Back to Journals » Infection and Drug Resistance » Volume 13
Household Transmission of COVID-19: A Cross-Sectional Study
Authors Dutta S , Kaur RJ , Bhardwaj P , Charan J , Bist SKS, Detha MD, Kanchan T, Sharma P , Misra S
Received 7 October 2020
Accepted for publication 13 November 2020
Published 23 December 2020 Volume 2020:13 Pages 4637—4642
DOI https://doi.org/10.2147/IDR.S285446
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Siddhartha Dutta,1 Rimple Jeet Kaur,2 Pankaj Bhardwaj,3 Jaykaran Charan,1 Sunil Kumar Singh Bist,4 Mohan Dan Detha,5 Tanuj Kanchan,6 Praveen Sharma,7 Sanjeev Misra8
1Department of Pharmacology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India; 2Department of Pharmacology, S. N. Medical College, Jodhpur, Rajasthan, India; 3Department of Community and Family Medicine, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India; 4Medical and Health, Jodhpur Zone and COVID 19 Nodal Officer, Jodhpur District, Rajasthan, India; 5Block CMHO, Luni, Jodhpur and Medical Officer in Charge, COVID Care Centre, Boranada, Jodhpur, Rajasthan, India; 6Department of Forensic Medicine, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India; 7Department of Biochemistry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India; 8All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Correspondence: Jaykaran Charan
Department of Pharmacology, AIIMS, Jodhpur, Rajasthan, India
Tel +919825219196
Email [email protected]
Introduction: The COVID-19 pandemic has brought the entire world to a standstill. The disease is rapidly transmitting in the community. Imposed lockdowns due to the COVID-19 pandemic have effectively delayed the transmission in the community but the transmissibility in households needs to be explored. The aim of this study was to estimate the household transmission of COVID-19 and assess the factors affecting transmission.
Patients and Methods: A cross-sectional study where the data were collected from a single isolation center, was conducted. Patients were contacted by phone. Information regarding number of COVID-19-positive cases in the family, their demographic details, along with number of rooms in their household was collected.
Results: A total of 369 families of COVID-19-positive patients were contacted. Nineteen families with a single member were excluded. Out of 350 families with a total 2126 members, 480 (22.5%) were COVID-19 positive. Mean age was 30.12 years (± 14.39) and majority of them were males (68.9%). Majority of the cases (67.3%) were in the age group (19– 49 years). Mean rooms per person were 0.51± 0.20 (0.14 to 1.50). Mild negative correlation was seen between number of positive COVID-19 cases and rooms per person (r= − 0.138, p=0.008) while moderate negative correlation with number of family members and proportion of family members being COVID-19 positive (r= − 0.542, p≤ 0.0001).
Conclusion: One in four family members got infected with COVID-19, they were majority males and in the working age group. Negative correlation of positive cases with number of family members and mild negative correlation between rooms per person and proportion of family member affected indicates some other factors may be responsible for household transmission than these factors.
Keywords: COVID-19, household transmission, SARS-CoV-2, coronavirus, isolation
Plain Language Summary
- COVID–19 transmission in the population led to the pandemic getting worse with increased morbidity and mortality. To prevent the virus from spreading, lockdown was ensured round the world with a plan to cut down community transmission but led to transmission to household contacts
- This study aimed to assess the transmission of COVID–19 in household contacts and the factors influencing its transmission. The patients or their contacts were telephonically contacted and were questioned for assessing the same
- COVID–19 did not affect all family members equally and only one fourth of the family members were infected. Males in the families were more susceptible to COVID–19 as compared to females and children less than ten years were less susceptible as compared older ones
- Non-availability of adequate space in the home for each member has a minor role to play in the infection of COVID–19 and these findings point towards various concealed or unidentified factors and natural immunity or resistance to the virus which might be playing role in determining the rate of household transmission of COVID–19
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus which has led to the current pandemic of coronavirus disease 2019 (COVID-19).1 It started with few unknown cases of pneumonia in December 2019 from Wuhan, Hubei Province, China and then swiftly began to spread to several other countries following which the World Health Organization (WHO) declared it an emergency, later on 11th March 2020 it was declared a pandemic.2 Globally, there have been 27,032,617 confirmed cases and 881,464 deaths related to COVID-19 as of 7 September 2020, as reported by WHO and currently, India stands second in the highest number of cases.3 The clinical presentation of COVID-19 is highly variable and it spreads primarily through droplets when a COVID-19-positive person coughs, sneezes, or speaks.4,5 In the absence of definitive treatment of COVID-19, preventive measures seem to play a crucial role in minimizing the chances of being infected by the disease and curb the disease from spreading in the population.5 To curb its spread, governments across the globe have imposed lockdowns and stay-at-home orders where the basic idea was to minimize the transmission in the community by reducing the mobility of the public. Mobility is an essential part of everyday life and the imposed lockdowns have decreased the mobility from 46.3% to 73.4% to various outdoor places, and increased the residential mobility by 26.32%.6 The mobility restrictions subsequently led to an increase in the time dwelling at home and a plausible increase in household transmission of COVID-19. The WHO-China Joint Mission has stated that the majority of the human-to-human transmission of COVID-19 has been found in families.7
The current recommendation is to avoid close contact with COVID-19-positive patients and maintain six feet of distance with the person who is ill or with the other members of the family.5 Practicing the recommended distancing norms seems difficult in a household as family members are likely to interact with each other regularly while having food, watching television or sharing bathrooms and quite impossible if they have a low average number of rooms per family member which will again increase the probability of getting infected if any of the family members gets sick.8 The airborne nature of its spread makes it difficult to contain within a household. In support of the fact, evidence shows that almost 70% of transmission of SARS-CoV-2 was attributed to contact within households when adequate community control measures were in place.9
In low and middle-income countries (LMICs), where a quality healthcare service for the entire population has been a challenge, overcrowding and inadequate housing per person can enhance the risk of transmission among close contacts in households, supposedly leading to decreased effectiveness of lockdown and stay-at-home orders.10,11 The fecal–oral transmission of SARS-CoV-2 due to enteric shedding further complicates the issue in these settings where a large part of the population lack access to clean water and sanitation facilities.11,12 Household transmission of infection seems to be a crucial component in the spread of the disease as it has already played a dominant role in previous pandemics of swine flu (H1N1) and severe acute respiratory syndrome (SARS).13–15 Literature shows that secondary transmission or infection of SARS-CoV-2 in household contacts ranges from 4.6% to 49.56%.16–20 WHO states that overcrowding or inadequate shelter are major contributors to the transmission of diseases like acute respiratory infections which can result in outbreaks or epidemic.21
Literature search has revealed only two studies from India determining the secondary attack rate (SAR) among COVID-19 patients. The study done by ICMR COVID Study Group reported SAR with a national average of 6% with the highest SAR in Chandigarh (11.5%) and Maharashtra (10.6%).22 A study conducted by Laxminarayan et al in two south Indian states reported that the per-contact risk of infection was 9.0% (7.5–10.5%) in the household.11 A lot of uncertainty remains about household transmission and factors that may affect it and more effort is needed to explore it through research. Hence, we planned this study with an aim to estimate household transmission of COVID-19 and to see the relationship between some factors which may affect this transmission.
Patients and Methods
The current study was conducted in an isolation facility in Jodhpur, Rajasthan. As per the state health department guidelines, COVID-19 patients who were asymptomatic and were not having appropriate facilities in the home, were kept in an institutional isolation center, under the supervision of general physicians. Patients with symptoms, or with co-morbidities, or aged >60 years, were transferred to the tertiary care center for better monitoring and treatment. The information about the patients admitted from 14th May 2020 to 7th July 2020 was collected from the data kept in the isolation facility. The contact number and details of the patients were extracted from the available data and they were telephonically contacted for the survey. Initially, the questionnaire tool was tested in a few cases and required modifications were made based on the survey experience of the pilot cases. One member from each of these families or households was telephonically contacted to know if any other member was found to be positive for COVID-19. They were asked about the number of family members, family members positive for COVID-19, details about the positive members of their family including age/gender, and the number of rooms present at their home. All the people in a family or a group who live and dwell together in a house was taken as a household. Verbal consent was taken from the participant regarding his/her free will to participate in the study, before the survey and responses were recorded into the proforma.
Statistical Analysis
The data was entered into the Microsoft Excel sheet and was reported in the form of frequency and percentages. The person’s correlation was used for the inferential statistics. Analysis was done with the help of Statistical Package for the Social Sciences for Windows, version 21 (SPSS Inc., Chicago, IL, USA).
Ethical Approval
The study was approved by the Institutional Ethics Committee, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India with the certificate reference number AIIMS/IEC/2020-21/3076. The survey participants were informed about the purpose of the study and it was conducted in accordance with the Declaration of Helsinki.
Results
We could contact families of 369 COVID-19-positive patients who were admitted to the isolation center. Households with at least two persons or more were included. Nineteen families which had only a single member were excluded. All the families that were contacted confirmed that all members of their family had been tested for COVID-19. There were a total of 2126 members in these 350 families of which 480 (22.5%) were COVID-19 positive. Out of these 480 patients, 68.9% were males and 31.1% were females. The mean age of the patients was 30.12 years with a standard deviation of 14.39. Around one-third (28.3%) of these patients were in young adulthood (19–29 years). The majority of affected children were teenaged (13–18 years), while 67.3% of COVID-19-positive cases were in the age group (19–49 years). Sociodemographic details are illustrated in Table 1. Mean rooms per person in these households were 0.51 with the standard deviation of 0.20 and a range of 0.14 to 1.50. The mean percentage of positive cases from all family members was 26% with a range of 5% to 100%. There was a mild negative correlation between the number of positive COVID-19 cases and rooms per person (r= −0.138, p=0.008) [Figure 1] while a moderate negative correlation was seen with the number of family members and proportion of family members (positive COVID-19 cases in family/total members in the family) being infected by COVID-19 (r= −0.542, p≤0.0001) [Figure 2].
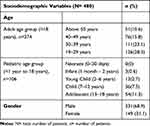 |
Table 1 Demographic Details of the COVID-19-Positive Cases |
 |
Figure 1 Correlation Between Rooms Per Person and Positive Cases. |
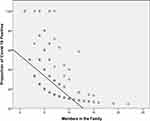 |
Figure 2 Correlation Between Total Family Members and Proportion of Positive Cases. |
Discussion
The current study tries to provide some insights into the transmission of COVID-19 in Indian households. It was found that around one-fourth of total family members becomes infected.
This study shows that 22.5% of the family members were affected by COVID-19. As per the data reported by ICMR COVID Study Group, 25.3% of patients of COVID-19 were asymptomatic family members of direct and high-risk contacts of a laboratory-confirmed case.22 Laxminarayan et al reported a SAR of 9% (7.5–10.5%) in the two south Indian states of Tamil Nadu and Andhra Pradesh.11 A study by Beale et al on seasonal coronavirus infections in English households reported that 9.3% (5.5–15.4) of the cases were in household members who were exposed and believed to be acquired by virtue of household transmission.23 Rosenberg et al reported a comparatively higher number based on a study conducted in New York, USA reported that initial COVID-19 prevalence was 57% in the household.18
This study reports majority of the COVID-19-positive cases were males (68.9%). The finding was similar to other studies conducted in India by ICMR COVID Study Group (64.5%), Laxminarayan et al (62–63%), Shah et al (67.6%) and Mahajan et al (76%).11,22,24,25 The Indian data on gender is contrary to the published data by other countries where both males and females had an almost similar risk of COVID-19 positivity.17,18,20
The current study shows the probability of infection was less in the pediatric age group as compared to adults, and children below 10–12 years were less susceptible to COVID-19 as compared to the older children. The study finding was similar to other studies conducted in India and abroad.11,17,19,20,22,25 The majority of the cases in this study were in the working-age group (19–49 years) which was also similar to the previously reported studies.11,22,25
This study reports a low mean room per person data. As per international standards, the data quoted by the “Organization for Economic Co-operation and Development (OECD)”, the average home contains 1.8 rooms per person.26 In India, as per the “State of Housing In India-A Statistical Compendium 2013” by the Government of India, Ministry of Housing and Urban Poverty Alleviation, National Buildings Organization, the majority (73%) of the population in India dwells in two or less than two rooms per household hence the study results are comparable to the national data.27 The mild negative correlation between the number of positive COVID-19 cases and rooms per person denotes that even though overcrowding should have increased the number of cases there can be multiple other associated factors governing the probability of secondary infection in the households. The negative correlation between the number of family members and the proportion of family members being infected by COVID-19 again points towards the same fact.
The study finding can be supported by the similar findings in the systematic review of various studies across the world which states that a large proportion (50–95%) of persons in contact with a COVID-19-positive case did not develop an infection, which points toward a potential role of inborn resistance to disease or natural immunity.19
The other possible reason for having less transmission in the family may be due to the strict adherence of isolation guidelines released by the Ministry of Health & Family Welfare, Government of India. The guidelines clearly mentioned that as soon as the result of RT-PCR of a person is received as positive, the person is either admitted to the isolation facility or if the adequate rooms are available in the house, maybe allowed home isolation. The person in the home isolation is under the strict monitoring of the state health department.
Conclusion
The current study supports the fact that besides natural immunity and unknown factors, the efficient implementation and strict adherence to the guidelines proved effective in preventing the transmission of COVID-19 in the household.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or nonprofit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Andersen KG, Rambaut A, Lipkin WI, et al. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450–452. doi:10.1038/s41591-020-0820-9
2. Coronavirus (COVID-19) events as they happen. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
3. WHO Coronavirus Disease (COVID-19) Dashboard. Available from: https://covid19.who.int.
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
5. CDC. Coronavirus Disease 2019 (COVID-19) – prevention & treatment. centers for disease control and prevention; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.
6. Saha J, Barman B, Chouhan P. Lockdown for COVID-19 and its impact on community mobility in India: an analysis of the COVID-19 community mobility reports, 2020. Child Youth Serv Rev. 2020;116:105160. doi:10.1016/j.childyouth.2020.105160
7. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
8. Haroon S, Chandan JS, Middleton J, Cheng KK. Covid-19: breaking the chain of household transmission. BMJ. 2020;370:m3181. doi:10.1136/bmj.m3181
9. Shen M, Peng Z, Guo Y, et al. Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households. Int J Infect Dis. 2020;96:503–505. doi:10.1016/j.ijid.2020.05.019
10. Leclerc QJ, Fuller NM, Knight LE. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5:83. doi:10.12688/wellcomeopenres.15889.2
11. Laxminarayan R, Wahl B, Dudala SR, et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Medrxiv[Preprint]. 2020:20153643. doi:10.1101/2020.07.14.20153643.
12. Hindson J. COVID-19: faecal-oral transmission? Nat Rev Gastroenterol Hepatol. 2020;17(5):259. doi:10.1038/s41575-020-0295-
13. Lau LL, Nishiura H, Kelly H, Ip DK, Leung GM, Cowling BJ. Household transmission of 2009 pandemic influenza A (H1N1): a systematic review and meta-analysis. Epidemiology. 2012;23(4):531–542. doi:10.1097/EDE.0b013e31825588b8
14. Tsang TK, Lau LLH, Cauchemez S, Cowling BJ. Household transmission of influenza virus. Trends Microbiol. 2016;24(2):123–133. doi:10.1016/j.tim.2015.10.012
15. Lau JT, Lau M, Kim JH, Tsui HY, Tsang T, Wong TW. Probable secondary infections in households of SARS patients in Hong Kong. Emerg Infect Dis. 2004;10(2):235–243. doi:10.3201/eid1002.030626
16. Wu J, Huang Y, Tu C, et al. Household Transmission of SARS-CoV-2, Zhuhai, China, 2020. Clin Infect Dis. 2020:ciaa557. doi:10.1093/cid/ciaa557.
17. Li W, Zhang B, Lu J, et al. The characteristics of household transmission of COVID-19. Clin Infect Dis. 2020:ciaa450. doi:10.1093/cid/ciaa450.
18. Rosenberg ES, Dufort EM, Blog DS, et al. New York State Coronavirus 2019 Response Team. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State-March 2020. Clin Infect Dis. 2020:ciaa549. doi:10.1093/cid/ciaa549.
19. Shah K, Saxena D, Mavalankar D. Secondary attack rate of COVID-19 in household contacts: systematic review. QJM. 2020;hcaa232. doi:10.1093/qjmed/hcaa232
20. Madewell ZJ, Yang Y, Longini IM, Halloran ME, Dean NE. Household transmission of SARS-CoV-2: a systematic review and meta-analysis of secondary attack rate. medRxiv. 2020;
21. World Health Organization. What are the health risks related to overcrowding? Available from: http://www.who.int/water_sanitation_health/emergencies/qa/emergencies_qa9/en/Accessed.
22. Abraham P, Aggarwal N, Babu G, ICMR COVID Study Group. Laboratory surveillance for SARS-CoV-2 in India: performance of testing & descriptive epidemiology of detected COVID-19, January 22 - April 30, 2020. Indian J Med Res. 2020;151(5):424–437. doi:10.4103/ijmr.IJMR_1896_20
23. Beale S, Lewer D, Aldridge RW, et al. Household transmission of seasonal coronavirus infections: results from the Flu Watch cohort study [version 1; peer review: awaiting peer review]. Wellcome Open Res. 2020;19(5):145. doi:10.12688/wellcomeopenres.16055.1
24. Shah K, Desai N, Saxena D, Mavalankar D, Mishra U, Patel GC. Household secondary attack rate in Gandhinagar district of Gujarat state from Western India. Medrxiv[Preprint]. 2020. doi:10.1101/2020.09.03.20187336
25. Mahajan P, Kaushal J. Epidemic Trend of COVID-19 transmission in india during lockdown-1 phase. J Community Health. 2020;23:1–10. doi:10.1007/s10900-020-00863-3
26. Organisation for economic co-operation and development. better life index: housing. Available from: http://www.oecdbetterlifeindex.org/topics/housing/#:~:text=In%20the%20OECD%2C%20the%20average%20home%20contains%201.8%20rooms%20per%20person.
27. State of Housing in India a Statistical Compendium −2013. Government of India, Ministry of Housing and Urban poverty alleviation national buildings organisation. Available from: http://mohua.gov.in/upload/uploadfiles/files/Housing_in_India_Compendium_English_Version2.pdf.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
