Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 16
Homocysteine Reduction for Stroke Prevention: Regarding the Recent AHA/ASA 2021 Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack
Authors Brown C , Wang J, Jiang H, Elias MF
Received 18 July 2023
Accepted for publication 6 September 2023
Published 3 October 2023 Volume 2023:16 Pages 895—900
DOI https://doi.org/10.2147/PGPM.S426421
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Craig Brown,1,* Jianhua Wang,2,* Hong Jiang,3,* Merrill F Elias4,*
1Department of Ophthalmology, College of Medicine, University of Arkansas for Medical Sciences, Fayetteville, AR, USA; 2Bascom Palmer Eye Institute, Miller School of Medicine, University of Miami, Miami, FL, USA; 3Bascom Palmer Eye institute, Department of Neurology, Miller School of Medicine, University of Miami, Miami, FL, USA; 4Department of Psychology, University of Maine and Graduate School of Biomedical Sciences and Engineering, University of Maine, Orono, ME, USA
*These authors contributed equally to this work
Correspondence: Craig Brown, 208 E Jason Dr, Fayetteville, AR, 72703, USA, Email [email protected]
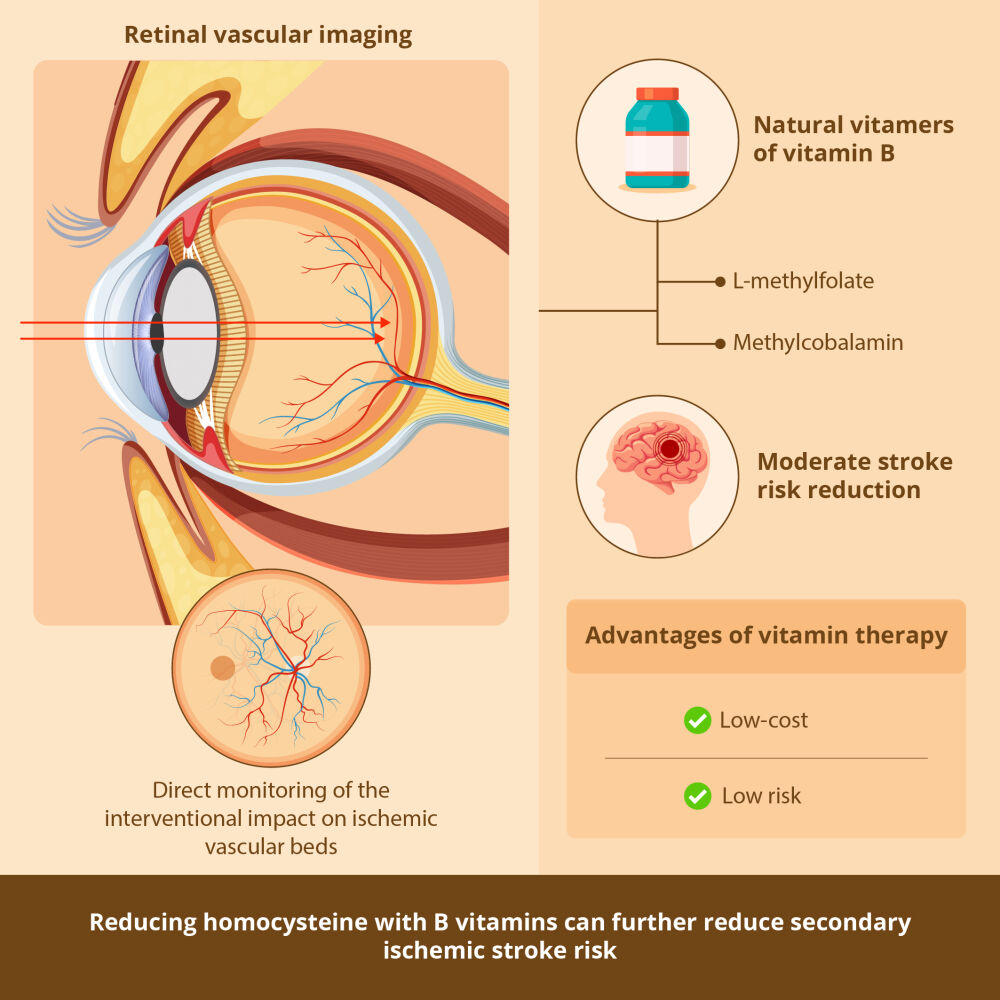
Abstract: Reduction of secondary ischemic stroke risk following an initial stroke is an important goal. The 2021 Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack assembles opportunities for up to 80% secondary stroke reduction. Homocysteine reduction was not included in the recommendations. The reduction of homocysteine with low doses of folic acid has been shown to reduce ischemic stroke and all stroke. This has been obscured by studies using high doses of folic acid and cyanocobalamin in patients with renal failure and Methylenetetrahydrofolate reductase (MTHFR) polymorphisms. The confounding impacts of high dose folic acid and cyanocobalamin toxicity in renal failure and MTHFR C677T subgroups are discussed. New studies show that their toxicity is due to non-bioequivalence to the natural dietary forms, L-methylfolate and methylcobalamin. Low doses of folic acid and cyanocobalamin are safer than high doses for these subpopulations. Even lower toxicity with greater effectiveness for reducing homocysteine is seen with L-methylfolate and methylcobalamin, which are safe at high doses. Retinal vascular imaging is a noninvasive method for evaluating central nervous system (CNS) microangiopathy. A formulation containing l-methylfolate and methylcobalamin has been shown to reduce homocysteine and increase perfusion in diabetic retinopathy. This supports homocysteine intervention for CNS ischemia. Future ischemic stroke intervention studies could benefit from monitoring retinal perfusion to estimate the impact of risk reduction strategies. The omission of a recommendation for homocysteine and secondary stroke reduction through the use of B vitamins should be reconsidered in light of re-analysis of major B vitamin intervention studies and new technologies for monitoring CNS perfusion. We recommend revision of the 2021 Guideline to include homocysteine reduction with low doses of folic acid and cyanocobalamin, or better yet, L-methylfolate and methylcobalamin, making a good clinical guideline better.
Plain Language Summary: The 2021 Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack is incomplete. Reduction of secondary ischemic stroke risk following an initial stroke or TIA is achievable through medication, lifestyle, and nutritional interventions detailed in the Guideline.
The common patient subgroups with renal failure and/or MTHFR C677T polymorphisms are at higher risk for homocysteine elevation, ischemic stroke, and toxicity from excessive folic acid and cyanocobalamin.
The natural forms, L-methylfolate and methylcobalamin, are recommended for these high-risk subpopulations with renal failure and common polymorphisms of the MTHFR and DHFR.
Non-invasive imaging of retinal vessels offers real-time monitoring of small vessel ischemia in stroke patients. A recent study has shown improved retinal perfusion using a cocktail of antioxidants, L-methylfolate, and methylcobalamin. This supports the use of L-methylfolate and methylcobalamin to lower homocysteine and improve CNS perfusion, which would be beneficial for stroke prevention.
We recommend revision of the 2021 Guideline to include homocysteine reduction with low dose folic acid, or better, L-methylfolate and B12 as methylcobalamin.
Keywords: homocysteine, ischemic stroke, l-methylfolate, methylcobalamin, n-acetyl cysteine, renal failure
Graphical Abstract:
Introduction
Interest in homocysteine management is increasing as a result of new studies clarifying the role of homocysteine in small vessel disease of the central nervous system (CNS). Smith and Refsum recently summarized the detailed evidence for homocysteine as a driver of disease, particularly in the CNS.1 Elias and others have discussed this in the context of an opportunity for cardio/neurovascular risk reduction, and particularly for reduction of stroke risk and severity.2–4
Prevention of ischemic stroke after an initial stroke or transient ischemic attack (TIA) is an important and achievable goal. Every reasonable effort should be made to reduce the risk of death and disability, which severely impact the lives of patients and families. The new American Heart Association (AHA) and American Stroke Association (ASA) 2021 Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack is a major step in this direction. It provides extensive well, considered opportunities for up to an 80% future risk reduction of subsequent ischemic stroke.5
Unaccountably, this otherwise excellent guideline failed to recommend homocysteine management for the prevention of stroke after previous stroke or TIA. However, as Spence and Hankey have pointed out, the Guideline wrongly assures the reader that there is no credible evidence that vitamin therapy for homocysteine elevation lowers secondary ischemic stroke risk.4 That is misleading. Several important studies demonstrating the benefits of homocysteine management for stroke reduction were ignored and others misinterpreted, thus leading to false conclusions.1,3,4 This is unfortunate because primary and secondary ischemic stroke prevention is achievable with the use of low-cost, low-risk B-vitamins.3,4,6
Spence et al addressed this omission by reanalysis of key homocysteine studies, revealing that form and dosage matter. They implicate 2 folate polymorphisms: dihydrofolate reductase (DHFR 19-bp deletion) and methylenetetrahydrofolate reductase (MTHFR C677T) affecting the risk of stroke. Toxicity from excessive folic acid and cyanocobalamin administration obscured their considerable benefits for stroke reduction at low dosages. They called for lower dosing or better, the use of the natural nontoxic forms: L-methylfolate and methylcobalamin, which are unaffected by DHFR and MTHFR mutations. For stroke reduction, they recommended low dose folic acid and cyanocobalamin, or higher dose l-methylfolate and methylcobalamin, and the addition of a homocysteine guideline for stroke reduction.3,4
Discussion
Spence and Hankey point out that the new prevention guidelines ignored the rigorous China Stroke Primary Prevention Trial (CSPPT), which found that MTHFR C677T significantly contributed to first stroke and ischemic stroke risk. In this large trial, low-dose folic acid administration reduced ischemic stroke relative risk by 24% with no adverse events.3,4,6
The most recent Cochrane systematic review of randomized controlled trials of homocysteine-lowering interventions found evidence of stroke prevention.7 The likelihood of secondary stroke prevention by the same mechanism as primary stroke prevention is a more-than-reasonable inference until prospective secondary stroke studies are available.3,4 It is misleading to ignore this. Although the magnitude of B-vitamin ischemic stroke risk reduction is moderate, the 80% overall risk reduction achieved by the GSPIS is literally the sum of many such small to moderate risk reductions.5
Spence and Hankey note that the error in the study design of previous large-scale homocysteine trials lies in the false assumption that folic acid and cyanocobalamin are bio-equivalent substitutes for the natural vitamers L-methylfolate and methylcobalamin. In fact, they are beneficial only at low doses, above which toxicity appears. This fact has led to unexpected outcomes and disappointment in vitamin intervention trials targeting homocysteine and stroke for reasons that are only recently being appreciated.3,4
In this paper and in Spence et al,3 evidence and mechanisms are discussed that folic acid and cyanocobalamin, when used at moderate-to-high doses, are harmful and not bio-equivalent to L-methylfolate and methylcobalamin. Folic acid and cyanocobalamin have underappreciated innate toxicities limiting their benefits in three high-risk stroke subgroups: patients with renal failure, with mutations of DHFR and with mutations of MTHFR. These subgroups are associated with deranged homocysteine metabolism and are at higher risk for stroke.3,4,8
House et al9 reported that in the Diabetic Intervention With Vitamins to Improve Nephropathy (DIVINe) trial, increased cardiovascular events occurred in patients with renal impairment who received high doses of folic acid and cyanocobalamin.9 In the previously cited meta-analysis, Spence et al3 reviewed several important randomized trials of no-dose, low-dose, and high-dose B-vitamin interventions using folic acid and cyanocobalamin which yielded an overall 10% reduction of stroke risk.3 They further reported that the subgroup of all patients with exposure to no dose or low dose cyanocobalamin had a 23% reduction in stroke risk, but this fell to a 5% stroke risk reduction with exposure to high doses of cyanocobalamin. More telling, in the subgroup with impaired renal function, high-dose cyanocobalamin yielded a stroke risk increase of 4%, supporting the findings of the DIVINe trial and highlighting the deleterious effects and non-bioequivalence of cyanocobalamin.3,9
On reflection, does it really surprise anyone that cyanide is not well tolerated in patients with renal failure? Yet, renal failure and cyanocobalamin supplementation are so common that they appear to routinely confound outcomes of large-scale B vitamin trials, as Spence et al3 have shown. They reflect common real-world clinical situations.3,4 One could view cyanocobalamin to be a poison pill for renal patients as well as a confounder for stroke prevention studies.
Folic acid non-bioequivalence to natural L-methylfolate is well established. L-methylfolate more readily crosses the blood–brain barrier than folic acid due to a very different pharmacokinetic profile and higher bioavailability.10,11 L-methylfolate is the preferred folate for brain metabolism.11 Folic acid, although effective for lowering homocysteine, fails to lower intra-cellular homocysteine or change the concentrations of other important one carbon metabolites.12 All beneficial folic acid activity derives from the small portion converted to L-methylfolate.3,4,10–12
DHFR and MTHFR reduced function mutations are very common and impair the conversion of supplemented folic acid into active L-methylfolate, further reducing brain folate stores.3,4,10,11 These mutations have well-documented associations with high blood pressure, high homocysteine, increased stroke risk, small vessel disease, and unmetabolized folic acid toxicity.3,4,8,11 Such nutrigenomic disease interactions should be prospectively addressed in future studies. In this regard, the CSPPT China Study evaluating stroke risk reduction, MTHFR status, and low dose folic acid is especially commendable.6 DHFR and MTHFR mutation impairments are easily bypassed, and their pathological consequences are minimized with formulations using the natural forms of the vitamins B2 (Riboflavin), B6 (as pyridoxyl-5-phosphate), B9 (as L-methylfolate), and B12 (as methylcobalamin).3,4,8,11 Thus, folic acid and L-methylfolate are not the same and are not interchangeable. L-methylfolate, with respect to folate polymorphisms, may be viewed as the “universal folate”, safe and effective under all circumstances.
Spence and Hankey and Spence et al summarize good evidence that B-vitamins do reduce all strokes, including ischemic stroke, and most likely secondary ischemic stroke. They conclude that there are sufficient studies to support the safe and economical use of B-vitamins containing low-dose folic acid and low-dose cobalamin for lowering homocysteine to reduce primary and secondary ischemic strokes. They note that, for moderate-to-high dose interventions, better safety and better results will be seen using the natural dietary form of folate (L-methylfolate) and the natural dietary form of B12 (methylcobalamin).3,4
We agree that primary and secondary ischemic stroke ischemic prevention through homocysteine reduction is achievable with the use of low-cost, low-risk B-vitamins and that this should be reflected in an updated ASA/AHA recommendation.4,8
Evidence from Microvascular Studies
Is there clinical support for Spence and Hankey’s analysis that optimized B-vitamins containing L-methylfolate and methylcobalamin may significantly protect from stroke and secondary stroke? Yes. Ischemic stroke is primarily a chronic microangiopathy of the CNS. The retinal vessels are an extracranial part of the CNS small vessel system well situated for frequent noninvasive monitoring of CNS vascular status. Liang et al found that patients with ischemic stroke demonstrated multiple markers of retina ischemia when scanned with ocular coherence tomographic angiography, OCTA.13
A recent study using OCTA and the Retinal Function Imager (RFI) demonstrated that a medical food containing L-methylfolate and methylcobalamin, coupled with other B vitamins and antioxidants, reversed microangiopathic changes in patients with early diabetic retinopathy and the common MTHFR gene variants.14
Liu et al14 demonstrated that the optimized B-complex medical food, Ocufolin®, improved retinal perfusion and hemodynamics in diabetic retinopathy patients with MTHFR gene variants. Liu et al15 further demonstrated improvement in microvascular density over the 6-month trial. Schmidl et al16 demonstrated that the same formula lowered homocysteine in diabetics by 30%.14–16
As a window into the pathophysiology of CNS small vessel disease, the measurement of retinal vessel density and perfusion indices provides easy and inexpensive test beds for intervention efficacy. It is reasonable to suppose that improving CNS small vessel hemodynamics and perfusion will reduce ischemic stroke risk.
Liu et al’s studies provide clinical and mechanistic support for Spence and Hankey’s conclusion that optimal B-vitamin preparations containing L-methylfolate and methylcobalamin have the potential for even greater prevention of secondary ischemic stroke by avoiding toxicity and improving small vessel structure and function.14,15
Recommendations
We agree with Spence and Hankey’s recommendation to revise the Hyperhomocysteinemia section of the AHA/ASA 2021 Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack to include the treatment of homocysteine with optimized B-vitamins.4 We base our support on the reasons given by Spence and Hankey, as well as new research showing improved small vessel microangiopathy and perfusion following the administration of optimized B-vitamins with L-methylfolate and methylcobalamin.4,13–16
We urge future studies to examine primary and secondary ischemic stroke prevention utilizing the natural forms of folate and B12 (L-methylfolate and methylcobalamin), rather than the more toxic forms (folic acid and cyanocobalamin). We believe that further ischemic stroke reduction benefits will be achieved through improved CNS hemodynamics and perfusion. We finally suggest that future stroke intervention studies should include noninvasive measurements of retinal vessel density and blood flow as windows for monitoring ischemic cerebral small vessel density, hemodynamics, and perfusion. Retinal imaging is safe, simple, and inexpensive, as are the natural forms of B-vitamins: L-methylfolate and methylcobalamin. This is an opportunity to make a good guideline even better.
Abbreviations
AHA, American Heart Association; ASA, American Stroke Association; CNS, Central Nervous System; CSPPT, China Stroke Primary Prevention Trial; DHFR, dihydrofolate reductase; DIVINe Trial, Diabetic Intervention With Vitamins to Improve Nephropathy Trial; MTHFR, methylenetetrahydrofolate reductase; OCTA, Ocular Coherence Tomographic Angiography; RFI, Retinal Function Imager; TIA, transient ischemic attack.
Disclosure
Dr Brown is a managing partner for Global Healthcare Focus, the manufacturers of Ocufolin®, a medical food used to address retinal ischemia. In addition, Dr Craig Brown has the patents: US 8822431B2, US 9770464B2, US 10278987B2, US 11,351,189; and Canada 2836445, and 2876169. All are licensed to Global Healthcare Focus. The authors report no other conflicts of interest in this work.
References
1. Smith AD, Refsum H. Homocysteine - from disease biomarker to disease prevention. J Intern Med. 2021;290(4):826–854. doi:10.1111/joim.13279.
2. Elias MF. Reclaiming the importance of homocysteine as a marker of cardiovascular and neurologic disease. J Intern Med. 2021;290(5):1098–1099. doi:10.1111/joim.13305.
3. Spence JD, Yi Q, Hankey GJ. B vitamins in stroke prevention: time to reconsider. Lancet Neurol. 2017;16(9):750–760. doi:10.1016/S1474-4422(17)30180-1
4. Spence JD, Hankey GJ. Problem in the recent American heart association guideline on secondary stroke prevention: b vitamins to lower homocysteine do prevent stroke. Stroke. 2022;53(8):2702–2708. doi:10.1161/STROKEAHA.122.038640
5. Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American heart association/American stroke association. Stroke. 2021;52(7):e364–e467. doi:10.1161/STR.0000000000000375
6. Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT Randomized Clinical Trial. JAMA. 2015;313(13):1325–1335. doi:10.1001/jama.2015.2274
7. Martí-Carvajal AJ, Solà I, Lathyris D, Dayer M. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev. 2017;8(8):CD006612. doi:10.1002/14651858.CD006612.pub5
8. Elias MF, Brown CJ. Medical foods for lowering homocysteine in hypertensive patients. J Clin Hypertens. 2023;25(1):111–114. doi:10.1111/jch.14608
9. House AA, Eliasson M, Cattran DC, et al. Effect of B-vitamin therapy on progression of diabetic nephropathy: a randomized controlled trial. JAMA. 2010;303(16):1603–1609. doi:10.1001/jama.2010.490
10. Willems FF, Boers GH, Blom HJ, Aengevaeren WR, Verheugt FW. Pharmacokinetic study on the utilization of 5-methyltetrahydrofolate and folic acid in patients with coronary artery disease. Br J Pharmacol. 2004;141(5):825–830. doi:10.1038/sj.bjp.0705446
11. Stover PJ, Durga J, Field MS. Folate nutrition and blood-brain barrier dysfunction. Curr Opin Biotechnol. 2017;44:146–152. doi:10.1016/j.copbio.2017.01.006
12. Smith DE, Hornstra JM, Kok RM, Blom HJ, Smulders YM. Folic acid supplementation does not reduce intracellular homocysteine, and may disturb intracellular one-carbon metabolism. Clin Chem Lab Med. 2013;51(8):1643–1650. doi:10.1515/cclm-2012-0694
13. Liang Y, Liu B, Xiao Y, et al. Retinal neurovascular changes in patients with ischemic stroke investigated by optical coherence tomography angiography. Front Aging Neurosci. 2022;14:834560. doi:10.3389/fnagi.2022.834560
14. Liu Z, Jiang H, Townsend JH, Wang J. Improved Retinal Microcirculation in Mild Diabetic Retinopathy Patients Carrying MTHFR Polymorphisms Who Received the Medical Food, Ocufolin®. Clin Ophthalmol. 2022;16:1497–1504.
15. Liu Z, Jiang H, Townsend JH, Wang J. Effects of Ocufolin on retinal microvasculature in patients with mild non-proliferative diabetic retinopathy carrying polymorphisms of the MTHFR gene. BMJ Open Diabetes Res Care. 2021;9(1):e002327. doi:10.1136/bmjdrc-2021-002327
16. Schmidl D, Howorka K, Szegedi S, et al. A pilot study to assess the effect of a three-month vitamin supplementation containing l-methylfolate on systemic homocysteine plasma concentrations and retinal blood flow in patients with diabetes. Mol Vis. 2020;26:326–333.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
