Back to Journals » Patient Preference and Adherence » Volume 17
Household Contact Tuberculosis Screening Adherence and Associated Factors Among Pulmonary Tuberculosis Patients on Follow-Up at Health Facilities in Shashamane Town, Southeast Ethiopia
Authors Naga Mamo A , Furi Gilo R, Fikadu Tesema A , Fetene Worku N, Teshome Kenea T, Kebede Dibisa D, Adisu Dagafa Y, Dube L
Received 31 March 2023
Accepted for publication 19 July 2023
Published 28 July 2023 Volume 2023:17 Pages 1867—1879
DOI https://doi.org/10.2147/PPA.S411685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Qizhi (Cathy) Yao
Adisu Naga Mamo,1 Robdu Furi Gilo,2,* Ashetu Fikadu Tesema,3,* Negash Fetene Worku,4 Tadese Teshome Kenea,5 Dinka Kebede Dibisa,6 Yonas Adisu Dagafa,7 Lamessa Dube8,*
1Department of Public Health Emergency Management, Kelem Wallaga Zonal Health Office, Dambi Dollo, Oromia, Ethiopia; 2Department of Pediatrics, Shala District Health Office, Shashamane, Oromia, Ethiopia; 3Department of Medical Laboratory Sciences, Institute of Health Science, Dambi Dollo University, Dambi Dollo, Oromia, Ethiopia; 4Department of Diseases Prevention and Control, Yaya Gulale District Health Office, Fiche, Oromia, Ethiopia; 5Department of Public Health Emergency Management, Sire Hospital, Nekemte, Oromia, Ethiopia; 6Department of Diseases Prevention and Control, Setema District Health Office, Jimma, Oromia, Ethiopia; 7Department of Medical Laboratory Sciences, Institute of Health Science, Wallaga University, Nekemte, Oromia, Ethiopia; 8Department of Epidemiology, Institute of Health Science, Jimma University, Jimma, Oromia, Ethiopia
*These authors contributed equally to this work
Correspondence: Adisu Naga Mamo, Tel +251917712305, Email [email protected]
Background: The greatest risk of getting tuberculosis (TB) infection is contact with patients who have pulmonary tuberculosis (PTB). The World Health Organization (WHO) strongly recommends tuberculosis screening for all household contacts of PTB patients. However, there is no information on household contact screening adherence among PTB patients in Shashamane town.
Methods: A facility-based mixed-method cross-sectional study was conducted from July 1 to November 30, 2021 among consecutively selected 392 PTB patients and 23 purposely selected key informants. Data were collected using a pre-tested interviewer administered questionnaire and leading questions. Data analysis was made using SPSS version 25 and in-depth interview information was analyzed based on thematic areas. Bivariable followed by multivariable logistic regression with 95% CI were conducted. P-value< 0.05 was considered to identify statistically significant factors.
Results: The overall adherence to household contact screening (HHCS) was 44.4% (95% CI: 39.3, 49.1). Having under fifteen years of contact (AOR=2.386, 95% CI: 1.44, 3.96), diploma and above education status (AOR=3.43, 95% CI: 1.286, 9.15), good knowledge (AOR=2.999, 95% CI: 1.79, 5.03), favorable attitude (AOR=2.409, 95% CI: 1.45, 4.02), getting health education (AOR=3.287, 95% CI: 1.92, 5.63) and smear positive type of PTB (AOR=2.156, 95% CI: 1.28, 3.62) were factors significantly associated with HHCS adherence. Workload, facility readiness and care provide commitments were also identified from qualitative data.
Conclusion and Recommendation: HHCS adherence in our study was sub-optimal referenced to WHO and national recommendations that all household contact should be screened. Having age less than fifteen years contact, education status, knowledge, attitude, receiving health education and type of pulmonary tuberculosis were factors associated with adherence. We recommend increasing community awareness of TB, providing health education TB patients and their families, strengthening positive attitudes toward HHC screening and strengthening the commitment of health professionals to screen for HHCs.
Keywords: adherence, household, contact, screening, pulmonary tuberculosis
Background
Tuberculosis (TB) is an air-borne infectious disease caused by the bacillus Mycobacterium tuberculosis, which is spread when people who are sick with TB expel bacteria into the air.1 The agent typically affects the lungs, causing pulmonary type of TB, but can affect other sites causing extra pulmonary type.2 It is among the top ten infectious diseases and leading cause of mortality worldwide from single agent Mycobacterium tuberculosis, ranging above HIV/AIDS.3
The principal risk factor for Mycobacterium tuberculosis is exposure to someone with active disease. Particularly, household contacts or other close contacts of index active disease are the most exposed individuals.4 Household contacts (HHCs) of pulmonary tuberculosis are at increased risk of being infected with active disease, with the initial bacillary burden predicting risk.1
Contact screening is used to identify undiagnosed tuberculosis infection among contacts of the index cases.5,6 Screening of HHCs of pulmonary tuberculosis is one strategy of detecting and treating TB patients earlier among a high risk population.7,8 Early identification of tuberculosis in contacts also benefits their communities by reducing tuberculosis transmission.4 Moreover, contact investigation is a key component of a Global End TB strategy for finding missing patients to fill the notification gap more rapidly and work toward elimination targets.9,10 Thus, screening of all age contacts of pulmonary tuberculosis is strongly recommended by the WHO to intensify active case finding.7,11 Household contact screening through index case invitation is the recommended option particularly in resource limited settings.9,10 In order to carry out this recommendation, health care workers are requested to inform patients to bring their contacts for screening.12,13
Counseling the index case about the purpose and importance of contact screening, and the ways it will be conducted is the starting point for contact enumeration, and contact's invitation through the index case followed.10 Index patient adherence to all these activities is a critical component of a household contact investigation strategy that ends up bringing contact/s for screening.9
However, globally 4.2 million patients with tuberculosis (TB) were not notified of national TB programs in 2020 due to COVID-19 impact, restricted accessibility, undeveloped health reporting systems and linkages between the public and private sectors, lack of human resources and inadequate adherence to household contact screening both by patients and health care providers.3,14 Additionally, 67% (867,000) of children younger than 5 years who were household contacts of smear pulmonary tuberculosis were not screened and administered TB preventative therapy in 2019.15,16
In 2019, 38 million people in 20 high-burden countries lived in a household with someone who had developed incident pulmonary tuberculosis.17 However, 43% of contacts of pulmonary tuberculosis cases remained unscreened for tuberculosis.18 The WHO’s End Tuberculosis Strategy’s by 2020 as of 2015 base line was challenged by lack of timely diagnosis, inadequate treatment of active TB cases, poor implementation of contact screening and negligence in treating latent tuberculosis infection (LTBI) to prevent it from progressing to active disease.19,20
Despite low contact screening, the studies in TB high burden countries revealed the prevalence of TB among contacts was ten times higher than the general population’s.14 The prevalence of TB among PTB contacts was estimated to be 6.9% in a study in South Delhi, India.21 Another observational study conducted in Afghanistan discovered that the estimated national incidence rate for tuberculosis was ten times lower than the actual number of cases among contacts.22 In addition to Ethiopia being one of 30 TB high burden countries for TB and TB/HIV burden with incidence of 140/100,000 for all forms of TB in 2019,16 a third (29%) of anticipated yearly incident cases are not being reported to the national TB prevention and control program (missing cases), which is a major challenge in achieving a 90% reduction of incident cases by 2035 as a baseline to 2015.23,24
All countries including Ethiopia have adopted WHO policies on contact investigation included in their National TB Program (NTP).25 However, the majority of them either do not implement it or do so with inadequate standards.11,14 In most settings, index patient adherence to bringing their HHCs for screening remained sub-optimal due to fear of stigma, poor awareness, costs of travel, perceived attitude, health system and clinical profile of index case related factors.10 Patients’ adherence to HHC TB screening 169 (52%) in Thailand was linked to perceived vulnerability, lower perceived barriers, higher intention to bring contacts, distance from facility’s and TB knowledge.26 Low household contact screening practice in Nigeria of 23.6% (348) was associated with knowledge and attitude related factors.27
Despite the high prevalence of TB among contacts,28,29 all age household contact screening which was conducted through index case invitation remained sub-optimal in Ethiopia.30,31 A few studies revealed index case adherence to HHCS to be low; only 33.7% in Amhara region32 and 47.5% in Gondar.33 These were linked to socio-demographic, health care facility-related factors, clinical-related factors and some individual factors.32–34
Despite HHCS is the main case finding strategy among household contacts of PTB,5 no study was so far undertaken in the West Arsi Zone to check whether this program was implemented properly. Few studies in Ethiopia used a single study design and did not consider contacts factors and health care provider’s perspectives on factors affecting household contact TB screening adherence.32,33 Hence, the aim of this study is to determine the magnitude of household contact tuberculosis screening adherence and related factors among adult pulmonary tuberculosis patients in Shashamane town health facilities, Southeast Ethiopia.
Methods and Materials
Study Setting
The study was conducted in Shashamane Town, one of the towns in Oromia region state. The town is the capital of West Arsi Zone located about 250 km south of Addis Ababa. According to zonal health office data: two government hospitals, four governmental health centers, one private hospital and six private medium clinics were delivering TB diagnosis and care. Additionally, there was one DR-TB treatment initiating center (TIC) in this area. According to the town’s DHIS2 data, a total of 667 all forms TB cases visited the town’s health facilities during the 2020/21 fiscal year with incidence of 166/100,000, which is higher than the estimated national incidence of the particular year. During our study period a total of 444 adults with pulmonary tuberculosis attended the health facilities on anti-TB regimen follow-up.
The Study Design and Period
A facility-based cross-sectional quantitative study design supplemented with qualitative inquiry was conducted from July 1 to November 30, 2021.
Source Population
The source populations for quantitative study were all pulmonary TB patients who were on anti-TB treatment follow-up. Key informants from contacts of PTB index cases and health care provider’s currently offering TB diagnosis and treatment service were considered for qualitative approach.
Study Population
All selected adult pulmonary tuberculosis patients who had household contact, on anti-TB regimen follow-up at health facilities of Shashamane town and found during the study period were the study population. Purposely selected key informants from contacts and health care providers were included for qualitative approach.
Inclusion Criteria
All adult pulmonary tuberculosis patients who had household contacts and on anti-TB treatment follow up at health facilities in Shashamane were included.
Exclusion Criteria
Adult patients with pulmonary tuberculosis who had household contacts and were critically ill and unable to communicate were excluded. Patients who initiated treatment during the day of data collection were excluded since he/she may not have information about bringing household contact for screening during entry day.
Sample Size and Sampling Procedure
Sample Size
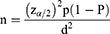
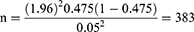
The sample size for the quantitative approach was calculated using a single population proportion formula considering 47.5% proportion of HHCS adherence taken from the study conducted in Gondar town, Amhara region,33 assuming 95% confidence interval (CI), 5% degree of precision and 10% non-response rate:
The final calculated sample size with 10% non-response rate was 421 for the quantitative approach.
For the qualitative approach, 23 key informants from both groups (five health professionals and 18 contacts) were interviewed. The sample size for the qualitative study was determined based on the saturation of ideas.
Sampling Techniques
All illegible consecutive patients who visited the health facilities for their regular follow-up during the study period were recruited until the desired sample size (421) was achieved. As per national TB guidelines, household contacts are enumerated by index cases and recorded on the tuberculosis unit register.5 During every day of data collection, review of these routinely recorded data was conducted to select eligible participants.
For the qualitative approach, purposively selected key informants consisting of health professionals and contacts gave their views on the key informant interview guide.
Data Collection Tools and Procedure
For the quantitative part a structured pretested questionnaire contained five parts; socio-demographic factors, individual factors, health care system related factors, practice and clinical related factors adapted by reviewing different literatures were used.26,32–35 Data were collected through face to face interview by six trained clinical nurses and the procedure was supervised by two trained health officers. Additionally, medical records of the respondents were reviewed to collect clinical related data.
Qualitative data were collected by in-depth interview of key informants (KI) using leading questions to explore barriers and initiators related to household contact tuberculosis screening practice. Audio record or strict note was taken during the interview. Contacts were interviewed for initiators of their attendance and also for the main barrier. Additionally, health professionals were interviewed for how the program was feasible in their facility, what challenges the program implementation and their experience on patient adherence to household contact screening.
Data Quality Control
An adapted data collection tool was translated to local language (Afaan Oromoo and Amharic) and translated back to English language to check its consistency. The tool was pre-tested among 5% of the sample size in one health center which was outside the study area. The reliability statistics for attitude and satisfaction items with Cronbach’s alpha were 72.1% and 75.6% during pretest respectively.
For qualitative data, data quality was ensured by enhancing the trustworthiness and rigor of the study findings.
Data Processing and Analysis
Data were entered and cleaned using Epidata version 4.6 and transported to SPSS version 25 software for analysis. The descriptive statistics were computed to summarize data initially. Binary logistic regression analysis was carried out at two levels. Variables with P-values of <0.25 in bivariate logistic regression analysis were exported into multivariable logistic regression analysis. Finally, the adjusted odds ratio (AOR) with 95% confidence intervals and P-value<0.05 was considered in multivariable logistic regression to determine the associated factors of TB household contact screening adherence. Multicollinearity was detected using variance inflation factors (VIF<10) among predictor variables and no variables were removed. The final model goodness of fit was checked by Hosmer and Lemeshow goodness of fit at P-value 0.80.
Qualitative data analysis was carried out using thematic framework analysis.36 Data collected through IDI was analyzed by open coding with a thematic analysis approach using ATLAS.ti 7 software. Direct verbatim and results from the coding and categorization were used to develop the narrative, triangulated and synthesized with the quantitative results. In our qualitative analysis most of the barriers stated by the respondents were facilitators of adherence to household contact screening in case of their absence.
Measurements
Pulmonary Tuberculosis (PTB)
Refers to any bacteriologically confirmed or clinically diagnosed case of TB involving the lung parenchyma or the tracheobronchial tree.37
Household Contact
A person who shared the same enclosed living space for one or more nights or extended periods during the day with the index case during the 3 months before commencement of the current treatment episode.13
Household Contact Tuberculosis Screening Adherence
Is when the index pulmonary TB patient brought at least one household contact to the TB unit for tuberculosis screening purpose, otherwise non-adherent.32,33
Knowledge
Knowledge score of respondent about TB ranged from 0 to 21 depending on whether the respondent answered the questions or not. The total score was computed and scores of below 80% was considered as not knowledgeable (poor knowledge) while scores equal to 80% and greater represented knowledgeable (good knowledge).33
Waiting Time
Time taken to get service after the arrival of the health facility.33
Satisfaction to the Service
Satisfaction to the TB service was measured by a total of 14 Likert's scale items. The response range of the items was from 14 to 70 for each respondent. Thus, the overall score of satisfaction was computed using 75% as the cut-off-point. Respondents with the score greater than or equal to 75% were classified as satisfied, otherwise unsatisfied.33,35
Attitude Toward Contact Screening
Attitude was measured on 5-point Likert's scale items with a total response range from 6 to 30. A composite attitude variable was created from the scores using the mean as the cut-off-point (favorable attitude=above mean, unfavorable attitude=below mean) upon checking normality of the scores.
Index Case
The initially registered case of new or recurrent TB in a person of any age in specific household. On whom a contact investigation is centered but is not necessarily the source.13
Ethical Consideration
The study was conducted in accordance with the Helsinki Declaration. The ethical clearance of this study was obtained from Institutional Review Board (IRB) of the Institute of Health, Jimma University, Ethiopia. Copies of the IRB and letter of support written from department of epidemiology of JU were submitted to Shashamane town health office in order to obtain a letter of permission used to contact health facilities. Considering the study subjects who cannot read and write and the awareness that the study was harmless to study subjects, the Institutional Ethical review board approved informed verbal consent for each respondent and their confidentiality was assured. The informed consent also included publication of anonymized responses.
Results
Socio-Demographic Characteristics of the Respondents
A total of 392 participants completed our study, yielding a 93.1% response rate. Of these participants 214 (54.6%) were male, whereas 178 (45.5%) were female. The mean age of respondents was 33.3±12.67SD. The mean number of household contacts index patients have were 5.63±1.61 (Table 1).
 |
Table 1 Socio-Demographic Related Factors for Household Contact Screening Adherence at Health Facilities in Shashamane Town, Southeast Ethiopia, November 2021 (n=392) |
The qualitative findings were analyzed under the four major themes of health worker related factors, health facility related factors, socio-economic and cultural related factors, and index and contact related knowledge and attitude.
Individual Related Characteristics
About 261 (66.6%) of the participants know that tuberculosis is caused by bacteria or germ and 374 (95.4%) of the participants know cough greater than two weeks could be one symptom of tuberculosis. The majority 368 (93.8%) of the participants know that tuberculosis is transmitted through air droplet from patient to another by cough, sneeze and during talking and 89% of the study participants know being in close contact with a TB patient is the risk factor for contracting the infection. Generally, half 196 (50%) of the respondents had good knowledge about tuberculosis. Nearly half of respondents 200 (51%) had favorable attitude regarding perceived household contact susceptibility, perceived contact screening benefit and perceived social discrimination. With respect to TB service satisfaction, greater than half of the respondents 217 (55.4%) were satisfied with the service and the majority 218 (55.6%) of the study participants visit the facility on foot (Table 2).
 |
Table 2 Individuals Related Factors for Household Contact Screening Adherence at Health Facilities in Shashamane Town, Southeast Ethiopia, November 2021 (n=392) |
Health System, Health Care Provider and Disease Profile Related Characteristics
More than half 239 (61%) of participants reported it takes above twenty minutes to visit the health facility and 244 (62.2%) reported it takes below thirty minutes to get service after visiting the facility. Two hundred and forty-eight (63.3%) participants reported that they received health education about household contact screening from their care provider (Table 3). The following statement from the in-depth interview indicates the absence of monitoring and evaluation for household contact screening by health facilities:
Our facility does not routinely monitor and follow household contacts of index TB cases for screening … (35-year-old, male, TB focal)
The interview also identified another logistic and supply related factor that affects institutional readiness:
Previously, contact screening was done using a specific contact screening registration book. However, we haven’t got this registration book for the past two years. (40-year-old, male, Health center TB Focal)
Most of the key informants reported difficulty of bringing all household contacts to the diagnostic health facilities which was worsened by transportation costs and contacts busy at work:
Despite the advantages of household contact screening, most index cases complain about transportation costs and contacts are too busy at work to come. (35-year-old, female, Hospital TB Focal)
Proportion of Adherence to Household Contact Screening
The overall adherence to household contact screening was 44.4% (95% CI: 39.3, 49.1). The mean number of household contacts brought among adhered participants were 1.8±0.8SD.
“The majority of index cases fail to bring their contacts for screening as required.” Even they didn’t enumerate the exact household contacts they have. They always say “I will bring” but they didn’t. “I’m busy, I forgot, or nobody has a cough”, they always say. These were the difficulties we faced when dealing with index cases. (29-year-old, male, TB Focal)
Factors Associated with Household Contact TB Screening Adherence
The bivariate logistic regression factors like age, marital status, education level, occupation, having under fifteen years of contact, having good knowledge, favorable attitude, satisfaction to TB unit service, receiving health education on contact screening, smear positive type of pulmonary tuberculosis, distance from facility less than 20 minute and service waiting time less than 30 minute were factors significantly associated with adherence to household contact screening and considered for further multivariable logistic analysis (Table 4).
 |
Table 4 Multivariable Logistic Regression Analysis of Factors for Household Contact Screening Adherence, in Health Facilities of Shashamane Town, Southeast Ethiopia, 2021 (n=392) |
Accordingly, in multivariable logistic regression six variables were significantly associated with household contact screening adherence; those who having under fifteen years of contact were adhered to HHCS twice more likely than those do not (AOR=2.386, 95% CI: 1.44, 3.96).
The participants with education status diploma and above adhered greater than three times more likely when compared to those with none formal education (AOR=3.43, 95% CI: 1.286, 9.15). The odds of adherence to household screening were two times higher among participants who had favorable attitude toward contact screening than those who had unfavorable attitude toward contact screening (AOR=2.409, 95% CI: 1.45, 4.02). The expression from in-depth interview states:
… It’s not because of a curse! I would never ashamed of that my family had TB. So, as soon as we were informed screening, I want to nearby health facility for screenings with all of my families. (40-year-old, male, Head of household contact)
The odds of adherence to household screening were three times higher among participants who had good knowledge about tuberculosis than those who had poor knowledge about tuberculosis (AOR=2.999, 95% CI: 1.79, 5.03). This was supported by the word of contacts that had not been screened because they misunderstood about transmission and diagnosis of tuberculosis:
… No one in our family has a cough or any other symptoms. So, what are we screening for? Is it possible to be diagnosed with TB without having any symptoms (50-year-old, male, household contact)
… Is TB longer being infectious after got treatment? I don’t think so! (26-year-old, male, household contact)
Odds of adherence to household screening were greater than three times among participants who have received health education on tuberculosis contact screening than those have not received health education (AOR=3.287, 95% CI: 1.92, 5.63).
I wouldn’t work full time for a month. When I am assigned to a night duty program, I am given the day off. As a result, there was a time when I couldn’t access some index cases to counsel on bringing all ages of household contacts at TB treatment program introduction. (Focal TB, 29-year-old, male)
Respondents with smear positive (drug resistance/susceptible) adhered greater than two times (AOR=2.156, 95% CI: 1.28, 3.62) more likely when compared with drug susceptible pulmonary negative. The expression from in-depth interview of health care providers revealed there was prioritization of household contact screening due to workload:
I know that all age household contacts of pulmonary tuberculosis should be screened. However, due to the workload and overwhelming of the laboratory our main focus is less than fifteen years contacts of smear positive pulmonary tuberculosis since they are targeted for tuberculosis preventive therapy (TPT). (35-year-old, female, hospital focal person)
Discussion
Household contact screening of pulmonary tuberculosis is a recommended active TB case finding strategy for high-risk groups.7,8 In Ethiopia, targeted and differentiated approach of household contact screening is the main case finding strategy and approach.5 Thus, this study assessed the level and factors affecting adherence to household contact screening.
In this study it is identified that the magnitude of household contact screening adherence was 44.4% (95% CI: 39.3, 49.1). This finding is lower when compared to the adherence level 52% reported in Bangkok, Thailand26 and another study conducted in southeast Ethiopia by secondary document review reported 55.7% of index cases brought at least one household for screening.38 Our finding was coherent with another study conducted in the northern part of Ethiopia that reported 47% of adherence level.33 However, this finding exceeds the report of household contact screening practice reported in Pune, India of 36.2% (29/80) and another from Southeast Nigeria reported only about 23.6% of the respondents brought contacts for screening and another household contact screening adherence level reported 33.7% in northern Ethiopia.27,32,39
The possible discrepancy could be due to difference in socio-demographic and socio-economic, cultural difference, difference in time of the study, difference in clinical profile of the study participant and difference in implementing contact screening strategy of the study areas.19,26,32,39,40 The possible difference between our finding and the study in Bangkok, Thailand might be due to the study in Thailand being solely on smear positive index for whom their contacts might get special invitation for screening due to infectiousness of the category.26 Additionally, the difference might be attributable to the study design and source of information that might be the cause of difference between our study and the study in southeast Ethiopia, Gambo hospital.38
In our current study, tuberculosis patients who had contact less than age fifteen years were more than twice as likely to undertake household contact screening. This might be because the prophylactic efforts are particularly recommended for contacts under the age of fifteen. Because of this, they can get a special invitation from health care providers.5,13 This finding was also supported by the IDI explanation that there was prioritization of screening for children due to workload and since they are target for IPT.
Another major factor of household contact screening adherence was that those with education status diploma and above were three times more likely adhered compared to those with informal education. Individuals with higher education levels were able to read and comprehend information shared on tuberculosis infection, such as the mode of transmission. This result is in line with the report of cross sectional studies from northern Ethiopia.32,33
Respondents with good knowledge about tuberculosis were adhered household contact screening three times more likely when compared to those with poor knowledge. This finding is supported by the findings of studies conducted in Thailand,19,26 and also consistent with the finding from southeast Nigeria that revealed the association of knowledge and bringing household contact for screening27 and other studies in northern Ethiopia.32,33 This is because people who have a thorough understanding of TB and the risk it poses to their families are more likely to heed the health care provider’s advice. This was supported by qualitative findings reported from Uganda and Ethiopia that poor knowledge and awareness about tuberculosis hinder contact screening.40,41
Having the favorable attitude about household contact screening was greater than two times more likely associated with odds of household contact screening adherence. This finding was supported by the studies in India42 and Tanzania43 that revealed stigma and fear of TB diagnosis are reasons why contacts were not brought to the health facility for screening. This result is also coherent with the finding from Bahir Dar Special Zone, northwest Ethiopia that reported a unit increment of respondent attitude score on household contact screening was associated with household contact screening practice.34 This infers that if the index patient believes positively about the perceived susceptibility of their contact and benefit of screening for their contact, they seek health care/bring their contact for screening.
Receiving health education from health care providers on TB was another factor significantly associated with adherence of household contact screening. This finding was supported by the study in Vietnam, which reported the majority of contacts went for screening as a result of instructions provided to them at the health education.44 This was also supported by another study conducted in Nigeria that reported the statistical significance of intensive planned health education intervention in improving contact tracing through index case.45 Another cross-sectional study in Pune, India also reported that inadequate counseling by health care provider was a barrier for contact screening higher than nineteen times when compared to those counseled adequately.39 Also supported by studies conducted in northern Ethiopia, those who received health education practiced contact screening three times more likely,32 also supported by another study in northwest Ethiopia,33 and another study in the Tigray region, northern Ethiopia also supported our finding.30 This might be due to the fact that health education delivered by care providers intensifies household contact screening practice. Our qualitative finding from IDI also expressed that lack of commitment, human resource shortage and workload of health worker were other barriers affecting household screening status. This finding was supported by qualitative finding from Hadiya Zone, southern Ethiopia that reported the absence of health worker commitment and motivation, work overload and shortage of human resource were barriers to household contact tracing.41
Respondents with smear positive type of pulmonary tuberculosis were two times more adhered to household contact screening when compared to those with pulmonary negative type. This finding was supported by the findings of a cross-sectional study from northern Ethiopia which revealed having smear negative type of pulmonary tuberculosis protects patient adherence to household contact screening by 70% compared to smear positive types.32 This could be because of the category’s high infectiousness, which invites health professionals’ attention for contact screening, and also might be due to the national guideline’s recommendation that contacts under the age of fifteen with smear-positive or drug-resistant tuberculosis are eligible for TB preventive therapy.
In conclusion, the level of HHCS adherence in our study was sub-optimal referenced to WHO and national recommendations that all household contacts of pulmonary tuberculosis should be screened. Having under fifteen years of household contacts, education status diploma and above, adequate knowledge level about tuberculosis, favorable attitude, receiving health education from health care providers and smear positive type of pulmonary tuberculosis were factors significantly associated with adherence. Health care provider and contact workload, contact knowledge and attitude, facility readiness, human resource, care provide commitments were among the factors identified by the qualitative approach.
To intensify HHCS practice, it is better to design new house contact tracing strategy like contact slips that enable index patient to start a conversation about TB with their contacts. We also recommend promoting health education for TB patients and their families and positive attitudes toward HHC screening and strengthening the commitment of health professionals to screen for HHCs and availing important logistics like household contact screening registration book for health facilities is also vital. Health facilities need to have a sustainable facility and community-based health education program for both index patients and contacts. A further study which can determine causal relationship and incorporate broader area is important. Having less than age fifteen years contact, education status, knowledge, attitude, receiving health education and type of pulmonary tuberculosis were factors associated with adherence.
Strength and Limitation of the Study
Our current study considered the previous unstudied contact factors and health care provider’s perspective through the mixed-methods study design. Our current study has its own limitations like there may be social desirability bias from participants toward the response they assumed preferable. However, we tried to overcome this by selecting data collectors from health professionals working outside the facilities, briefing the objective of the study to participants and by assuring confidentiality of their response. Working in only one town is another limitation of our study.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; HCW, Health Care Worker; HHCS, Household Contact Screening; HIV, Human Immune Deficiency Virus; HIV/AIDS, Human Immune Deficiency Virus/Acquired Immuno-deficiency Syndrome; IDI, In-depth Interview; MDR-TB, Multi-drug Resistance Tuberculosis; KI, Key Informants; OR, Odds Ratio; PTB, Pulmonary Tuberculosis; SD, Standard Deviation; SPSS, Statistical Package for Social Sciences; TB, Tuberculosis; WHO, World Health Organization.
Data Sharing Statement
Datasets used for this study are available upon request from the corresponding author.
Acknowledgments
We are eternally grateful to the omnipotent God for blessing us full health and ability. We want to express our gratitude to Jimma University for giving the opportunity to conduct this study. We would like to extend our sincere gratitude to the Shashamane Town Health Office and the Zonal Health Department for providing us with the baseline data. Our data collectors, supervisors and all respondents of our study also deserve special thanks for their cooperation.
Author Contributions
ANM conceptualized, developed the proposal, performed analysis and wrote up the result, and drafted the manuscript. LD, RFG and AFT revised the proposal, and participated in data analysis and result write up. NFW, TTK, DKD and YAD data analysis and manuscript revision. Each author significantly contributed to the work that was reported, participated in its drafting and critical evaluation, gave final approval of the version that would be published, agreed on the journal to which the article would be submitted and agreed to be responsible for all aspects of the work.
Funding
No funding was obtained for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chaisson RE, Bishai WR. Overview of tuberculosis. In: Handbook of Tuberculosis. Cham: Springer International Publishing;2017:1–15. doi:10.1007/978-3-319-26273-4_1
2. World Health Organization. Operational Handbook on Tuberculosis Module 1: Prevention-Tuberculosis Preventive Treatment. Geneva: World Health Organization; 2020:1–119.
3. World Health Organization. Global Tuberculosis Report. Geneva: World Health Organization; 2021:1–10.
4. Fox GJ, Dodd PJ, Marais BJ. Household contact investigation to improve tuberculosis control. Lancet Infect Dis. 2019;19(3):235–237. doi:10.1016/S1473-3099(19)30061-1
5. Ethiopian Federal Ministry of Health. Guidelines for clinical and programmatic management of TB, TB/HIV, DR-TB and Leprosy in Ethiopia. TBL guideline; 2021.
6. World Health Organization. Systematic Screening for Active tuberculosis: Principles and Recommendations. Who/Htm/Tb/201304. World Health Organization; 2013:1–123.
7. Kuznetsov VN, Grjibovski AM, Mariandyshev AO, Johansson E, Bjune GA. A comparison between passive and active case finding in TB control in the Arkhangelsk region. Int J Circumpolar Health. 2014;73(1):1–10. doi:10.3402/ijch.v73.23515
8. Chen J-O, Qiu Y, Rueda ZV, et al. Role of community-based active case finding in screening tuberculosis in Yunnan province of China. BMC Infect Dis Poverty. 2019;8(1):1–12. doi:10.1186/s40249-019-0602-0
9. World Health Organization. The End Tb Strategy: Global Strategy and Target for Tuberculosis Prevention, Care and Control After 2015. Geneva: World Health Organization; 2014:1–30.
10. Stop TB Partnership W. Using contact investigation to improve TB case detection 1; 2018.
11. TB care I. Adaptation and Implementation Guide for Recommendations for Inves- Tigating Contacts of Persons with Infectious Tuberculosis in Low- and Middle-Income Countries. The haguee: TB care I; 2015.
12. Claessens NJM, Gausi FF, Meijnen S, Weismuller MM, Salaniponi FM, Harries AD. Screening childhood contacts of patients with smear-positive pulmonary tuberculosis in Malawi. Int J Tuberc Lung Dis. 2002;6(4):362–364.
13. World Health Organization. Recommendations for Investigating Contacts of Persons with Infectious Tuberculosis in Low- and Middle-Income Countries. WHO/HTM/TB/2012.9. Geneva: World Health Organization; 2012:27–30.
14. Pande T, Vasquez NA, Cazabon D, et al. Finding the missing millions: lessons from 10 active case finding interventions in high tuberculosis burden countries. BMJ Glob Heal. 2020;5(12):e003835. doi:10.1136/bmjgh-2020-003835
15. Hamada Y, Glaziou P, Sismanidis C, Getahun H. Prevention of tuberculosis in household members: estimates of children eligible for treatment. Bull World Health Organ. 2019;97(8):534–547D. doi:10.2471/BLT.18.218651
16. World Health Organization. TUBERCULOSIS GLOBAL REPORT 2020. World Health Organization; 2020.
17. Ross JM, Xie Y, Wang Y, et al. Estimating the population at high risk for tuberculosis through household exposure in high-incidence countries: a model-based analysis. eClinicalMedicine. 2021;42:101206. doi:10.1016/j.eclinm.2021.101206
18. World Health Organization. Global Tuberculosis Report. Geneva: World Health Organization; 2020.
19. Fox GJ, Loan LP, Nhung NV, et al. Barriers to adherence with tuberculosis contact investigation in six provinces of Vietnam: a nested case – control study. BMC Infect Dis. 2015;15(103):1–8. doi:10.1186/s12879-015-0816-0
20. Resistance D, Pan Z, Zhang J, et al. The gap between global tuberculosis incidence and the first milestone of the WHO end tuberculosis strategy: an analysis based on the global burden of disease 2017 database. Dovepress. 2020;13:1281–1286.
21. Singh J, Sankar MM, Kumar S, et al. Incidence and prevalence of tuberculosis among household contacts of pulmonary tuberculosis patients in a Peri-Urban Population of South Delhi, India. PLoS One. 2013;8(7):1–11.
22. Sayedi SM, Seddiq MK, Rashidi MK, et al. Active household contact screening for tuberculosis and provision of isoniazid preventive therapy to under-five children in. PLoS One. 2020;15(10):1–11. doi:10.1371/journal.pone.0240031
23. FMOH. National strategic plan tuberculosis and leprosy control 2006 – 2013 EC (2013/14 – 2020) with; 2017: 92. Available from: https://www.who.int/tb/publications/global_report/GraphicExecutiveSummary.pdf.
24. Ethiopian Federal Ministry of Health. 2013 EFY annual performance report of the Ethiopian Health Sector; 2020.
25. Hwang TJ, Ottmani S, Uplekar M. A rapid assessment of prevailing policies on tuberculosis contact investigation. Int J Tuberc Lung Dis. 2011;15(12):1620–1623. doi:10.5588/ijtld.11.0222
26. Tornee S, Kaewkungwal J, Fungladda W, Silachamroon U, Akarasewi P, Sunakorn P. Factors associated with the household contact. Southeast Asian J Trop Med Public Health. 2005;36(2):331–340.
27. Omotowo BI, Ekwueme OC AM. Tuberculosis control mechanisms and contact tracing: knowledge and practice among TB Patients At Dots Centers in Southeast Nigeria. J Biom Biostat. 2012;01(451):1–6.
28. Tefera F, Barnabee G, Sharma A, et al. Evaluation of facility and community-based active household tuberculosis contact investigation in Ethiopia: a cross-sectional study. BMC Health Serv Res. 2019;19(234):1–9. doi:10.1186/s12913-019-4074-5
29. Gashu Z, Jerene D, Ensermu M, Habte D, Melese M. The yield of community-based “Retrospective” tuberculosis contact investigation in a high burden setting in a high burden setting in Ethiopia. PLoS One. 2016;11(8):1–13. doi:10.1371/journal.pone.0160514
30. Gebretnsae H, Ayele BG, Hadgu T, et al. Implementation status of household contact tuberculosis screening by health extension workers: assessment findings from programme implementation in Tigray region, northern Ethiopia. BMC Health Serv Res. 2020;20(27):1–7. doi:10.1186/s12913-020-4928-x
31. Assefa D, Klinkenberg E, Yosef G. Cross sectional study evaluating routine contact investigation in Addis Ababa, Ethiopia: a missed opportunity to prevent tuberculosis in children. PLoS One. 2015;10(6):1–10. doi:10.1371/journal.pone.0129135
32. Gebregergs GB, Alemu WG. Household contact screening adherence among tuberculosis patients in Northern Ethiopia. PLoS One. 2015;10(5):1–8. doi:10.1371/journal.pone.0125767
33. Shiferaw DA, Mekonnen HS, Abate AT. House-hold contact tuberculosis screening adherence and associated factors among tuberculosis patients attending at health facilities in Gondar town, northwest. BMC Infect Dis. 2019;19(1063):1–8. doi:10.1186/s12879-019-4695-7
34. Fentahun N, Wasihun Y, Mamo A, Gebretsadik LA. Contact screening and isoniazid preventive therapy initiation for under-five children among pulmonary tuberculosis-positive patients in Bahir Dar Special Zone, Northwest Ethiopia: a cross- sectional study. Hindawi. 2020;2020:1–8.
35. Getahun B, Nkosi ZZ. Satisfaction of patients with directly observed treatment strategy in Addis Ababa, Ethiopia: a mixed-methods study. PLoS One. 2017;12(2):e0171209. doi:10.1371/journal.pone.0171209
36. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117. doi:10.1186/1471-2288-13-117
37. Federal Democratic Republic of Ethiopia Ministry of Health. Guidelines for Management of TB, DR-TB and Leprosy. Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health; 2018:1–180.
38. Ramos JM, Biru D, Tesfamariam A, Reyes F, Górgolas M. Screening for tuberculosis in family and household contacts in a rural area in Ethiopia over a 20-month period. Int J Mycobacteriology. 2013;2(4):240–243. doi:10.1016/j.ijmyco.2013.10.001
39. Belgaumkar V, Chandanwale A, Valvi C, et al. Barriers to screening and isoniazid preventive therapy for child contacts of tuberculosis patients. Int J Tuberc Lung Dis. 2018;22(10):1179–1187. doi:10.5588/ijtld.17.0848
40. Ayakaka I, Ackerman S, Ggita JM, et al. Identifying barriers to and facilitators of tuberculosis contact investigation in Kampala, Uganda: a behavioral approach. BMC. 2017;12(33):1–13.
41. Tesfaye L, Lemu YK, Tareke KG, Chaka M, Feyissa GT. Exploration of barriers and facilitators to household contact tracing of index tuberculosis cases in Anlemo district, Hadiya zone, Southern Ethiopia: qualitative study. PLoS One. 2020;15(5):1–16. doi:10.1371/journal.pone.0233358
42. Velayutham B, Jayabal L, Watson B, et al. Tuberculosis screening in household contacts of pulmonary tuberculosis patients in an urban setting. PLoS One. 2020;15(10):e0240594. doi:10.1371/journal.pone.0240594
43. Emerson C, Ng’eno B, Ngowi B, et al. Assessment of routine screening of pediatric contacts of adults with tuberculosis disease in Tanzania. Public Heal Action. 2019;9(4):148–152. doi:10.5588/pha.19.0034
44. Hoang T, Thanh T, Ngoc SD, Viet NN, Van HN, Horby P. A household survey on screening practices of household contacts of smear positive tuberculosis patients in Vietnam. BMC Public Health. 2014;14(713):1–7. doi:10.1186/1471-2458-14-1
45. Ekwueme OC, Omotowo BI, Agwuna KK. Strengthening contact tracing capacity of pulmonary tuberculosis patients in Enugu, southeast Nigeria: a targeted and focused health education intervention study. BMC Public Health. 2014;14(1175):1–17. doi:10.1186/1471-2458-14-1175
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.