Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
How to Choose the Appropriate Posterior Slope Angle Can Lead to Good Knee Joint Function Recovery in Total Knee Arthroplasty?
Authors Pan XQ, Liu JH, Zhang JL, Chai A, Li F, Shu L, Zhao W
Received 25 June 2023
Accepted for publication 17 September 2023
Published 25 September 2023 Volume 2023:19 Pages 767—772
DOI https://doi.org/10.2147/TCRM.S427542
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Xi-Qing Pan, Jin-Hui Liu, Jiang-Li Zhang, An Chai, Feng Li, Lei Shu, Wei Zhao
Department of Joint Surgery, Third Hospital of Shijiazhuang, Shijiazhuang, Hebei, People’s Republic of China
Correspondence: Jin-Hui Liu, Department of Joint Surgery, Third Hospital of Shijiazhuang, No. 15 Tiyu South Street, Shijiazhuang, Hebei, 050011, People’s Republic of China, Tel +86 13191872146, Fax +86 31185990628, Email [email protected]
Objective: In this study, we aim to examine the effects of osteotomy under varying posterior slope angles on knee joint function recovery following knee arthroplasty.
Methods: We conducted a retrospective analysis from September 2015 to September 2018 on 240 patients who underwent knee arthroplasty three years previously. The study participants were categorized based on changes in the angle of the posterior slope before and after surgery: Group 1, > 5°; Group 2, 3°– 5°; Group 3, 0°– 3°; Group 4, − 3°– 0°; Group 5, < − 3°. All participants were affected with knee osteoarthritis. The Knee Society Clinical Rating System (KSS) knee function score, Western Ontario and McMaster Universities Arthritis Index (WOMAC) knee function score, Visual Analogue Scale (VAS) pain score, and postoperative complications were measured 3 years after surgery.
Results: The level of pain experienced by the patients decreased significantly than before, with pain scores ranging from 1.0– 3.0, and there was a statistical difference between groups (H = 93.400, P < 0.001). The KSS score increased, with group 5 having the lowest median score of 78.0 and group 2 having the highest median score of 97.0, and there was a statistical difference between groups (H = 164.460, P < 0.001). The WOMAC score was reduced, with the median score being 24.0, 11.0, 14.0, 20.0, and 26.0, in the five groups, respectively. Group 5 had the highest score, while Group 2 had the lowest score, and there was a statistically significant difference between groups (H = 164.223, P < 0.001). No symptoms such as periprosthetic femoral fracture, prosthetic loosening, or pad wear were detected in patients postoperatively.
Conclusion: Osteotomy at various posterior slope angles in total knee arthroplasty impacts postoperative knee function rehabilitation. An excessive increase or decrease in angle can have an impact on the postoperative recovery of knee function.
Keywords: functional rehabilitation, knee arthroplasty, knee function, knee osteoarthritis, posterior slope angle, tibial osteotomy, tibial slope, TKA
Background
Knee arthroplasty, which has become one of the most effective surgical alternatives for the treatment of severe osteoarthritis, can significantly relieve patients’ pain and restore knee joint function. Mild osteoarthritis patients can relieve symptoms through oral nonsteroidal drugs, physical therapy and arthroscopy. Knee arthroplasty surgery has become the ultimate treatment plan for patients with severe osteoarthritis.1 After a 15-year period following surgery, the utilization rate of the prosthesis in knee arthroplasty can exceed 90%. Most patients have achieved good treatment results, early recovery of normal life, greatly improving the quality of life.2 However, due to the unsatisfactory functional recovery of the affected limb or the inappropriate placement of the prosthesis, revision total knee arthroplasty may be needed for affected limbs in the early postoperative period.3,4 Sharkey et al reported that the likelihood of surgical failure in knee arthroplasty surpassed 20% due to insufficient force lines and displaced prosthesis placement, but that the prevalence of such errors could be considerably reduced with the improvement in surgical expertise.5–7 Previous research focused on the influence of a poor force line in the coronal plane of a knee prosthesis on postoperative knee function.8–12 Matsuda et al found that postoperative knee varus can decrease patients’ knee joint function.13 The finite element analysis revealed that a poor force line in the coronal plane of the knee joint can result in tibial tray settlement of the knee prosthesis. Barrack et al reported the effect of rotational malalignment of knee prosthesis on postoperative knee function recovery. Excessive internal rotation of the femoral prosthesis was shown to cause postoperative patellofemoral problems in patients. In finite element analysis experiments, internal rotation of the femoral prosthesis was observed to produce changes in the patellar trajectory after surgery.14,15
Many clinical and specimen tests have been conducted to determine the appropriate posterior slope angle, although osteotomy error makes the experiment much more challenging.16,17 Barrett et al discovered that more than 30% of surgeries had a more than 2° error between preoperative planning and postoperative reality. Neither the seniority of surgeons nor advanced navigation technology have been able to prevent such accident at present. Differences in the soft tissue surrounding the knee may also affect the pressure of patellofemoral joint and the strength of quadriceps femoris. As a result, there are ongoing disagreements about how to choose the appropriate posterior slope angle.18
Previous research has shown that reducing the posterior slope angle in knee arthroplasty while retaining the posterior cruciate ligament can prevent paradoxical anterior translation, allowing for functional rehabilitation of the knee joint.15 However, the trial design was modest at the time, with a small number of cases and a short follow-up period. In this study, we collected a large number of samples to further investigate the long-term influence of changes in posterior slope angle in knee arthroplasty retaining posterior cruciate ligament on the postoperative rehabilitation of the knee function.
Prosthesis type, patellofemoral joint pressure, and postoperative knee motion can affect the incidence of periprosthetic femoral fracture, prosthetic loosening, pad wear, and other related complications.19 As there is no research on the relationship between these complications and posterior slope angle, we also evaluated the effect of posterior slope angle on the incidence of periprosthetic femoral fracture, prosthetic loosening, pad wear, and other related complications. The purpose of this retrospective study is to investigate the effect of posterior tibial slope on clinical results in total knee replacement arthroplasty.
Materials and Methods
General Information
We performed a retrospective study performed from September 2012 to September 2015 on 240 patients who had knee arthroplasty three years previously with an average age of 62.5 y (57–68 y) at the time of surgery. All TKAs were performed by the same senior surgeon using a CR prosthesis (Waldemar Link GmbH & Co. KG, Hamburg, Germany, Medium) using a consistent, controllable, and reproducible technique. In accordance with the procedure described by Utzschneider et al, the PTS was determined by measuring the proximal tibial anatomical axis on the preoperative and postoperative lateral radiographic images, and the slope was measured based on the configuration of the metal backing by a computer program. The posterior slope angle was measured before and after surgery (Figure 1).20 The patients were divided into five groups based on changes in posterior slope angle before and after surgery: Group 1, > 5°; Group 2, 3°–5°; Group 3, 0°–3°; Group 4, −3°–0°; Group 5, < −3°.
 |
Figure 1 Posterior slope angle before and after surgery; (a) Posterior slope angle before surgery; (b) Posterior slope angle after surgery. |
Western Ontario and McMaster Universities Arthritis Index (WOMAC), Knee Society Clinical Rating System (KSS) knee function score, and Visual Analogue Scale (VAS) scores were measured 3 years after surgery. WOMAC mainly evaluated the pain, stiffness, and activity disorders of patients in their daily life and work. KSS mainly evaluated the pain, range of motion and stability of the patient’s knee joint.
Statistical Methods
SPSS21.0 was used for statistical analysis. The scale scoring data are expressed as median—M (QL, QU) and were compared between groups using the Kruskal–Wallis (K-W) H-test. P < 0.05 indicates statistically significant difference.
Results
Preoperative Score
The knee function and pain were scored using WOMAC, KSS, and VAS scales before surgery. The WOMAC scores ranged from 24.0–25.0, with no significant difference between groups (H = 8.567, P = 0.070). The KSS had a median score of 25.0, with no significant difference between groups based on the K-W H-test (H = 1.632, P = 0.825). The median KSS score was 8.5, with no significant difference between groups (H=0.286, P = 0.998). Table 1 displays the results.
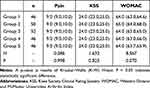 |
Table 1 Preoperative Pain and Function Levels of the Five Groups |
Postoperative Score
The WOMAC score was reduced, with a median of 24.0, 11.0, 14.0, 20.0, and 26.0, in the five groups respectively, and there was statistical difference between groups (H=164.223, P <0.001). The KSS score increased, and there was statistical difference between groups (H = 164.460, P < 0.001). Pain was relieved, with a VAS score of 1.0–3.0, and there was statistical difference between groups (H= 93.400, P < 0.001). Subgroup analysis had be done. The significant difference between each group had been found. The results are shown in Table 2.
 |
Table 2 Postoperative Pain and Functional Scores of the Five Groups |
Postoperative Complications
None of the patients developed complications such as periprosthetic femoral fracture, prosthetic loosening, and pad wear.
Discussion
Many studies have been conducted to improve surgical techniques to avoid incorrect alignment of knee prostheses in the coronal and rotational planes, but few studies have been conducted to investigate the influence of modifications in the sagittal plane force line on postoperative knee function recovery.21–25 Furthermore, there are still disagreements on the appropriate range of posterior slope angle during surgery. Changes in the posterior slope angle can both raise and decrease the postoperative knee function score. Increasing the posterior slope angle not only increases the flexion range of the knee joint, but also the intensity of the quadriceps femoris flexion. However, some investigations, have discovered that a greater posterior slope angle can result in anterior translation of the tibial prosthesis and wear behind the tibial pad. Furthermore, the posterior slope angle affects different types of knee prostheses to varying degrees. An increasing number of studies have revealed that posterior slope angle affects knee joint prosthesis preserving posterior cruciate ligament more than posterior stabilized knee joint prosthesis in knee arthroplasty.10–13
We conducted a retrospective study from September 2012 to September 2015 on 240 patients who underwent knee arthroplasty 3 years previously. The VAS, WOMAC, and KSS scores of the five groups differed statistically. Group 2 had the lowest VAS and WOMAC scores, while also having the highest KSS scores. Groups 1 and 5 exhibited poor postoperative function recovery, demonstrating that changes in the angle of the posterior slope in total knee arthroplasty impacted knee function rehabilitation. Too much increase or reduction in angle can hinder the rehabilitation of the knee after surgery. No problems such as periprosthetic femoral fracture, prosthetic loosening, or pad wear were detected in patients postoperatively.
Group 2 had the lowest VAS and WOMAC scores, while also having the highest KSS score. Group 2 experienced a small reduction in the angle of the posterior slope following surgery, consistent with our earlier experimental findings. This also confirms our prior theory that suitably lowering the posterior slope angle in the application of prostheses preserving the posterior cruciate ligament may prevent paradoxical anterior translation, thereby enhancing the rehabilitation of the postoperative knee function. Group 1 had a greater decrease in the angle of the posterior slope and had poor postoperative function recovery. It is possible that a posterior slope angle that is too small can restrict the flexion range of patients, resulting in prepatellar pain. The functional recovery in Group 5 was the weakest. It is believed that a large posterior slope angle places the femur in a posterior position relative to the tibia, resulting in a decreased moment arm of the quadriceps femoris tendon and generating patient discomfort. In addition, a large posterior slope angle can result in joint relaxation. In Groups 3 and 4, the posterior slope angle was most similar to that before surgery, but the functional score was lower compared to Group 2, which may be a result of our use of a prosthesis that preserves the posterior cruciate ligament. As the prosthesis-preserving posterior cruciate ligament preserves the posterior cruciate ligament while removing the anterior cruciate ligament, there is a change in postoperative biomechanical balance. As a result, while the physiological angle of the posterior slope angle is restored, it fails to maximize postoperative knee function recovery.
In our study, no postoperative complications such as periprosthetic femoral fracture, prosthetic loosening, or pad wear were found, which could be attributed to the short follow-up duration.
Changes in the posterior slope angle after total knee arthroplasty have an impact on knee function rehabilitation. An excessive increase or reduction in angle can have an impact on the postoperative rehabilitation of knee function.26
Consistent with other studies, the present study has several strengths and weaknesses. One limitation was that there are many factors related to postoperative functional recovery after TKA, and the posterior slope is only one of them. Hence, a follow-up study is needed to discuss this point.
Conclusion
Osteotomy at various posterior slope angles in total knee arthroplasty impacts postoperative knee function rehabilitation. An excessive increase or reduction in angle can have an impact on the postoperative rehabilitation of knee function.
Data Sharing Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of the Third Hospital of Shijiazhuang. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
No external funding received to conduct this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Biz C, Maso G, Gambato M, et al. Challenging surgical treatment of displaced articular tibial plateau fractures: do early knee radiographic features have a predictive value of the mid-term clinical functional outcomes? Orthop Surg. 2019;11(6):1149–1162. doi:10.1111/os.12577
2. Siviero P, Marseglia A, Biz C, et al. Quality of life outcomes in patients undergoing knee replacement surgery: longitudinal findings from the QPro-Gin study. BMC Musculoskelet Disord. 2020;21(1):436. doi:10.1186/s12891-020-03456-2
3. Khasian M, Meccia BA, LaCour MT, et al. Effects of posterior tibial slope on a posterior cruciate retaining total knee arthroplasty kinematics and kinetics. J Arthroplasty. 2021;36(7):2379–2385. doi:10.1016/j.arth.2020.12.007
4. Faschingbauer M. Editorial commentary: posterior tibial slope: the “unknown size” of the knee joint. Arthroscopy. 2021;37(1):250–251. doi:10.1016/j.arthro.2020.10.024
5. Dean RS, Larson CM, Waterman BR. Posterior tibial slope: understand bony morphology to protect knee cruciate ligament grafts. Arthroscopy. 2021;37(7):2029–2030. doi:10.1016/j.arthro.2021.05.006
6. Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi:10.1097/00003086-200211000-00003
7. Ersin M, Demirel M, Civan M, Ekinci M, Akgül T, Şen C. The effect of posterior tibial slope on anteroposterior stability in posterior cruciate retaining total knee arthroplasty. BMC Musculoskelet Disord. 2023;24(1):390. doi:10.1186/s12891-023-06507-6
8. Dennis DA, Komistek RD, Hoff WA, et al. In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res. 1996;33(1):107–117. doi:10.1097/00003086-199610000-00015
9. Dennis DA, Komistek RD, Mahfouz MR, et al. Multicenter determ- ination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;41(6):37–57. doi:10.1097/01.blo.0000092986.12414.b5
10. Dennis DA, Komistek RD, Scuderi GR, et al. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007;46(4):53–60. doi:10.1097/BLO.0b013e31812f785d
11. Eisenhuth SA, Saleh KJ, Cui Q, et al. Patellofemoral instability after total knee arthroplasty. Clin Orthop Relat Res. 2006;44(6):149–160. doi:10.1097/01.blo.0000214415.83593.db
12. Fujimoto E, Sasashige Y, Tomita T, et al. Significant effect of the posterior tibial slope on the weight-bearing, midflexion in vivo kinematics after cruciate-retaining total knee arthroplasty. J Arthroplasty. 2014;29(12):2324–2330. doi:10.1016/j.arth.2013.10.018
13. Matsuda S, Kawahara S, Okazaki K, et al. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013;47(1):125–127.
14. Massin P, Gournay A. Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthro Plasty. 2006;21(6):889–896. doi:10.1016/j.arth.2005.10.019
15. Pan XQ, Peng AQ, Wang F, et al. Effect of tibial slope changes on femorotibial contact kinematics after cruciate-retaining total knee arthrop- lasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3549–3555. doi:10.1007/s00167-016-4384-7
16. Ritter MA, Faris PM, Keating EM, et al. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;29(9):153–156.
17. McLean SG, Oh YK, Palmer ML, et al. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am. 2011;93(14):1310–1317. doi:10.2106/JBJS.J.00259
18. Barrett WP, Mason JB, Moskal JT, et al. Comparison of radiographic alignment of imageless computer-assisted surgery vs conventional instrumentation in primary total knee arthroplasty. J Arthroplasty. 2011;26(8):1273. doi:10.1016/j.arth.2011.04.037
19. Nowakowski AM, Kamphausen M, Pagenstert G, et al. Influence of tibial slope on extension and flexion gaps in total knee arthroplasty: increasing the tibial slope affects both gaps. Int Orthop. 2014;38(10):2071–2077. doi:10.1007/s00264-014-2373-3
20. Utzschneider S, Goettinger M, Weber P, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1643–1648. doi:10.1007/s00167-011-1414-3
21. Van Dommelen BA, Fowler PJ. Anatomy of the posterior cruciate ligament. A review. Am J Sports Med. 1989;17(1):24–29. doi:10.1177/036354658901700104
22. Stulberg SD. How accurate is current TKR instrumentation? Clin Orthop Relat Res. 2003;41(6):177–184. doi:10.1097/01.blo.0000093029.56370.0f
23. Victor J, Bellemans J. Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res. 2006;459(2):53–58. doi:10.1097/01.blo.0000238792.36725.1e
24. Tsukeoka T, Tsuneizumi Y, Lee TH. The effect of the posterior slope of the tibial plateau osteotomy with a rotational error on tibial component malalignment in total knee replacement. Bone Joint J. 2013;95-B(9):1201–1203. doi:10.1302/0301-620X.95B9.31775
25. Stein A, Fleming B, Pope MH, et al. Total knee arthroplasty kinematics. An in vivo evaluation of four different design. J Arthroplasty. 1988;3:31–36. doi:10.1016/S0883-5403(88)80005-6
26. Akbari Shandiz M, Boulos P, Saevarsson SK, et al. Changes in knee shape and geometry resulting from total knee arthroplasty. Proc Inst Mech Eng H. 2018;232(1):67–79. doi:10.1177/0954411917743274
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
