blood platelets to acetylsalicylic acid in coronary artery disease: a randomized multicenter study. Pharmacol Res. 2013;74:7–22. | ||
Fu S, Luo L, Ye P, Xiao W. Multimarker analysis for new biomarkers in relation to central arterial stiffness and hemodynamics in a Chinese community-dwelling population. Angiology. Epub 2015 Apr 16. | ||
Liu J, Xu Y, Zhang H, Gao X, Fan H, Wang G. Coronary flow velocity reserve is impaired in hypertensive patients with hyperhomocysteinemia. J Hum Hypertens. 2014;28:743–747. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.