Back to Journals » Risk Management and Healthcare Policy » Volume 16
Hospitalization Costs for Patients with Acute Appendicitis: An Update Using Real-World Data from a Large Province in China
Authors Peng N , He Q, Bai J, Chen C, Liu GG
Received 19 September 2023
Accepted for publication 17 November 2023
Published 20 December 2023 Volume 2023:16 Pages 2805—2817
DOI https://doi.org/10.2147/RMHP.S436853
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Nan Peng,1 Qinghong He,2 Jie Bai,1 Chen Chen,3 Gordon G Liu1,4
1School of International Pharmaceutical Business, China Pharmaceutical University, Nanjing, Jiangsu, 211198, People’s Republic of China; 2Institute of Economics, Chinese Academy of Social Sciences, Beijing, 100836, People’s Republic of China; 3Department of Global Health, School of Public Health, Wuhan University, Wuhan, 430071, People’s Republic of China; 4Institute for Global Health and Development, Peking University, Beijing, 100080, People’s Republic of China
Correspondence: Gordon G Liu, Institute for Global Health and Development, Peking University, Beijing, 100080, People’s Republic of China, Email [email protected]
Purpose: The aim of this study is to investigate the factors influencing hospitalization costs for patients diagnosed with acute appendicitis in China.
Methods: We conducted a cross-sectional study using data from Provincial Health Statistics Support System Database from S Province in China. This dataset contained all hospital’s electronic medical records from January 1, 2015 to December 31, 2018 including both public and private hospitals. The target population was identified based on the principal diagnosis of appendicitis (ICD-10: K35). To examine the impact of various factors on hospitalization costs, we conducted a multivariate linear regression analysis. Furthermore, we employed the Shapley value decomposition method to gain a more comprehensive understanding of the factors that influenced hospitalization costs and their respective levels of importance.
Results: Our study comprised 317,200 cases. During the period from 2015 to 2018, the average hospitalization expenses for patients with acute appendicitis were estimated at approximately 7014 RMB (1061 USD), which accounts for a considerable 12% of China’s per capita GDP. The results of this study demonstrate a significant correlation between various factors, such as the patient’s age, gender, marital status, occupation, payment method, number of complications, treatment method, hospital tier, and ownership, and the total hospitalization costs and subcomponents of hospitalization costs. Notably, the treatment method employed had the most substantial impact on hospitalization costs.
Conclusion: To the best of knowledge, this is one of the first studies to investigate the hospitalization costs of acute appendicitis incorporating both patient-level and hospital-level covariates, using a large sample size. To reduce the costs associated with acute appendicitis in China, it is recommended to consider suitable treatment options and explore the option of receiving medical care at lower-tier and privately-owned healthcare facilities.
Keywords: appendicitis, hospitalization costs, influencing factors, multivariate regression
Introduction
Acute appendicitis (AA) is one of the most common general surgical emergencies worldwide.1 The global incidence of AA (0.23%)2 was higher than that of the most common cancers among men (lung cancer with an incidence of 0.01%) or women (breast cancer with an incidence of 0.06%).3 The incidence of appendicitis is reported to be higher in low and middle-income countries(LMICs) than in many Western countries and has been increasing in LMICs over the last three decades.4 AA is a prevalent medical emergency that can affect individuals of all ages, with a higher incidence observed among those aged between 10 and 30 years.1,5,6 The majority of studies indicated a minor prevalence of males.1 Additionally, untreated appendicitis and negative appendectomies may result in severe impairment and fatality.7 The incidence of perforation in acute appendicitis varies between 16% and 40%, with a higher occurrence in younger individuals (40% to 57%) and those over 50 years old (55% to 70%). Perforated appendicitis is linked to increased morbidity and mortality in comparison to non-perforated appendicitis.8
The current standard and most widely accepted treatment of AA is an appendectomy.7,8 Over 95% of appendicitis patients in the United States had an appendectomy as recently as 2014.9 As one of the most common emergency surgery, appendectomy contributes substantially to the disease burden on modern health systems.1 For low and middle-income countries, the lower rates of health insurance reimbursement combined with the continuing increase in incidence underscore the importance of the issue of the disease burden of AA.
Appendicitis imposed a significant economic burden on China. According to a study conducted in China, acute appendicitis was found to be the fifth most economically burdensome disease, following myocardial infarction coronary artery bypass, acute myocardial infarction, cerebral hemorrhage, and acute upper gastrointestinal bleeding.10 The total economic burden of acute appendicitis was 230 ($billion), which accounted for 4.45% of the total health expenses in China.
Medical costs linked to AA are predominantly utilized in hospitals.8 The most common treatment for patients with AA is surgical treatment,11 and the total costs for hospitalization are the direct economic burden for inpatients and their families, so it is particularly important to determine the influencing factors for hospitalization expenses.
There are many international studies on the medical costs of appendicitis. Taking different regions as examples, it has shown that the average total costs of appendicitis for hospitalization in the United States (2018) were US $1181,12 accounting for about 2% of the US GDP per capita in 2018. In the Netherlands (2019), there were about 13,500 patients receiving treatment for appendicitis annually, with the average hospitalization costs per patient of US $4384,13 accounting for 9.7% of the Netherlands’s GDP per capita between 2006–2015. In Asia, taking Japan as an example, the average total costs of appendicitis for hospitalization in Japan (2018) were about US $6075,14 accounting for 15.3% of Japan’s GDP per capita in 2018.
Turning attention to the literature on factors influencing costs, we found that recent international literature studies focused on the impacts of different treatment methods on the medical costs of appendicitis.15–19 Since it spares the use of personal protective equipment, eases the strain on operating rooms, and lowers total expenses, nonoperative management may be more advantageous to health care systems than operative management.19 However, most studies pointed to a significant increase in cost of care with nonoperative management, and they also suggested that prolonged hospital stays might be linked to higher care costs. Besides, compared to laparoscopic surgery, open surgery is more costly to treat. Some literature examined the impacts of health insurance type.9 Clement20 analyzed the treatment costs in 99 patients with appendicitis undergoing laparoscopic surgery at Ninewells Hospital, UK, and revealed that the treatment costs were mainly affected by surgical duration (53.2%) and hospital stay (39.2%). The costs of treatment were not influenced by gender and did not vary significantly between adult and pediatric patients.20,21 However, they were found to be higher in the elderly population,20,22 this may be associated with increased utilization of imaging. Comorbidities of the patient are another element that influences the cost, and the elderly generally have more comorbidities.22
The main factors affecting hospitalization costs of appendicitis in the existing domestic literature were the length of stay(LOS),23–25 received surgery or not,23,25 having any comorbidities or not,24 age,24–26 appendicitis severity,26 surgical grades27 and payment methods.24 Despite the abundance of literature on the subject, the majority of studies have relied on cross-sectional data with limited sample sizes from a single or a few hospitals. Consequently, these studies have failed to account for the influence of various factors, including hospital-level variables. Additionally, there exists a deficiency in studies examining the temporal trends of the fundamental determinants of the total hospitalization costs for appendicitis.
This paper had made some contributions to the previous literature in the following ways. To begin with, we investigated the hospitalization costs of AA by utilizing the data from province S between 2015 and 2018. We employed panel data with a large sample size, which allowed us to incorporate a wide range of covariates, including patient-level and hospital-level covariates, to provide a complete understanding of the factors associated with the hospitalization costs of AA. Subsequently, we conducted a more in-depth examination of the temporal patterns of pivotal determinants. Secondly, utilizing the Shapley value decomposition method, we delved deeper into the factors that influenced hospitalization costs and their relative importance. The results indicated that treatment methods were the most crucial factor in determining hospitalization costs. Additionally, it is crucial to examine the driving factors behind the hospitalization costs associated with AA, which is a widespread general surgical emergency worldwide and leads to a significant economic burden on individuals and society. The findings indicate that selecting suitable treatment methods in public or private hospitals of lower tier can be an effective measure to manage hospitalization costs for patients with AA. This has significant policy implications for low- and middle-income nations.
Data and Methods
Case Selection
This study was a population-based retrospective observational study that adopted a healthcare system perspective, which mainly focused on direct healthcare costs.
This study contained all appendicitis inpatients admitted to hospitals in Province S, China, from January 1, 2015 to December 31, 2018. The patient-level information comes from all hospitals’ electronic medical record system in Province S, including the inpatient’s basic information (age, gender, health insurance schemes), admission information (admission source, ICD-code of primary diagnosis, and the number of secondary diagnoses), and discharge information (discharge method, health outcomes, and inpatient costs). Based on ICD-10 codes with variations in the three digits after the decimal point, we identified all appendicitis-related admissions from January 1, 2015, to December 31, 2018. As shown in Figure 1, two inclusion criteria were applied: (1) patients were admitted with the principal diagnosis of appendicitis (ICD-10: K35), (2) the date of admission was between January 1, 2015 to December 31, 2018. In addition, we excluded patients with missing gender, marriage status, hospital tier and other control variables.
 |
Figure 1 Flow chart of the sampling process. |
Variable Measurements
In this study, the dependent variable was hospitalization costs, including total hospitalization costs and sub-group costs. Total hospitalization costs consisted of diagnostic costs, treatment fees, drug costs, material costs, and other costs. Diagnostic costs included diagnostic pathology costs, laboratory diagnostic costs, diagnostic imaging costs, and clinical diagnostic program costs. Treatment fees included surgical treatment costs and non-surgical treatment costs. Drug costs included western medicine costs, antimicrobial drug costs, Chinese medicine costs, Chinese herbal medicine costs, and proprietary Chinese medicine costs. Material costs included material costs for inspection, surgical material costs, and material costs for treatment. Other costs included comprehensive medical service costs, rehabilitation costs, Chinese medical treatment costs, and blood product costs.
To study the factors affecting hospitalization costs in the hospital, we merged hospital-level information with patient-level details according to the unified provider ID to form the combined hospital-inpatient data. More specifically, patient-level covariates included age, gender, occupation, health insurance schemes, number of complications and treatment method. The treatment method was categorized into open appendectomy, laparoscopic appendectomy and non-operation. Besides, occupations included workers, farmers, students and freelancers, jobless and retired and others. Health insurance schemes consisted of three main social health insurance, the urban employee basic medical insurance (UEBMI), the urban resident basic medical insurance (URBMI), and the new rural cooperative medical system (NRCMS), in addition to other social insurance. The number of complications was denoted as the number of second diagnoses.
In addition, we included the following hospital-level covariates: ownership, hospital tier and location of the hospital. In China, the health care system was organized as a three-tiered system, which included tertiary hospitals (including teaching hospitals), secondary hospitals (including urban district hospitals and rural county hospitals), and primary health centers (PHCs) (including community health centers and rural township hospitals).24 In this study, hospital tier consist of I tier or unclassified hospitals, II tier hospitals, and III tier hospitals. Moreover, hospitals were divided into public and private hospitals according to hospital ownership. The location of the hospital indicated the prefecture-level city where the hospital is located.
Statistical Analysis
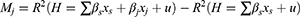
To investigate how the factors influence hospitalization costs, we employed multivariate linear regression with the following equation (1):
The dependent variable Yiht was denoted as hospitalization costs for individual i who was treated in hospital h in year t. β1 to β9 indicated age, gender, marriage status, occupation, treatment method, number of complications, payment method, hospital tier, and ownership, respectively. Also, city-level fixed effects δcity and time-fixed effects γt were controlled.
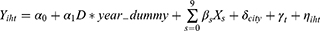
Moreover, based on the above regression equation (1), we used the Shapley value decomposition method to further analyze what contributed to the hospitalization costs and their relative importance. According to the Shapley value decomposition method, the marginal contribution of influencing factors to hospitalization costs is the amount of change in the goodness of fit before and after the variable is removed from the regression equation, namely:
The relative contribution of this influencing factor is equal to the ratio of the Shapley value of this influencing factor to the sum of the Shapley values of all explanatory variables. Furthermore, statistical analyses were performed in Stata 17.0.
Furthermore, we used equation (3) to examine the temporal trends of critical influential factors:
where Yiht was the dependent variable, which denoted the appendicitis inpatient costs for individual i who was treated in hospital h in year t. Xs was a vector of control variables consist with equation(1). The variable D*year_dummy was the interaction of our main independent variable of interest and year trend, which indicated the temporal trends of critical influential factors. D included treatment method, hospital tier, hospital ownership, patients’ age, and number of complications. We also controlled city-level fixed effects δcity and time-fixed effects γt.
Ethical Considerations
Ethical approval for this study was obtained from China Pharmaceutical University (IRB approval number: CPU2021026). Participants in the study were not required to give their consent because the data were obtained retrospectively. The ethics committee waived the requirement for informed consent. All participant personal information is unidentifiable. Ethical principles of the Declaration of Helsinki were adhered to throughout this study.
Results
Descriptive Statistics
After applying our selective criteria, a total of 317,200 patients were included in the study. The primary characteristics of these patients have been presented in Table 1. The male-to-female ratio was approximately 1:1. Hospitalization costs differed among the various health insurance schemes, with the average costs for UEBMI, URBMI, and NRCMS being 7800 RMB, 7034 RMB, and 6373 RMB, respectively. The number of complications was an important factor, the more numbers were, the higher costs were. As far as the treatment method, the proportion of patients who operated open procedures was about 40%. The hospitalization costs of laparoscopic appendectomy were the highest among the three treatments. Concerning hospital tiers, tertiary and public facilities were the preferred choices among patients, with primary, secondary, and tertiary hospitals incurring average hospitalization costs of 3986 RMB, 5578 RMB, and 8185 RMB, respectively.
 |
Table 1 Descriptive Statistics of Inpatients with Acute Appendicitis from 2015 to 2018 |
Components of Hospitalization Costs
On average, hospitalization costs per patient amounted to 7014 RMB (±4654) (Table 2). The reimbursement of expenses accounted for the largest portion of hospitalization costs, representing 81.05% of the total costs per patient. The medicine products cost consisted of the largest proportion (27.84%) of the hospitalization costs, including 27.47% western medicine costs, 7.98% antimicrobial drug costs and 0.38% traditional Chinese medicine costs. Diagnosis costs accounted for 20.40% of total hospitalization costs, followed by treatment fees (19.74%). Chinese medical treatment costs accounted for 0.1%, which was the smallest part.
 |
Table 2 Components of Hospitalization Costs (RMB) |
Regression Results
Table 3 displayed the findings of a multiple linear regression model. The results showed that patients’ age, gender, marriage status, occupation, payment method, number of complications, treatment method, hospital tier and hospital ownership were significantly associated with total hospitalization costs and other costs. More specifically, compared to women, men spent 0.59% more on total hospitalization costs. On average, the total hospitalization costs are higher for children and the elderly than for young people. Compared to unmarried, the total hospitalization costs for married patients increased by 2.15%. Compared with patients who participated in UEBMI, total hospitalization costs were 8.64%, 7.72%, 9.26%, and 5.83% lower for URBMI, NRCMS, other social insurance, and fully self-paying patients, respectively. Regarding the occupation of the patients, the total hospitalization costs were on average 0.23%, 4.62%, 5.88% and 5.52% higher for students and other freelancers, the unemployed and retired people, and others, versus farmers.
 |
Table 3 Regression Results |
Moreover, the total hospitalization costs increased by 10.3% for each additional complication. In addition, compared to patients who did not have surgery, hospitalization costs increased by 98.61% and 120.12% for open surgery and laparoscopic surgery, respectively. Total hospitalization costs for patients in tier II and tier III hospitals were on average 17.42% and 44.13% more than those in tier I and unclassified hospitals. Hospitalization costs for patients in private hospitals were on average 11.18% more than those in government-owned hospitals. For columns 2 through 5 in Table 3, where other types of costs were reported, the results for the impact factors were generally consistent with the results for total hospitalization costs in column 1.
Relative Importance of Influencing Factors
This section utilized the linear regression model to examine the relative importance of crucial variables in determining the total hospitalization costs. The results indicated that the ranking of relative importance was: treatment method (0.544), number of complications (0.1692), hospital tier (0.1249), city (0.0515), age (0.0341), hospital ownership (0.03828), occupation (0.0186), payment method (0.015), marriage (0.0027), and gender (0.0017). The treatment method and number of complications were the key determinants of the variation in hospitalization costs, contributing to approximately 0.7132 of the total variation. Conversely, the variables at the patient level had a relatively minor impact.
Time Trend of Influencing Factors
Subsequently, we proceeded to conduct a more in-depth analysis of the temporal trends of critical influential factors, utilizing 2015 as the baseline year (see Figure 2). Our findings, as depicted in Panel A and Panel B of Figure 2, indicated that the laparoscopic surgery incurred the highest total hospitalization costs, in contrast to the open surgery and no surgery. Furthermore, we observed a slight reduction in the disparity between the total hospitalization costs of the laparoscopic surgery and the open surgery in 2018, relative to 2015.The data presented in Panel D and Panel E indicated a positive correlation between the hospital tier and total hospitalization costs of AA. Notably, the discrepancy in total hospitalization expenses between PHCs and tier II hospitals, as well as between tier II and tier III hospitals, has been exhibiting a declining trend. Panel F indicated that the total hospitalization costs in public hospitals exceeded those in private ones. Moreover, the difference between the two widened during the initial two years and narrowed down slightly in 2018, as compared to 2015.
In accordance with Panel G, it can be observed that the total hospitalization costs incurred by the elderly demographic surpass those of the 18–65 age cohort. Nevertheless, there has been a gradual reduction in the contrast between the two groups over time. According to the findings in Panel H, the number of patient complications has a significant and positive effect on the total hospitalization costs, despite a slight decline in the coefficient magnitude in 2018 relative to 2015.
Discussion
The study revealed that the average expenses incurred during hospitalization of patients with acute appendicitis ranged around 7014 RMB from 2015 to 2018, which accounted for approximately 12% of China’s per capita GDP. A regression analysis revealed that various demographic characteristics of patients, including the number of complications, gender, age, and occupation, had a significant impact on the hospitalization costs for acute appendicitis patients. Furthermore, it was found that the treatment method employed was the most influential factor in determining hospitalization costs.
Compared to the study in the Netherlands, the hospitalization costs were €3700 per patient between 2006 and 2016,13 which was much higher than this study. The average total costs of appendicitis for hospitalization in Japan were about US $6075 in 2020.14 In general, the hospitalization costs of this study were significantly lower than those of the developed nations. However, in terms of the percentage of GDP per capita, the hospitalization costs of appendicitis in China were lower than that of Japan but higher than that of the Netherlands. Our study provides important and up-to-date evidence on the costs of patients with appendicitis in China. This is important for future comparative assessments of the cost-effectiveness of therapeutic interventions for patients with appendicitis.
Among the various cost groups that were categorized, drug costs had the highest share of almost 28% of the total direct medical costs, surpassing the corresponding figures of other nations. The results were consistent with several previous studies in China.23,28 In the UK, for instance, medication accounts for 2% of the total costs for appendicectomy.20 The percentage of drug costs is 0.4% of the total direct medical costs for appendix care in the acute surgical unit (ASU) in Australia, 12.9% in Thailand, and 2.2% in Japan.14,26,29
The study’s regression analysis revealed a significant (P<0.05) association between hospitalization costs and patients’ age. The data revealed a nominal uptick in spending for individuals aged over 65 years, in contrast to those aged between 18–65 years. However, it is important to note that the coefficient size exhibited a downward trend over time. Moreover, it is crucial to highlight that the number of patient complications had a positive impact on the total hospitalization costs. Nevertheless, it is worth mentioning that the coefficient size experienced a slight decrease in 2018. A study in Taiwan25 showed that age and complications had a significant impact on the hospitalization costs of patients with AA, especially the hospitalization cost of the elderly increased significantly, which was similar to the results of this study. Many international studies30,31 have found that children with complications have a longer length of stay and higher hospitalization costs than children without complications.
Ever since the nineteenth century, when appendectomies were first performed by surgeons, surgery has been the treatment that has gained the most widespread acceptance.8 The use of minimally invasive techniques in surgical procedures is increasingly prevalent, particularly in the removal of the appendix, where it is recommended as a standard approach.32 Compared with the open appendectomy, the laparoscopic appendectomy was consistently associated with higher hospitalization costs. This result was consistent with the results of most previous studies.15,33–35 Moreover, it was discovered that the gap in total hospitalization expenditures between the laparoscopic appendectomy and the open appendectomy was narrowing. Furthermore, we only evaluated the direct hospitalization costs, whereas laparoscopic appendectomy offers considerable advantages over open appendectomy.36 Current evidence showed laparoscopic appendectomy to be the most effective surgical treatment, was associated with a lower incidence of wound infection and post-intervention morbidity, shorter hospital stays, and better quality of life scores compared to open appendectomy.37,38 Meanwhile, non-operative treatment of appendicitis was an economical choice, as we can see from our study, which other studies have also proposed.39–42
China has a 3-tier healthcare system that consists of PHCs, secondary hospitals, and tertiary hospitals.43 In 2015, China implemented the Hierarchical Medical System to alleviate the unbalanced distribution of medical resources and promote equal access to primary medical and health services. However, most patients in China increasingly bypass primary care and access the health system at higher-tier hospitals when they require medical treatment.44–46 In terms of our study, most patients with acute appendicitis were also willing to seek treatment in high-tier hospitals. Some evidence indicates there are wide gaps in the quality of primary health care, and residents do not trust the health services provided by primary care facilities.47 On the other side, differences in hospitalization costs among different tiers of hospitals were significantly larger. According to more details about the hospitalization costs in our study, high-tier hospitals charged higher fees for diagnosis, treatment, drugs, and other aspects. These all contributed to high hospitalization costs in all three treatments. Additionally, our investigation indicated a reduction in the discrepancy of total hospitalization costs among different tiers of medical institutions. This was evidenced by the decreasing disparity between tier II hospitals and PHCs, as well as the diminishing gap between tier III hospitals and tier II hospitals. To reduce the economic burden of AA or other diseases, China needs to further optimize the hierarchical medical treatment system and further improve the level of treating patients.
Subsequently, we used against medical advice (AMA) as an indicator of the quality of care.48 AMA, which refers to patients leaving the hospital against medical advice, is an indicator of poor quality. Table 4 demonstrates that secondary and tertiary hospitals have a significantly higher probability of AMA compared to primary and unclassified hospitals, indicating lower quality. Furthermore, Table 1 shows that hospitalization costs are significantly higher in public hospitals than in private hospitals. However, our results revealed no significant difference in AMA rates between public and private hospitals (Table 4), suggesting that quality is not significantly different between the two types of hospitals. In this regard, we believe that a hierarchical medical system should be established for diseases such as AA with a high degree of standardized treatment. In addition, private hospitals should be encouraged to enhance hospital competition to improve the quality of care.
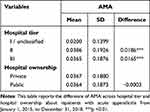 |
Table 4 The Difference of AMA Across Hospital Tier and Hospital Ownership |
It is important to recognize that this study has certain limitations. Firstly, due to the unavailability of national data, only provincial data was utilized for the analysis of factors influencing the hospitalization costs for acute appendicitis. Secondly, relevant potential confounding factors such as the timing of surgery, the patient’s physical condition at admission (including weight), and postoperative complications, which can impact hospitalization costs, could not be further differentiated. Thirdly, the outpatient costs of acute appendicitis were not examined, and it is recommended that future studies investigate this aspect.
Conclusion
This study examined every patient diagnosed with acute appendicitis in S Province’s public and private hospitals between 2015 and 2018. The average hospitalization costs for patients with acute appendicitis was found to be 7014 RMB. Furthermore, we found that the main factors influencing hospitalization cost for AA were the treatment method, number of complications, hospital tier, age, hospital ownership, occupation, payment method, gender and so on, among which treatment method was the most important factor affecting hospitalization cost. To manage the hospitalization costs for acute appendicitis patients in China or other LMICs, it is recommended that patients consider options such as selecting appropriate treatment methods, seeking care at lower-tier hospitals, or consulting with private healthcare providers.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Consent for Publication
Details in this study can be published.
Funding
There was no financial support or funding source for this study.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278–1287. doi:10.1016/S0140-6736(15)00275-5
2. Wickramasinghe D, Xavier C, Samarasekera D. The worldwide epidemiology of acute appendicitis: an analysis of the global health data exchange dataset. World J Surg. 2021;45. doi:10.1007/s00268-021-06077-5
3. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca A Cancer J Clinicians. 2021;71(3):209–249. doi:10.3322/caac.21660
4. Ferris M, Quan S, Kaplan BS, et al. The global incidence of appendicitis: a systematic review of population-based studies. Ann Surg. 2017;266(2):237–241. doi:10.1097/SLA.0000000000002188
5. Ilves I, Fagerström A, Herzig KH, Juvonen P, Miettinen P, Paajanen H. Seasonal variations of acute appendicitis and nonspecific abdominal pain in Finland. World J Gastroenterol. 2014;20(14):4037–4042. doi:10.3748/wjg.v20.i14.4037
6. Viniol A, Keunecke C, Biroga T, et al. Studies of the symptom abdominal pain--A systematic review and meta-analysis. Fam Pract. 2014;31(5):517–529. doi:10.1093/fampra/cmu036
7. Baird DL, Simillis C, Kontovounisios C, Rasheed S, Tekkis PP. Acute appendicitis. BMJ. 2017;357:j1703.
8. Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27. doi:10.1186/s13017-020-00306-3
9. Sceats LA, Trickey AW, Morris AM, Kin C, Staudenmayer KL. Nonoperative management of uncomplicated appendicitis among privately insured patients. JAMA Surg. 2019;154(2):141–149. doi:10.1001/jamasurg.2018.4282
10. Song X, Lan L, Zhou T, Yin J, Meng Q. Economic Burden of Major Diseases in China in 2013. Front Public Health. 2021;9:649624. doi:10.3389/fpubh.2021.649624
11. Walędziak M, Lasek A, Wysocki M, et al. Risk factors for serious morbidity, prolonged length of stay and hospital readmission after laparoscopic appendectomy - results from Pol-LA (Polish Laparoscopic Appendectomy) multicenter large cohort study. Sci Rep. 2019;9(1):14793. doi:10.1038/s41598-019-51172-2
12. Malhotra L, Pontarelli EM, Grinberg GG, Isaacs RS, Morris JP, Yenumula PR. Cost analysis of laparoscopic appendectomy in a large integrated healthcare system. Surg Endosc. 2022;36(1):800–807. doi:10.1007/s00464-020-08266-0
13. de Wijkerslooth Elisabeth ML, Wijnhoven WB. Disease burden of appendectomy for appendicitis: a population-based cohort study. Surg Endosc. 2020;34(1):116–125. doi:10.1007/s00464-019-06738-6
14. Sugiura K, Suzuki K, Umeyama T, Omagari K, Hashimoto T, Tamura A. Cost-effectiveness analysis of initial nonoperative management versus emergency laparoscopic appendectomy for acute complicated appendicitis. BMC Health Serv Res. 2020;20(1):1019. doi:10.1186/s12913-020-05839-6
15. Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L. Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg. 2016;11(1):44. doi:10.1186/s13017-016-0102-5
16. Buitrago G, Junca E, Eslava-Schmalbach J, Caycedo R, Pinillos P, Leal LC. Clinical outcomes and healthcare costs associated with laparoscopic appendectomy in a middle-income country with universal health coverage. World J Surg. 2019;43(1):67–74. doi:10.1007/s00268-018-4777-5
17. Alves VHR, Guimarães NM, Soares BS, Ruiz LM, Martins Filho J, Silva RCDD. Cost-benefit analysis of surgical appendectomy in the brazilian public health system. RSD. 2022;11(11):e359111133315. doi:10.33448/rsd-v11i11.33315
18. Carrillo montenegro AF, Aristizabal Rojas S, Pulido Segura JA, et al. Single incision laparoscopic appendectomy with surgical-glove port is cost-effective and reliable in complicated acute appendicitis: a casecontrol multicenter study in Colombia. Heliyon. 2023;9(1):e12972. doi:10.1016/j.heliyon.2023.e12972
19. De Almeida Leite RM, Seo DJ, Gomez-Eslava B, et al. Nonoperative vs operative management of uncomplicated acute appendicitis: a systematic review and meta-analysis. JAMA Surg. 2022;157(9):828. doi:10.1001/jamasurg.2022.2937
20. Clement KD, Emslie K, Maniam P, Wilson MSJ. What is the operative cost of managing acute appendicitis in the NHS: the impact of stump technique and perioperative imaging. World J Surg. 2020;44(3):749–754. doi:10.1007/s00268-019-05306-2
21. Rogers EB, Davenport DL, Parrish J, Bernard AC. Variability in hospital costs for short stay emergent laparoscopic appendectomy. Surg Open Sci. 2022;10:223–227. doi:10.1016/j.sopen.2022.10.007
22. Kim KH, Lee SC, Lee SK, Choi BJ, Jeong W, Kim SJ. Does Korea’s current diagnosis-related group-based reimbursement system appropriately classify appendectomy patients? Ann Surg Treat Res. 2016;91(2):66. doi:10.4174/astr.2016.91.2.66
23. Sheng LY, Gao LM, Zhou L. Influencing factors on hospitalization expenses of inpatients with acute appendicitis. Chinese Rural Health Service Administration; 2013. Available from: http://en.cnki.com.cn/Article_en/CJFDTotal-ZNWS201305010.htm.
24. Wei X, Zou G, Zhang H, et al. Implementation of the Chinese national microscopy centre policy: health facility survey in Shandong Province. Tropical Medicine and International Health. 2011;16(7):847–853. doi:10.1111/j.1365-3156.2011.02769.x
25. Yeh CC, Wu SC, Liao CC, Su LT, Hsieh CH, Li TC. Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc. 2011;25(9):2932–2942. doi:10.1007/s00464-011-1645-x
26. Ali A, Mobarak Z, Al-Jumaily M, et al. Cost-utility analysis of antibiotic therapy versus appendicectomy for acute uncomplicated appendicitis. Int J Environ Res Public Health. 2021;18(16):8473. doi:10.3390/ijerph18168473
27. Xue J, Wang H, Li N, et al. Path Analysis of hospitalization expenses of 2164 appendicitis patients at county-level public hospitals in Anhui Province, China. 2020.
28. Xu Y, Zeng P, Zhao H, Wang K, Bian J, He P. Decision tree model of factors influencing hospitalization costs in patients with acute appendicitis. Chongqing Med. 2015;44(31):4403–4405.
29. Wang E, Jootun R, Foster A. Management of acute appendicitis in an acute surgical unit: a cost analysis. ANZ J Surg. 2018;88(12):1284–1288. doi:10.1111/ans.14727
30. Wu J, Counihan T, Eko F, Ryb G, Drager L, Goldwater E. Ideal timing of surgery for acute uncomplicated appendicitis. N Am J Med Sci. 2013;5(1):22–27. doi:10.4103/1947-2714.106186
31. Papandria D, Goldstein SD, Rhee D, et al. Risk of perforation increases with delay in recognition and surgery for acute appendicitis. J Surg Res. 2013;184(2):723–729. doi:10.1016/j.jss.2012.12.008
32. Shakya YR, Shakya S, Napit D, Dahal S, Malla BR. The trend and outcomes of laparoscopic appendectomy for complicated appendicitis in Nepal: a retrospective study from 2014 to 2018 in a University Hospital. Kathmandu Univ Med J. 2019;68(4):306–310.
33. Ruiz-Patiño A, Rey S, Molina G, Dominguez LC, Rugeles S. Cost-effectiveness of laparoscopic versus open appendectomy in developing nations: a Colombian analysis. J Surg Res. 2018;224:33–37. doi:10.1016/j.jss.2017.11.007
34. Adisa A, Kachapila M, Ekwunife C, et al. A prospective, observational cost comparison of laparoscopic and open appendicectomy in three tertiary hospitals in Nigeria. World J Surg. 2023. doi:10.1007/s00268-023-07148-5
35. Fuentes S, Núñez-Alfonsel J, Pradillos-Serna JM, et al. Quality of life in pediatric minimally invasive surgery: cost-utility analysis of laparoscopic versus open appendectomy. J Laparoendosc Adv Surg Tech. 2022;32(2):219–225. doi:10.1089/lap.2021.0495
36. Di Saverio S, Birindelli A, Kelly MD. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11(1). doi:10.1186/s13017-016-0090-5
37. Jaschinski T, Mosch C, Eikermann M, Neugebauer EA. Laparoscopic versus open appendectomy in patients with suspected appendicitis: a systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015;15(1). doi:10.1186/s12876-015-0277-3
38. Yu MC, Feng Y-J, Wang W, Fan W, Cheng H-T, Xu J. Is laparoscopic appendectomy feasible for complicated appendicitis ?A systematic review and meta-analysis. Int J Surg. 2017;40:187–197. doi:10.1016/j.ijsu.2017.03.022
39. Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015 CRD42015016882). Ann Surg. 2017;265(5):889–900. doi:10.1097/SLA.0000000000002039
40. Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018;320(12):1259. doi:10.1001/jama.2018.13201
41. Sippola S, Grönroos J, Tuominen R, et al. Economic evaluation of antibiotic therapy versus appendicectomy for the treatment of uncomplicated acute appendicitis from the APPAC randomized clinical trial. Br J Surg. 2017;104(10):1355–1361. doi:10.1002/bjs.10575
42. Flum DR, Davidson GH, Monsell SE. A randomized trial comparing antibiotics with Appendectomy for Appendicitis. N Engl J Med. 2020;383(20):1907–1919. doi:10.1056/NEJMoa2014320
43. Wang J, Wang P, Wang X, Zheng Y, Xiao Y. Use and prescription of antibiotics in primary health care settings in China. JAMA Intern Med. 2014;174(12):1914. doi:10.1001/jamainternmed.2014.5214
44. Liu Y, Kong Q, Yuan S, van de Klundert J. Factors influencing choice of health system access level in China: a systematic review. PLoS One. 2018;13(8):e0201887.
45. Li Z, Ma Z. Construction and scale development of willingness to utilize primary care services: a study from China. RMHP. 2023;16:2171–2185. doi:10.2147/RMHP.S428369
46. Han L, Zeng L, Duan Y, et al. Improving the applicability and feasibility of clinical practice guidelines in primary care: recommendations for guideline development and implementation. RMHP. 2021;14:3473–3482. doi:10.2147/RMHP.S311254
47. Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi:10.1016/S0140-6736(20)30122-7
48. Fan Z. Differences and Predictors of departure ways for discharge patients in Sichuan province based on Hierarchy Medical System. Jiangxi Univ Chin Med. 2020. doi:10.27180/d.cnki.gjxzc.2020.000005
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.