Back to Journals » Risk Management and Healthcare Policy » Volume 16
How Can China’s New Health Care Reform Promote the Balance of Interest Game?–Based on Game Evolution and Simulation Analysis
Authors Gong H, Wang X , Zhang T , Li J, Chen B
Received 9 June 2023
Accepted for publication 20 July 2023
Published 7 August 2023 Volume 2023:16 Pages 1435—1454
DOI https://doi.org/10.2147/RMHP.S422296
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Hanxiang Gong,1,2 Xi Wang,1 Tao Zhang,1 Jinghua Li,3 Baoxin Chen1
1Faculty of Humanities and Social Sciences, Macao Polytechnic University, Macao, People’s Republic of China; 2The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, People’s Republic of China; 3School of Public Health, Guangzhou Medical University, Guangzhou, Guangdong, People’s Republic of China
Correspondence: Xi Wang, Faculty of Humanities and Social Sciences, Macao Polytechnic University, Macao, 999078, People’s Republic of China, Tel +8618029928803, Fax +86853-28718003, Email [email protected]
Purpose: The new round of medical reform is a significant exploration of reform in the public service sector in China. Health insurance regulatory departments, medical institutions, and patients, as critical stakeholders in China’s medical reform, play a crucial role in the success of the reform through their strategic interactions.
Patients and Methods: Starting from the perspective of bounded rationality, applies evolutionary game theory to establish an evolutionary game model for the collaborative governance of health insurance regulatory departments, medical institutions, and patients and analyzes the stability of each party’s strategy and the sensitivity of parameters in the tripartite game system.
Results: The study shows that an equilibrium point will be formed when medical institutions provide reasonable treatment, patients choose to accept treatment, and health insurance regulatory departments adopt a lenient regulatory strategy, maximizing the interests of all parties involved in the game. Factors such as the benefits of unreasonable treatment by medical institutions, fines, and regulatory costs impact the decision-making of health insurance regulatory departments. To maximize social welfare, health insurance regulatory departments should reform payment methods, adjust medical service behaviors of medical institutions, and guide the rational allocation of medical resources; the government should increase subsidies for the operation of medical institutions and the intensity of penalties; regulatory departments should reduce regulatory costs and introduce third-party forces to strengthen health insurance supervision further.
Conclusion: The research findings of this paper will provide valuable insights into some countries’ medical and health reform.
Keywords: new health care reform, health insurance regulators, medical institutions, patients, evolutionary game
Introduction
Medical reform is a global challenge and a significant livelihood project. Since the beginning of the 21st century, the Chinese government has been committed to exploring a new path for medical reform different from the past. In March 2009, the release of the “Opinions on Deepening Medical and Health System Reform” marked the official launch of the “new medical reform”.1 Under the central government’s operational guidance and local governments’ active exploration, reform experiments have been widely carried out across the country.
Over the past decade, the central government and health departments have made multifaceted efforts. China’s investment in medical resources has gradually increased, with health conditions continuously improving.2–4 In 2021, government health expenditure reached 2,067.606 billion yuan, the total number of medical and health institutions reached 1,030,935, the number of beds in medical and health institutions reached 945,010, and the number of medical and health personnel reached 12.3003 million, an increase of 338.06%, 12.48%, 114.01%, and 79.73% respectively compared to 2009. There has also been a significant improvement in “medical output”. In 2018, the total number of visits to medical and health institutions nationwide reached 8.472 billion, and the number of hospitalized patients reached 201.55 million, an increase of 58.38% and 137.45%, respectively, compared to 2009.5,6
Since the Chinese government launched the new round of medical reform in 2009, specific achievements have been made in promoting medical reform. However, we should also recognize that the deeper reason behind these achievements is the mutual restraint and game-playing among the stakeholders. Only by ensuring a more reasonable distribution of interests among the government, medical institutions, and patients can the smooth progress of medical reform be guaranteed. Numerous data show that the problems of “difficulty in seeking medical treatment and high medical expenses” have not been effectively resolved during China’s “new medical reform”.7–9 The continuous advancement of China’s new medical reform is, in fact, a constant balancing of the interests of various stakeholders in the reform. The ultimate goal is to effectively reduce the burden of medical expenses for residents while ensuring the reasonable interests of all parties and thoroughly solving the problem of difficulties in seeking medical treatment.
In the context of China’s healthcare reform, the relationship between the healthcare insurance regulatory authorities, medical institutions, and patients is dynamic rather than static. This dynamism arises from the continuous interaction and competition among the various stakeholders, whose interests and goals are subject to constant change. As the leading force and policy maker in the healthcare reform, the government aims to ensure the stability and safety of healthcare insurance funds, as well as improve their utilization efficiency. The healthcare insurance regulatory authorities, as the decision-making body, seek to balance the sustainability and social equity of healthcare insurance funds, while also enhancing the allocation efficiency of medical resources. Medical institutions, particularly public hospitals, face the dual challenge of fulfilling their public service mission and pursuing economic benefits in the market-oriented environment. They must ensure the quality and efficiency of healthcare services, while also meeting development needs such as infrastructure expansion, technological advancements, and reasonable compensation for medical staff, all of which rely on financial support.10–12 Patients, as beneficiaries of healthcare services, aspire to receive high-quality diagnosis and treatment while safeguarding their own interests. They advocate for reasonable healthcare costs and equitable distribution of medical resources to meet their individual healthcare needs. Therefore, constructing an adaptable gaming environment that promotes cooperation and coordination among the various stakeholders is a critical challenge for China’s new healthcare reform.
In the process of China’s new round of healthcare reform, the healthcare insurance regulatory authorities, medical institutions, and patients need to jointly govern and share interests. Only by taking the healthcare insurance regulatory authorities as the guiding force, the medical institutions as the main body, and the interests of patients as the starting and focal point, can a mutually beneficial gaming mechanism be constructed to ensure the healthy development of China’s healthcare services industry. The achievements of the new medical reform over the past decade have been remarkable, yet they do not match public expectations.13,14 Building a mutually beneficial and win-win interest game mechanism for multiple stakeholders should be the top priority for the next step of medical reform. In light of this, Aims to contribute to the field by constructing a tripartite evolutionary game model for medical insurance regulatory authorities, medical institutions, and patients based on the perspective of evolutionary game theory. This model will analyze the strategic stability of each game participant and investigate the influence of various factors on strategy selection. Additionally, Matlab2020b will be employed to conduct simulation analysis and validate the effectiveness of the model under different initial conditions. Ultimately, this research will provide valuable insights and propose relevant countermeasures and suggestions to promote reasonable medical treatment in medical institutions.
Background
The Evolution of China’s New Healthcare Reform
On March 17, 2009, the Central Committee of the Communist Party of China and the State Council issued the “Opinions on Deepening the Reform of the Medical and Health System”, proposing the establishment of a basic medical and health system covering urban and rural residents to achieve the goal of universal access to essential medical and health services.15 The new medical reform highlights top-level design, focusing on the basic principles, strengthening grassroots health construction, and alleviating the difficulties and high costs of medical treatment that the public strongly reflects. After 2009, the new medical reform began to move towards multi-dimensional and multi-faceted systemic reform.16,17 The development process of the new medical reform can be divided into three stages:3 The first stage is from 2009 to 2010, which serves as the beginning of the new medical reform. The main task is to effectively implement top-level design and conduct preliminary exploration, including establishing the essential drug system, expanding medical insurance coverage, and popularizing essential public health services. The second stage is from 2011 to 2015, with the core being the comprehensive deepening of medical reform. Based on the achievements of the initial stage, this phase is committed to the coordinated and collaborative advancement of five key areas: social security system, essential drug system, equalization of basic public health services, and public hospital reform. The most important achievements during this period were the cancellation of drug markups, the transformation of payment methods, the adjustment of service prices, and the reform of the compensation system for public hospitals. The third stage is from 2016 to the present, accompanied by the advent of the information age and the significant data era. Health technology innovation injects new vitality into transforming health management methods.18,19 During this period, “health” becomes the central policy theme, and the medical reform goal is no longer limited to essential medical and health services. The focus is on continuously meeting people’s health expectations, adhering to disease prevention and control, promoting the complementarity of technology and health, and safeguarding the health rights of every citizen.
Major Achievements of China’s New Health Care Reform
Following the new medical reform, China has gradually established four systems and eight supporting measures.15 The four systems are the public health service, medical service, medical insurance, and drug supply guarantee systems.20 The eight measures mainly include a coordinated and unified medical and health management system, an efficient and standardized operation mechanism for medical and health institutions, a government-led diversified health investment mechanism, a scientific and rational medical price formation mechanism, a strict and effective medical and health supervision system, a sustainable development mechanism for medical and health technology innovation and talent guarantee, a practical and shared medical and health information system and a medical and health legal system.
Since the launch of a new round of medical reform in 2009, China has successively implemented measures such as the cancellation of drug markups pilot, nationwide promotion of zero drug markups, centralized procurement of medical consumables, and zero markup sales of consumables, increasing the efforts to cancel drug-based medical supplementation and promote the “three-medical linkage” (medical, medical insurance, and medical reform linkage).21–23 Regarding public hospital reform, the “three-medical linkage” is reflected in the cancellation of drug-based medical supplementation and comprehensive reforms in the management system, compensation mechanism, pricing mechanism, procurement mechanism, medical insurance payment system, personnel allocation, and regulatory mechanisms. In terms of establishing and improving the medical insurance system, the “three-medical linkage” synchronously raises medical insurance coverage and protection levels; in terms of medical circulation reform, the linkage reform aims to improve the essential drug system and drug supply guarantee. A series of measures taken by the Chinese government have, to a certain extent, reduced the share of personal health expenditures in total health costs, which is conducive to reducing the medical burden on individuals and promoting the rational allocation and use of health resources (Figure 1).
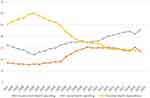 |
Figure 1 Composition of total health costs in China by year (%). China Health Care Statistical Yearbook, 1996–2022: http://www.nhc.gov.cn/mohwsbwstjxxzx/tjzxtjsj/tjsj_list.shtml. |
In the aspect of administrative institution reform, the newly established Medical Security Bureau plays an essential role in this round of medical reform. Its function is to coordinate multi-party resources, promote communication and cooperation among different departments, and strive to use the advantages of the social security fund’s scale to represent the demands of most patients within the affordable range of social security funds. This involves bargaining with medical service providers and, based on ensuring service quality and supply levels, reducing medical service social security expenditures as much as possible to alleviate the economic burden on patients.
The Real-Life Dilemma Facing the Implementation of China’s New Healthcare Reform
The distribution of medical and health resources is uneven. Facing the pressure of a population of 1.4 billion, China’s comprehensive health resources are insufficient, regional health resource allocation needs to be balanced, and primary community and rural health resources need to be more robust.24–27 Despite significant progress in hardware construction for underdeveloped areas in the western region and primary healthcare institutions with the support of governments at all levels, software construction still needs to be a bottleneck.28,29 The “first consultation at the grassroots level” has not been effectively implemented, and the “tiered diagnosis and treatment” has not achieved practical results.30 Primary health institutions’ development space and salary need to be more attractive, facing the dilemma of not retaining and attracting high-level medical talents.31
The burden of medical treatment for urban and rural residents is still relatively heavy. With the development of the economy and society and the improvement of health security levels, the demand for health services throughout the life cycle is increasing, and the demand for medical and health services for residents is becoming more diversified, with an increased demand for high-end and diversified medical services. However, the current structure of China’s medical and health service system still needs to be revised, and the burden of medical costs on residents is still heavy, and the costs are on a rising trend (Figure 2). Regarding overall development, China’s medical insurance system is not sound; the social security planning level is low, the financing level of medical insurance funds is significantly lower than the growth rate of medical expenses, and the sustainability of medical security is lacking. The reimbursement ratio of rural residents’ medical insurance is much lower than that of employees’ medical insurance, and the problem of the absence of fairness in medical security is still severe.32,33
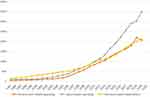 |
Figure 2 Total health expenditure in China by year (RMB billion). China Health Care Statistical Yearbook, 1996–2022: http://www.nhc.gov.cn/mohwsbwstjxxzx/tjzxtjsj/tjsj_list.shtml. |
In public hospitals, there has been insufficient public welfare. Prior to the new round of medical reform, the primary sources of income for public medical institutions were mainly composed of revenue from drug sales, medical services, and financial subsidies. After canceling drug and consumables sales markups, they can only rely on financial subsidies and medical service revenue to maintain daily operations. According to police regulations, financial subsidies can only make up for 80% of the revenue loss caused by the cancellation of markups, while the remaining 20% is to be internally absorbed by adjusting medical service prices and improving hospital management levels. For a long time, the level of refined and scientific management in Chinese medical service institutions has been relatively limited, and the vast majority of public hospitals cannot effectively reduce costs and compensate for losses by improving internal management in the short term.34,35 In this situation, they often rely on increasing medical service prices to compensate for operational losses. Although public medical institutions have a public welfare nature, their operating costs are also a considerable expenditure that cannot be ignored. If the long-term income is insufficient to cover the expenses, the supply of medical services will inevitably be significantly affected, which will harm citizens’ rights and interests.
Evolutionary Model Assumptions and Model Description
Game theory has been mainly applied in fields such as management, economics, and law for an extended period. In recent years, it has gradually been used in healthcare. Under the context of deepening medical and health system reforms, stakeholders such as the government, health departments, medical insurance departments, medical institutions, and patients differentiate into independent interest entities, aiming to maximize their interests in building their actions during the reform process. Stakeholders are important research subjects in healthcare reform, and those with vested interests may choose the strategy that is most advantageous to themselves when assessing various constraints in the new environment, even deliberately hiding some actions and information and deviating from the overall goal.36–39 Studies have found that increasing incentives and driving measures for doctors can effectively promote improving healthcare levels and enhancing medical services.40 As an essential role in healthcare reform, the medical insurance department’s payment subsidies can effectively stimulate medical demand while raising prices and inhibiting hospital competition.41 In promoting medical reform, the bargaining model can facilitate multilateral Nash negotiations, leading to a win-win situation for medical, medical insurance, and policyholders.42 In promoting hierarchical diagnosis and treatment and accessibility of medical services, China has continuously adjusted and balanced the interests of the government, medical institutions, and patients, hoping to achieve the best results.43 More and more countries use medical insurance payments as the primary means to guide and ensure the success of medical reforms from the rational payment of medical insurance funds.44–46
Model Description
Assumes that patients involved in the medical consumption process need to pay medical expenses (policy-complying medical costs ( )/noncomplying medical costs (
)/noncomplying medical costs ( )). The probability of patients (
)). The probability of patients ( ) seeking medical treatment is influenced by the severity of their illness (
) seeking medical treatment is influenced by the severity of their illness ( ). At the same time, Assumes that the patient’s game participant’s benefit is reflected in the perceived value (
). At the same time, Assumes that the patient’s game participant’s benefit is reflected in the perceived value ( ) of the patient receiving medical services. The total revenue of the medical institution can be divided into two parts: the reasonable medical treatment revenue (
) of the patient receiving medical services. The total revenue of the medical institution can be divided into two parts: the reasonable medical treatment revenue ( ) and the subsidy (
) and the subsidy ( ) provided by the government. The marginal cost (
) provided by the government. The marginal cost ( ) of the medical institution providing medical services, the revenue (
) of the medical institution providing medical services, the revenue ( ) from unreasonable medical treatment, and the penalty (F) imposed by the medical insurance regulatory department for unreasonable medical treatment. When the medical institution chooses “unreasonable medical treatment” and the patient “refuses treatment”, the medical insurance regulatory department will incur additional regulatory costs (
) from unreasonable medical treatment, and the penalty (F) imposed by the medical insurance regulatory department for unreasonable medical treatment. When the medical institution chooses “unreasonable medical treatment” and the patient “refuses treatment”, the medical insurance regulatory department will incur additional regulatory costs ( ). It will affect the reputation (
). It will affect the reputation ( ) of the medical insurance department. When the medical institution chooses “reasonable medical treatment” and the patient “accepts treatment”, the medical insurance fund pays the medical institution for reasonable medical treatment (
) of the medical insurance department. When the medical institution chooses “reasonable medical treatment” and the patient “accepts treatment”, the medical insurance fund pays the medical institution for reasonable medical treatment ( ) and rewards the medical institution for reasonable medical treatment (
) and rewards the medical institution for reasonable medical treatment ( ). All variables and their meanings used in the model are shown in Table 1.
). All variables and their meanings used in the model are shown in Table 1.
 |
Table 1 Variables and Variable Meanings |
In the new medical reform process, stakeholders include the medical insurance regulatory department, medical institutions, patients, and social groups. Their interests interact with each other, thus influencing each other’s behavior. For example, if healthcare institutions choose to implement the new healthcare reform policies and provide reasonable medical services, they can obtain profits from proper diagnoses and receive subsidies from the government. This will contribute to the stability of the healthcare insurance fund and enhance the reputation and incentives for healthcare institutions. Conversely, if healthcare institutions choose to provide unreasonable medical services, they may face penalties from the government and incur losses in the healthcare insurance fund, consequently affecting their profits and reputation. Similarly, the choices made by patients also impact healthcare institutions and the healthcare insurance fund. The severity of patients’ illnesses, the likelihood of seeking medical treatment, and the expenses incurred determine whether they seek medical care and the type of medical services they choose. If patients lean towards receiving reasonable medical services and making appropriate financial contributions, this will encourage healthcare institutions to provide better services and increase their profits. It will also ensure the effective utilization of the healthcare insurance fund. Therefore, examines three primary stakeholders, led by the government and centered around public hospitals, with a focus on patient interests, aiming to establish a mutually beneficial game mechanism and synergistically promote the goals of the new medical reform.
Evolutionary Model Assumptions
This paper’s three main game participants - medical insurance regulatory departments, medical institutions, and patients - seek to maximize their interests. They need to decide on their strategies based on the choices of strategies by the other two parties. This game is not a traditional, static, one-time game but a process where each individually boundedly rational entity within the three main game groups adjusts its strategy based on its own experience, eventually tending towards stability. To construct a game model, analyze the stability of the strategies and equilibrium points of all parties and the relationship of the impact of various factors, the following assumptions are made:
Assumption 1: Participating Entities. The regulation and rectification of unreasonable medical practices require the joint participation of government health regulatory departments, medical institutions, and patients. Constructs a tripartite evolutionary game model composed of medical insurance regulatory departments, medical institutions, and patients. Considering the complexity and inherent uncertainty in decision-making processes, each individual within the three entities exhibits a bounded rationality, meaning their decision-making abilities are limited by factors such as incomplete information, cognitive constraints, and rationality constraints. Under the premise of bounded rationality, all three parties engage in strategic choices, adapting their strategies based on their own experience and the choices made by others. Assumption 2: Decisions of Each Stakeholder. The three main entities, namely the medical insurance regulatory department, medical institutions, and patients, have two strategic options. Specifically, patients can choose to accept treatment or not, with probabilities Assumption 3: We assume a traditional principal-agent relationship between doctors and medical institutions, ie, the behavior of doctors aligns with that of medical institutions. The income from unreasonable medical treatments ( Assumption 4: Patients resist unreasonable medical practices by medical institutions. The degree of a patient’s illness ( Assumption 5: When a medical institution implements reasonable treatments, its income from reasonable treatments is Assumption 6: When a medical institution implements unreasonable medical practices and faces patient complaints, it incurs regulatory costs ( Assumption 7: Each stakeholder is a participant with bounded rationality. As different game participants aim to maximize their expected benefits under information asymmetry, the strategy selection gradually evolves and stabilizes at the optimal strategy, realizing collaborative governance. and
and  , respectively; medical institutions can choose to provide reasonable medical care or not, with probabilities
, respectively; medical institutions can choose to provide reasonable medical care or not, with probabilities  and
and  , respectively; the medical insurance regulatory department can choose to strictly or loosely regulate unreasonable medical practices, with respective probabilities
, respectively; the medical insurance regulatory department can choose to strictly or loosely regulate unreasonable medical practices, with respective probabilities  and
and  . Each individual within the three entities exhibits bounded rationality and adopts an imitative strategy, determining their strategy based on other individuals’ choices.
. Each individual within the three entities exhibits bounded rationality and adopts an imitative strategy, determining their strategy based on other individuals’ choices. ) is larger than that from proper treatments (
) is larger than that from proper treatments ( ). This assumption reflects the financial incentives for medical institutions to engage in reasonable or unreasonable practices.
). This assumption reflects the financial incentives for medical institutions to engage in reasonable or unreasonable practices. ), the perceived value of the medical service received by the patient (
), the perceived value of the medical service received by the patient ( ), and the reasonable/unreasonable treatment behavior of the medical institution together determine the probability (
), and the reasonable/unreasonable treatment behavior of the medical institution together determine the probability ( ) of a patient seeking medical care at the institution. This assumption captures the patient’s decision-making process based on their health condition, perceived value of the medical service, and the reputation and behavior of the medical institution.
) of a patient seeking medical care at the institution. This assumption captures the patient’s decision-making process based on their health condition, perceived value of the medical service, and the reputation and behavior of the medical institution. , and the government provides a financial subsidy (
, and the government provides a financial subsidy ( ). When a medical institution implements unreasonable treatments, its income from such treatments is M. Meanwhile, the medical insurance regulatory department will cease its financial subsidies to the institution and may impose a fine (
). When a medical institution implements unreasonable treatments, its income from such treatments is M. Meanwhile, the medical insurance regulatory department will cease its financial subsidies to the institution and may impose a fine ( ). Regardless of whether a medical institution chooses reasonable or unreasonable treatments, it will incur operational costs (
). Regardless of whether a medical institution chooses reasonable or unreasonable treatments, it will incur operational costs ( ). These assumptions highlight the financial implications for medical institutions based on their treatment choices and the regulatory actions of the medical insurance department.
). These assumptions highlight the financial implications for medical institutions based on their treatment choices and the regulatory actions of the medical insurance department. ) and losses to the medical insurance fund (
) and losses to the medical insurance fund ( ) caused by unreasonable treatments, thus diminishing the reputation (
) caused by unreasonable treatments, thus diminishing the reputation ( ) of the medical insurance department. This assumption captures the consequences of unreasonable practices for the reputation and financial stability of both the medical institution and the medical insurance department.
) of the medical insurance department. This assumption captures the consequences of unreasonable practices for the reputation and financial stability of both the medical institution and the medical insurance department.
Parameters are set according to the model assumptions, as shown in Table 1.
Evolutionary Model Construction and Analysis
Model Construction
In the game model, we denote  as the strategy where medical institutions provide appropriate treatment and
as the strategy where medical institutions provide appropriate treatment and  as the strategy of providing unreasonable treatment. The strategy where patients accept treatment is denoted as
as the strategy of providing unreasonable treatment. The strategy where patients accept treatment is denoted as  , and the strategy where patients refuse treatment is denoted as
, and the strategy where patients refuse treatment is denoted as  . The willingness of the medical insurance regulatory department to strictly regulate is denoted as
. The willingness of the medical insurance regulatory department to strictly regulate is denoted as  , and the willingness to loosely regulate is denoted as
, and the willingness to loosely regulate is denoted as  . The
. The  is mentioned above. Based on the above assumptions and variable definitions, the mixed strategy game payoff matrix of medical institutions, patients, and the medical insurance regulatory department is established, as shown in Table 2.
is mentioned above. Based on the above assumptions and variable definitions, the mixed strategy game payoff matrix of medical institutions, patients, and the medical insurance regulatory department is established, as shown in Table 2.
 |
Table 2 The Matrix of the Mixed Strategy Game Between Medical Institutions, Patients, and Health Insurance Regulators |
Game Model Analysis
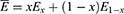
(1) Benefits of reasonable treatment by medical institutions:
Benefits of unreasonable medical treatment by medical institutions:
The average return for healthcare providers is:
The replication dynamics equation for the medical institution is
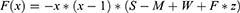
The benefits of patient refusal of treatment were
The average patient benefit was:
The replication dynamic equation for the patient is:
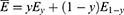
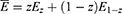
Gains from lax regulation by health insurance regulators:
The average benefit to health care regulators is:
The replication dynamic equation for the health insurance regulator is
Evolutionary System Equilibrium Analysis
The game dynamics among the health insurance regulatory department, medical institutions, and patients are subject to continuous evolution. To capture this dynamic evolution, we establish a tripartite game model and replicate the dynamic equation group. This allows us to calculate the equilibrium point of the tripartite game model. Importantly, the probabilities (x, y, and z) associated with the strategies chosen by the three parties are time-dependent, reflecting the evolving nature of the game process.
In order to analyze the stability of the system, we employ the principle of differential equation stability. Specifically, when all dynamic equations reach a state of equilibrium, the entire dynamic system tends towards stability. Thus, by establishing the dynamic equation group within the tripartite game model, we can determine the equilibrium point of the tripartite evolutionary game by solving the equations  . This approach considers the evolution of probabilities associated with the strategies chosen by the health insurance regulatory department, medical institutions, and patients. The continuous adaptation and adjustment of these probabilities over time contribute to the dynamic nature of the game process and influence the attainment of equilibrium.
. This approach considers the evolution of probabilities associated with the strategies chosen by the health insurance regulatory department, medical institutions, and patients. The continuous adaptation and adjustment of these probabilities over time contribute to the dynamic nature of the game process and influence the attainment of equilibrium.
According to Selton’s research findings, in a non-zero-sum game, if the condition of asymmetric information holds, the evolutionarily stable strategy is pure. Therefore, it is only necessary to discuss the asymptotic stability of the eight local equilibrium points  that satisfy
that satisfy  in the above formula.
in the above formula.
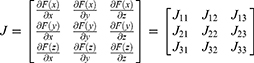
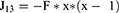
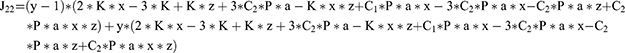
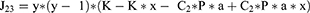
According to the replicator dynamics equations of the three parties, the Jacobian matrix of the tripartite evolutionary game system can be obtained as follows:
The Lyaploff method shows that stability can be judged in the stability analysis of differential systems based on the positive and negative eigenroots of the equilibrium point. When all the eigenvalues (roots) of the equilibrium point are negative, the point is an evolutionarily stable strategy (asymptotically stable point). The eight pure strategy points are brought into the Jacobian matrix in turn, and the eigenvalues of the equilibrium points are obtained, as shown in Table 3.
 |
Table 3 System Equilibrium Points and Characteristic Values |
As shown in Table 3, there may be two evolutionarily stable equilibrium points in the evolutionary game system: When  becomes an equilibrium point, it needs to satisfy the stability conditions
becomes an equilibrium point, it needs to satisfy the stability conditions  and
and  . When
. When  becomes an equilibrium point, it needs to satisfy the stability conditions
becomes an equilibrium point, it needs to satisfy the stability conditions  and
and  .
.
Numerical Simulation Analysis
Evolutionary Stabilization Strategy
For the equilibrium point  , when the conditions M < S + W and C1*P*a>K are met,
, when the conditions M < S + W and C1*P*a>K are met,  is an evolutionarily stable equilibrium point. To satisfy the above conditions, we assume
is an evolutionarily stable equilibrium point. To satisfy the above conditions, we assume  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  . As shown in Figure 3, as the evolution progresses, the probability of medical institutions choosing the “reasonable treatment” strategy continues to increase. In contrast, the probability of patients choosing the “refusal of treatment” strategy and the probability of health insurance regulatory departments choosing the “loose regulation” strategy continuously decrease. Therefore, the optimal strategies for medical institutions, patients, and health insurance regulatory departments are “reasonable treatment”, “refusal of treatment”, and “loose regulation”, respectively.
. As shown in Figure 3, as the evolution progresses, the probability of medical institutions choosing the “reasonable treatment” strategy continues to increase. In contrast, the probability of patients choosing the “refusal of treatment” strategy and the probability of health insurance regulatory departments choosing the “loose regulation” strategy continuously decrease. Therefore, the optimal strategies for medical institutions, patients, and health insurance regulatory departments are “reasonable treatment”, “refusal of treatment”, and “loose regulation”, respectively.
 |
Figure 3 Simulation of parameters of equilibrium point |
As shown in Figure 3, when the cost of unreasonable medical treatment for patients is higher than the sum of the excellent reputation benefits  of the health insurance regulatory department, the medical operation cost
of the health insurance regulatory department, the medical operation cost  of the medical institution, and the reasonable medical treatment income
of the medical institution, and the reasonable medical treatment income  of the medical institution, no matter what the initial strategies of the medical institutions and health insurance regulatory departments are, the final evolution result is
of the medical institution, no matter what the initial strategies of the medical institutions and health insurance regulatory departments are, the final evolution result is  . The medical institution will choose “unreasonable medical treatment”, and the health insurance regulatory department will choose “loose regulation”.
. The medical institution will choose “unreasonable medical treatment”, and the health insurance regulatory department will choose “loose regulation”.
For the equilibrium point  , when the conditions M < S + W and C1*P*a<K are met,
, when the conditions M < S + W and C1*P*a<K are met,  is an evolutionarily stable equilibrium point. To satisfy the above conditions, we assume
is an evolutionarily stable equilibrium point. To satisfy the above conditions, we assume  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  . As shown in Figure 4, as the probability of medical institutions choosing the “reasonable treatment” strategy and patients choosing the “acceptance of treatment” strategy increases, the probability of health insurance regulatory departments choosing “strict regulation” tends towards 0. This indicates that when the benefits of medical institutions choosing the “reasonable treatment” strategy are sufficiently high, medical institutions will be more inclined to implement a series of policies under the new medical reform. In this case, the results of health insurance regulatory departments choosing “strict regulation” and “loose regulation” are consistent, considering that “strict regulation” would increase regulatory costs. Therefore, the optimal strategy for the government is “loose regulation”. Consequently, the optimal strategies for medical institutions, patients, and the government are “reasonable treatment”, “acceptance of treatment”, and “loose regulation”, respectively.
. As shown in Figure 4, as the probability of medical institutions choosing the “reasonable treatment” strategy and patients choosing the “acceptance of treatment” strategy increases, the probability of health insurance regulatory departments choosing “strict regulation” tends towards 0. This indicates that when the benefits of medical institutions choosing the “reasonable treatment” strategy are sufficiently high, medical institutions will be more inclined to implement a series of policies under the new medical reform. In this case, the results of health insurance regulatory departments choosing “strict regulation” and “loose regulation” are consistent, considering that “strict regulation” would increase regulatory costs. Therefore, the optimal strategy for the government is “loose regulation”. Consequently, the optimal strategies for medical institutions, patients, and the government are “reasonable treatment”, “acceptance of treatment”, and “loose regulation”, respectively.
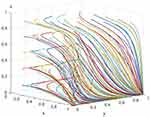 |
Figure 4 Simulation of parameters of equilibrium point |
Parameter Sensitivity Analysis
In China’s health reform context, the system’s stable equilibrium point  is the current optimal strategic choice. At equilibrium point
is the current optimal strategic choice. At equilibrium point  , the strategic combination of the three parties is “reasonable treatment”, “acceptance of treatment”, and “loose regulation”. Unreasonable medical behaviors of medical institutions could harm the interests of patients within the same system and reduce patients’ trust in health insurance regulatory departments. Only when medical institutions assume social responsibility and implement appropriate treatments can they effectively reduce patients’ treatment costs, enhance trust in the healthcare system, and the government’s strong regulation of the medical institutions’ treatment behaviors would be wasteful when medical institutions choose a reasonable treatment strategy. Therefore, the government could appropriately reduce regulation. Simultaneously, there may be a transition between equilibrium points
, the strategic combination of the three parties is “reasonable treatment”, “acceptance of treatment”, and “loose regulation”. Unreasonable medical behaviors of medical institutions could harm the interests of patients within the same system and reduce patients’ trust in health insurance regulatory departments. Only when medical institutions assume social responsibility and implement appropriate treatments can they effectively reduce patients’ treatment costs, enhance trust in the healthcare system, and the government’s strong regulation of the medical institutions’ treatment behaviors would be wasteful when medical institutions choose a reasonable treatment strategy. Therefore, the government could appropriately reduce regulation. Simultaneously, there may be a transition between equilibrium points  and
and  under certain conditions. When the game system is at equilibrium point
under certain conditions. When the game system is at equilibrium point  , it is not conducive to improving overall social welfare.
, it is not conducive to improving overall social welfare.
Thus, this article conducts a sensitivity analysis of some critical parameters in three possible equilibrium points to reveal better the significant influencing factors of each party’s strategic choice. These key parameters include government subsidies  for medical institutions, reasonable treatment income
for medical institutions, reasonable treatment income  , unreasonable medical treatment income WMMM, government fines
, unreasonable medical treatment income WMMM, government fines  , government rectification costs
, government rectification costs  , and government regulatory costs
, and government regulatory costs  . It should be emphasized that when analyzing the sensitivity of one of the above parameters, the values of other parameters are the same as the simulation values of equilibrium point
. It should be emphasized that when analyzing the sensitivity of one of the above parameters, the values of other parameters are the same as the simulation values of equilibrium point  .
.
The Impact of Patients’ Unreasonable Treatment Expenditure on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , assuming
, assuming  the simulation evolution scenario is shown in Figure 5. The results show that when patients choose medical treatment strategies, medical institutions issue unreasonable prescriptions for patients’ conditions, leading to an increase in patients’ unreasonable expenditure. As the patients’ unreasonable treatment expenditure increases, patients will likely choose the “refusal of treatment” strategy. The patients’ unreasonable treatment expenditure has almost no influence on medical institutions and government decisions.
the simulation evolution scenario is shown in Figure 5. The results show that when patients choose medical treatment strategies, medical institutions issue unreasonable prescriptions for patients’ conditions, leading to an increase in patients’ unreasonable expenditure. As the patients’ unreasonable treatment expenditure increases, patients will likely choose the “refusal of treatment” strategy. The patients’ unreasonable treatment expenditure has almost no influence on medical institutions and government decisions.
 |
Figure 5 Sensitivity analysis of patients’ unreasonable treatment expenditure. |
The Impact of Patients’ Policy-Complying Medical Costs on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , assuming
, assuming  , the simulation evolution scenario is shown in Figure 6. The results show that as the patients’ reasonable treatment expenditure increases, the probability of patients choosing the “acceptance of treatment” strategy will increase. The patients’ reasonable treatment expenditure has almost no influence on medical institutions’ and government decisions.
, the simulation evolution scenario is shown in Figure 6. The results show that as the patients’ reasonable treatment expenditure increases, the probability of patients choosing the “acceptance of treatment” strategy will increase. The patients’ reasonable treatment expenditure has almost no influence on medical institutions’ and government decisions.
 |
Figure 6 Sensitivity analysis of patients’ policy-complying medical costs. |
The Impact of Medical Institutions’ Reasonable Treatment Revenue on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , assuming
, assuming  , the simulation evolution scenario is shown in Figure 7. The results indicate that when medical institutions conduct medical practices within the scope of reasonable treatment, patients’ reasonable treatment costs will increase, but not infinitely, eventually stabilizing, which is beneficial for maintaining patients’ interests in reasonable treatment. Meanwhile, due to strict regulation by the health insurance regulatory department, the revenue from reasonable treatment by medical institutions will only grow for a while. The health insurance regulatory department allocates corresponding health insurance funds because the medical institutions comply with appropriate treatment.
, the simulation evolution scenario is shown in Figure 7. The results indicate that when medical institutions conduct medical practices within the scope of reasonable treatment, patients’ reasonable treatment costs will increase, but not infinitely, eventually stabilizing, which is beneficial for maintaining patients’ interests in reasonable treatment. Meanwhile, due to strict regulation by the health insurance regulatory department, the revenue from reasonable treatment by medical institutions will only grow for a while. The health insurance regulatory department allocates corresponding health insurance funds because the medical institutions comply with appropriate treatment.
 |
Figure 7 Sensitivity analysis of the revenue cost of reasonable treatment in medical institutions. |
Figure 7 shows that as the total revenue from reasonable treatment by medical institutions increases, the probability of medical institutions choosing the “reasonable treatment” strategy continuously increases. This suggests that the total revenue from appropriate treatment positively promotes medical institutions implementing reasonable treatment measures. Figure 7 indicates that as the revenue from reasonable treatment by medical institutions increases, patients are more inclined to choose the “acceptance of treatment” strategy, but the convergence speed keeps decreasing. Figure 7 demonstrates that with the continuous increase in the revenue from reasonable treatment by medical institutions, the health insurance regulatory department will be more inclined to adopt loose supervision. However, the convergence speed keeps decreasing, indicating that the health insurance regulatory department will still maintain a certain level of regulation.
The Impact of Medical Institutions’ Unreasonable Treatment Revenue on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , assuming
, assuming  , the simulation evolution scenario is shown in Figure 8. The results show that when medical institutions opt for unreasonable treatment, due to the strict supervision by the health insurance regulatory department, the increase in patients’ medical costs is slowed; similarly, the revenue from unreasonable treatment by medical institutions will not always increase. With the health insurance regulatory department opting for strict supervision strategies, the revenue growth rate from unreasonable treatment by medical institutions slows down; at this point, the health insurance regulatory department needs to increase its regulatory cost expenditure.
, the simulation evolution scenario is shown in Figure 8. The results show that when medical institutions opt for unreasonable treatment, due to the strict supervision by the health insurance regulatory department, the increase in patients’ medical costs is slowed; similarly, the revenue from unreasonable treatment by medical institutions will not always increase. With the health insurance regulatory department opting for strict supervision strategies, the revenue growth rate from unreasonable treatment by medical institutions slows down; at this point, the health insurance regulatory department needs to increase its regulatory cost expenditure.
 |
Figure 8 Sensitivity analysis of unreasonable treatment in medical institutions. |
Figure 8 shows that when the revenue from unreasonable treatment by medical institutions increases, the probability of medical institutions implementing appropriate treatment decreases. In contrast, the probability of patients choosing the “refuse treatment” strategy increases. Medical institutions tend to choose the “reasonable treatment” strategy when the revenue from unreasonable treatment is low. Once the revenue from the unreasonable treatment exceeds a threshold, medical institutions change their strategy and adopt an “unreasonable treatment” approach. As the revenue from medical institutions’ unreasonable treatment increases, the probability of patients choosing the “refuse treatment” strategy also increases. With the increased revenue from medical institutions’ unreasonable treatment, the probability of the government choosing “strict regulation” becomes more considerable.
The Influence of Medical Insurance Penalties for Unreasonable Treatment by Medical Institutions on the Evolutionary Game of the Three Parties
Under the equilibrium condition of point  , we assume
, we assume  . The simulation evolution situation is shown in Figure 9. The results indicate that as the severity of medical insurance penalties for unreasonable treatment by medical institutions increases, the medical institutions will choose the “reasonable treatment” strategy in line with the intensification of medical insurance supervision, and the probability of patients choosing to “accept treatment” also continuously increases. Moreover, as the severity of medical insurance penalties for unreasonable treatment by medical institutions increases, the medical insurance regulatory department will opt for “strict supervision”, but the convergence speed keeps decreasing.
. The simulation evolution situation is shown in Figure 9. The results indicate that as the severity of medical insurance penalties for unreasonable treatment by medical institutions increases, the medical institutions will choose the “reasonable treatment” strategy in line with the intensification of medical insurance supervision, and the probability of patients choosing to “accept treatment” also continuously increases. Moreover, as the severity of medical insurance penalties for unreasonable treatment by medical institutions increases, the medical insurance regulatory department will opt for “strict supervision”, but the convergence speed keeps decreasing.
 |
Figure 9 Sensitivity analysis of medical insurance to penalties for unreasonable treatment by medical institutions. |
The Influence of the Supervision Costs of Medical Insurance Regulatory Departments on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , we assume
, we assume  . The simulation evolution situation is depicted in Figure 10. The results demonstrate that when supervision costs maintain a low growth rate, the likelihood of medical institutions choosing the “reasonable treatment” strategy somewhat decreases. However, once a certain threshold is exceeded, the probability of medical institutions choosing the “reasonable treatment” strategy remains nearly unchanged. When supervision costs maintain a low growth rate, the probability of patients opting for the “refuse treatment” strategy increases somewhat. However, once a certain threshold is exceeded, the probability of patients choosing the “refuse treatment” strategy remains nearly constant. The higher the supervision costs, the more likely the medical insurance regulatory department will choose the “relaxed supervision” strategy, although the convergence speed continually decreases.
. The simulation evolution situation is depicted in Figure 10. The results demonstrate that when supervision costs maintain a low growth rate, the likelihood of medical institutions choosing the “reasonable treatment” strategy somewhat decreases. However, once a certain threshold is exceeded, the probability of medical institutions choosing the “reasonable treatment” strategy remains nearly unchanged. When supervision costs maintain a low growth rate, the probability of patients opting for the “refuse treatment” strategy increases somewhat. However, once a certain threshold is exceeded, the probability of patients choosing the “refuse treatment” strategy remains nearly constant. The higher the supervision costs, the more likely the medical insurance regulatory department will choose the “relaxed supervision” strategy, although the convergence speed continually decreases.
 |
Figure 10 Sensitivity analysis of regulatory costs for health insurance regulators. |
The Influence of Normal Allocation of Medical Insurance Funds During Reasonable Treatment by Medical Institutions on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , we assume values of
, we assume values of  . The simulation evolution situation is illustrated in Figure 11. The results indicate that the average allocation of medical insurance funds does not affect the strategic choices of medical institutions, patients, and the medical insurance regulatory department.
. The simulation evolution situation is illustrated in Figure 11. The results indicate that the average allocation of medical insurance funds does not affect the strategic choices of medical institutions, patients, and the medical insurance regulatory department.
 |
Figure 11 Sensitivity analysis of the normal allocation of medical insurance funds in case of reasonable treatment by medical institutions. |
The Influence of the Loss of Health Insurance Fund Due to Unreasonable Treatment on the Evolutionary Game of the Three Parties
Under the equilibrium conditions of point  , we assume values of
, we assume values of  . The simulation evolution situation is illustrated in Figure 12. The results indicate that the loss of health insurance funds due to unreasonable treatment has no effect on the strategic choices of medical institutions, patients and health insurance regulators.
. The simulation evolution situation is illustrated in Figure 12. The results indicate that the loss of health insurance funds due to unreasonable treatment has no effect on the strategic choices of medical institutions, patients and health insurance regulators.
 |
Figure 12 Sensitivity analysis of the loss of health insurance fund due to unreasonable treatment. |
Results
In China’s new round of healthcare reform, a game mechanism has been formed with medical insurance regulatory departments, medical institutions, and patients as the main interest entities. Based on the perspective of bounded rationality, Establishes an evolutionary game model of collaborative governance among the medical insurance regulatory departments, medical institutions, and patients, explores the strategy evolution equilibrium of different subjects, and the impact of various factors on the strategic evolution of the three parties. It also analyzes the intrinsic logic of the medical insurance regulatory department to exert its maximum advantage and force medical institutions to implement reasonable diagnostic and treatment measures through economic incentives or penalties for unreasonable medical practices and the intrinsic conditions for achieving collaborative governance. Under this theoretical framework, further empirical testing of the theoretical results with actual data is the next research direction.
From the perspective of promoting overall social welfare, our study identifies that the equilibrium point, characterized by “reasonable diagnosis and treatment by medical institutions”, “patients accepting treatment”, and “relaxed supervision by medical insurance regulatory departments”, maximizes the interests of all game participants. Our findings indicate that medical institutions’ implementation of reasonable diagnostic and treatment strategies has gained recognition and support from patients, who willingly choose to receive treatment and pay for related medical expenses. Additionally, the simplified regulatory strategy employed by the medical insurance regulatory department effectively reduces regulatory costs and ensures the stable operation of the medical insurance fund. These coordinated strategies enable medical institutions, patients, and the medical insurance regulatory department to optimize their interests. Overall, our results demonstrate that the game evolution under the new healthcare reform policy can achieve a balanced state, where medical institutions provide high-quality, reasonable diagnostic and treatment services, patients actively seek treatment and contribute to the cost, and the medical insurance regulatory department adopts a streamlined regulatory approach to incentivize proper practices by medical institutions. These outcomes contribute to improving the quality of medical services, optimizing resource allocation, and fostering the sustainable development of the entire healthcare system.
Discussion
The game among medical insurance regulatory departments, medical institutions, and patients as stakeholders is critical to driving successful reform. To achieve successful reform, all three parties must cooperate and work together actively.
Firstly, medical insurance regulatory departments should regulate the medical service behavior of medical institutions and guide the rational allocation of medical resources through payment system reforms. The ultimate goal of the medical insurance payment system reform is to provide appropriate incentives for healthcare service providers so that they can offer suitable services according to patients’ needs, aligning the interests of healthcare service providers with the health level of the general public. Implementing DRG/DIP payment system reform is crucial in incentivizing public hospitals to voluntarily standardize medical service behaviors, ensuring diagnostic and treatment levels and service quality, and achieving cost control. The reform of the payment system will also further improve patients’ medical treatment quality, reduce the burden of medical expenses on the public, enhance people’s well-being, compel hospitals to actively improve management and operational efficiency, and enhance diagnostic and treatment levels and service quality. By avoiding the waste of medical resources and unreasonable medical practices, patients can enjoy better diagnostic and treatment services and experiences, allowing them to “spend less money” while still receiving quality care.
Secondly, medical insurance regulatory departments should increase operational subsidies for medical institutions and strengthen penalties. Insufficient government investment in healthcare units has led to the slow development of healthcare, forcing hospitals to seek survival and development by passing the burden of inadequate funding onto the public. This has created the current passive situation of expensive and demanding access to medical care, resulting in the gradual deterioration of doctor-patient relationships and deepening conflicts. Therefore, increasing investment in medical institutions is one of the channels to address this issue.
The “Opinions on Strengthening the Performance Assessment of Tertiary Public Hospitals” issued by the General Office of the State Council in 2019 explicitly states that localities should establish a mechanism for sharing performance assessment information and results among departments, forming a joint effort among departments and strengthening the application of performance assessment results. The government helps hospitals standardize diagnostic and treatment behaviors and avoid unreasonable medical practices by regulating public hospitals’ medical behaviors, such as drug costs, doctors’ prescriptions, average inpatient costs, average outpatient costs, and examination fees. The government further improves supervision and regulatory mechanisms to comprehensively supervise the operational management process of public hospitals and timely correct deviations in their behaviors. This ensures the public welfare nature of public hospitals and their operational efficiency.
Meanwhile, medical insurance regulatory departments should reduce regulatory costs. Investigations show that large-scale equipment inspections, antibiotic use, implantable medical devices, and intensive care have become significant areas of unreasonable medical practices. Due to the particularity and concealment of medical services, it is difficult to determine whether a treatment is unreasonable after it has been implemented, or if it can be achieved, it may incur excessively high costs. Effectively curbing unreasonable medical practices is critical to the success of the reform. Regulatory authorities should take the following measures to contain unreasonable medical practices and reduce regulatory costs:
- Establish a coordinated platform by establishing a joint conference system to supervise medical insurance funds. The joint conference should be led by the municipal government, with the office in the medical insurance department, and include departments such as health and wellness, drug supervision, auditing, finance, and public security as member units.
- Promote information sharing and strengthen the application of results among various departments, forming seamless integration of medical and pharmaceutical-related information centered around the medical insurance entity.
- Ensure smooth channels for patients to express their interests and demands.
In today’s service-oriented government, the quality of essential medical services also needs to be evaluated and receive feedback from patients. In the future, during the pricing process of essential medical services, patients’ opinions should be collected extensively through standardized information platforms, allowing their demands to be expressed smoothly, given attention, and promptly responded to.
Lastly, it introduces third-party forces to strengthen medical insurance supervision further. To improve social governance capabilities, it is essential to perfect the institutional mechanism and establish a social governance system where the government is responsible, society collaborates, the public participates, and the rule of law is guaranteed. This will enhance the level of socialization, legalization, intelligence, and specialization in governance. In this context, medical insurance departments should explore leveraging their advantages, introduce third-party forces, and strengthen medical insurance supervision. This includes entrusting intermediary agencies to strengthen medical insurance supervision, entrusting insurance companies to enhance special supervision, and periodically inviting personnel from relevant government departments, members of the Chinese People’s Political Consultative Conference, insured persons, and media reporters to conduct in-depth inspections of medical institutions and medical insurance handling agencies, implementing social supervision on medical service practices and the use of medical insurance funds.
Limitations of the Study: It is important to acknowledge the limitations of our study. The model employed in our research represents a simplified abstraction of the complex dynamics involved in the healthcare system. While it provides valuable insights into the promotion of balanced interest among medical insurance regulatory departments, medical institutions, and patients, it may not fully capture the intricacies and variations inherent in the real-world context. For example, we did not explicitly consider factors such as the differences between the central and local governments, variations among different hospitals, or other contextual nuances that could potentially influence the outcomes. Future research should explore these factors to provide a more comprehensive understanding of the reform process and the dynamics of interest balance among stakeholders.
Conclusion
After more than a decade of exploration and practice, China’s new healthcare reform has achieved remarkable accomplishments, contributing “Chinese wisdom” to the global development of healthcare. However, China still needs to work on issues such as imbalanced and insufficient healthcare development, obstacles in the institutional mechanism, a relatively high burden on residents seeking medical care, and weak medical supervision forces. These problems urgently need to be fundamentally resolved through deepening reforms. Given this, this article constructs a tripartite evolutionary game model composed of medical insurance regulatory authorities, medical institutions, and patients, analyzing each party’s optimal strategy selection, the stability of the game system’s equilibrium strategy combination, and the influence relationships among various factors. The effectiveness of the results is verified through simulation analysis. Without empirical materials and data, this article employs game thinking to enhance its explanatory power, hoping to provoke widespread reflection and discussion among scholars on good governance in China’s healthcare field. Although China’s unique national conditions and healthcare system have characteristics, the related concepts, and methods can still provide valuable insights for healthcare reforms in many countries.
Disclosure
The authors report no conflicts of interest in this work.
References
1. CPC Central Committee and State Council. Opinions on deepening the reform of the medical and health system [EB/OL]; 2023. Available from: http://www.gov.cn/jrzg/2009-04/06/content_1278721.htm.
2. Chen J, Lin Z, Li L, et al. Ten years of China’s new healthcare reform: a longitudinal study on changes in health resources. BMC Public Health. 2021;21(1):2272. doi:10.1186/s12889-021-12248-9
3. Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–1204. doi:10.1016/S0140-6736(19)32136-1
4. Tan X, Liu X, Shao H. Healthy China 2030: a vision for health care. Value Health Reg Issues. 2017;12:112–114. doi:10.1016/j.vhri.2017.04.001
5. National Health Commission of the People’s Republic of China. China health statistics yearbook [EB/OL]; 2023. Available from: http://www.nhc.gov.cn/mohwsbwstjxxzx/tjzxtjcbw/tjsj_list.shtml.
6. NHS.2021 National statistical bulletin on the development of the health security service[EB/OL]; 2023. Available from: http://www.nhsa.gov.cn/art/2022/6/8/art_7_8276.html.
7. Zhang Y, Wang Q, Jiang T, et al. Equity and efficiency of primary health care resource allocation in mainland China. Int J Equity Health. 2018;17:1–12.
8. Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi:10.1016/S0140-6736(20)30122-7
9. Zhang T, Xu Y, Ren J, et al. Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health. 2017;16(1):1–8. doi:10.1186/s12939-017-0543-9
10. Mei J, Kirkpatrick I. Public hospital reforms in China: towards a model of new public management? Int J Pub Sect Manag. 2019;32(4):352–366. doi:10.1108/IJPSM-03-2018-0063
11. Wang L, Wang Z, Ma Q, et al. The development and reform of public health in China from 1949 to 2019. Global Health. 2019;15(1):1–21. doi:10.1186/s12992-019-0486-6
12. Xu J, Jian W, Zhu K, et al. Reforming public hospital financing in China: progress and challenges. BMJ. 2019;365. doi:10.1136/bmj.l4015
13. Ta Y, Zhu Y, Fu H. Trends in access to health services, financial protection and satisfaction between 2010 and 2016: has China achieved the goals of its health system reform? Soc Sci Med. 2020;245:112715. doi:10.1016/j.socscimed.2019.112715
14. Ratigan K. Riding the tiger of performance legitimacy? Chinese villagers’ satisfaction with state healthcare provision. Int Political Sci Rev. 2022;43(2):259–278. doi:10.1177/0192512120927482
15. The Central Committee of the Communist Party of China and the State Council. Opinions on deepening the reform of the medical and health system [EB/OL]; 2023. Available from: https://www.gov.cn/gongbao/content/2009/content_1284372.htm.
16. Chen Z. Launch of the health-care reform plan in China. Lancet. 2009;373(9672):1322–1324. doi:10.1016/S0140-6736(09)60753-4
17. Li L, Fu H. China’s health care system reform: progress and prospects. Int J Health Plann Manage. 2017;32(3):240–253. doi:10.1002/hpm.2424
18. Agrawal R, Prabakaran S. Big data in digital healthcare: lessons learnt and recommendations for general practice. Heredity. 2020;124(4):525–534. doi:10.1038/s41437-020-0303-2
19. Li D. 5G and intelligence medicine—how the next generation of wireless technology will reconstruct healthcare? Precis Clin Med. 2019;2(4):205–208. doi:10.1093/pcmedi/pbz020
20. Li B, Ma X, Yu Y, et al. Improving the drug supply security system. In: Tutorial for Outline of the Healthy China 2030 Plan. Springer; 2020:131–139.
21. Liu W, Hsu C, Liu T, et al. Systematic review of the effect of a zero-markup policy for essential drugs on healthcare costs and utilization in China, 2015–2021. Front Med. 2021;8:618046. doi:10.3389/fmed.2021.618046
22. Shi X, Zhu D, Man X, et al. “The biggest reform to China’s health system”: did the zero-markup drug policy achieve its goal at traditional Chinese medicines county hospitals? Health Policy Plan. 2019;34(7):483–491. doi:10.1093/heapol/czz053
23. Du J, Xie J, Qian Y, et al. Impact of China’s zero mark-up drug policy on drug cost of NCDs’ outpatients: an interrupted time series analysis. BMC Health Serv Res. 2021;21(1):1–13. doi:10.1186/s12913-021-06414-3
24. Yu Q, Yin W, Huang D, et al. Trend and equity of general practitioners’ allocation in China based on the data from 2012–2017. Hum Resour Health. 2021;19:1–16. doi:10.1186/s12960-021-00561-8
25. Meng Q, Mills A, Wang L, et al. What can we learn from China’s health system reform? BMJ. 2019;365. doi:10.1136/bmj.l2349
26. Lu C, Zhang Z, Lan X. Impact of China’s referral reform on the equity and spatial accessibility of healthcare resources: a case study of Beijing. Soc Sci Med. 2019;235:112386. doi:10.1016/j.socscimed.2019.112386
27. Wu H, Ba N, Ren S, et al. The impact of internet development on the health of Chinese residents: transmission mechanisms and empirical tests. Socioecon Plann Sci. 2022;81:101178. doi:10.1016/j.seps.2021.101178
28. Xu W, Pan Z, Lu S, et al. Regional heterogeneity of application and effect of telemedicine in the primary care centres in rural China. Int J Environ Res Public Health. 2020;17(12):4531. doi:10.3390/ijerph17124531
29. Du Y, Zhou Q, Cheng W, et al. Factors influencing adoption and use of telemedicine services in rural areas of China: Mixed Methods Study. JMIR Public Health Surveill. 2022;8(12):e40771. doi:10.2196/40771
30. Xiao Y, Wu X, Chen J, et al. Challenges in establishing a graded diagnosis and treatment system in China. Fam Pract. 2022;39(1):214–216. doi:10.1093/fampra/cmab089
31. Zhang Z, Shi G, Li L, et al. Job satisfaction among primary care physicians in western China. BMC Fam Pract. 2020;21(1):1–10. doi:10.1186/s12875-020-01292-w
32. Chen S, Chen Y, Feng Z, et al. Barriers of effective health insurance coverage for rural-to-urban migrant workers in China: a systematic review and policy gap analysis. BMC Public Health. 2020;20(1):1–16. doi:10.1186/s12889-020-8448-8
33. Huang X, Wu B. Impact of urban-rural health insurance integration on health care: evidence from rural China. China Econ Rev. 2020;64:101543. doi:10.1016/j.chieco.2020.101543
34. Xu C, Jin J, Song J, et al. Application of refined management in prevention and control of the coronavirus disease 2019 epidemic in non-isolated areas of a general hospital. Int J Nurs Sci. 2020;7(2):143–147. doi:10.1016/j.ijnss.2020.04.003
35. Kong X, Ai B, Kong Y, et al. Artificial intelligence: a key to relieve China’s insufficient and unequally-distributed medical resources. Am J Transl Res. 2019;11(5):2632.
36. Haidari AM, Zaidi S, Gul R. Prospects for the sustainability of delivering the basic package of health services in Afghanistan: a stakeholder analysis. East Mediterr Health J. 2014;20(5):300–308. doi:10.26719/2014.20.5.300
37. Abiiro GA, McIntyre D. Universal financial protection through National Health Insurance: a stakeholder analysis of the proposed one-time premium payment policy in Ghana. Health Policy Plan. 2013;28(3):263–278. doi:10.1093/heapol/czs059
38. Blanchet NJ, Fox AM. Prospective political analysis for policy design: enhancing the political viability of single-payer health reform in Vermont. Health Policy. 2013;111(1):78–85. doi:10.1016/j.healthpol.2013.02.012
39. Ashraf S, Moore C, Gupta V, et al. Overview of a multi-stakeholder dialogue around shared services for health: the digital health opportunity in Bangladesh. Health Res Policy Syst. 2015;13:74. doi:10.1186/s12961-015-0063-2
40. Blake A, Carroll BT. Game theory and strategy in medical training. Med Educ. 2016;50(11):1094–1106. doi:10.1111/medu.13116
41. Wang C, Nie PY. Effects of asymmetric medical insurance subsidy on hospitals competition under non-price regulation. Int J Equity Health. 2016;15(1):184. doi:10.1186/s12939-016-0468-8
42. Ehlert A, Wein T, Zweifel P. Overcoming resistance against managed care - insights from a bargaining model. Health Econ Rev. 2017;7(1):19. doi:10.1186/s13561-017-0156-4
43. Tao C, Chen X, Zheng W, et al. How to promote the hierarchical diagnosis and treatment system: a tripartite evolutionary game theory perspective. Front Psychol. 2022;13:1081562. doi:10.3389/fpsyg.2022.1081562
44. Tummers LG, Van de Walle S. Explaining health care professionals’ resistance to implement Diagnosis Related Groups: (No) benefits for society, patients and professionals. Health Policy. 2012;108(2–3):158–166. doi:10.1016/j.healthpol.2012.08.024
45. Or Z. Implementation of DRG Payment in France: issues and recent developments. Health Policy. 2014;117(2):146–150. doi:10.1016/j.healthpol.2014.05.006
46. Rajtar M. Health care reform and Diagnosis Related Groups in Germany: the mediating role of Hospital Liaison Committees for Jehovah’s Witnesses. Soc Sci Med. 2016;166:57–65. doi:10.1016/j.socscimed.2016.08.016
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.