Back to Journals » Vascular Health and Risk Management » Volume 18
Home Blood Pressure Measurement and Self-Interpretation of Blood Pressure Readings During Pregnancy: Hy-Result e-Health Prospective Study
Authors Postel-Vinay N, Shao JD, Pinton A , Servais A, Gebara N, Amar L
Received 9 December 2021
Accepted for publication 5 April 2022
Published 15 April 2022 Volume 2022:18 Pages 277—287
DOI https://doi.org/10.2147/VHRM.S350478
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mirna N Chahine
Nicolas Postel-Vinay,1,2 Jiali-Delphine Shao,3 Anne Pinton,4 Aude Servais,5 Nicole Gebara,1 Laurence Amar1
1Hypertension Unit, ESH Excellence Center, Hôpital Européen Georges Pompidou, APHP, Paris, France; 2Hospital at Home, Fondation Santé Service, Levallois, France; 3Faculté de médecine de l’Université Paris Saclay, Le Kremlin Bicêtre, France; 4Department of Obstetrics and Gynecology, Trousseau Hospital, APHP, Sorbonne University, Paris, France; 5Nephrology and Transplantation Department, Necker Hospital, APHP, Paris, France
Correspondence: Nicolas Postel-Vinay, Email [email protected]
Introduction: Hy-Result is a rule management system designed to help patients to be compliant with the home blood pressure measurement (HBPM) monitoring schedule and to understand their BP readings. The aim of the Hy-Result e-Health prospective study is to evaluate the practice and experience of women using the Hy-Result coaching app for self-interpretation of BP readings during and after pregnancy.
Methods: Participants were asked to: i) measure their BP at home; ii) use the Hy-Result app and send their PDF report to the researcher; iii) answer anonymously to 3 online independent questionnaires (Q).
Results: A total of 107 women accepted to measure their BP and use the app. Among them 82 (77%) performed HBPM and used successfully the system and 72 (88%) shared to the investigator their PDF report by email. Of these, 95% declared the software was “easy” or “very easy” to use; 93% believe the software helps them to monitor their BP more effectively (74% agree, 18% somewhat agree); 94% that the color code classification was “clear”; 76 (93%) affirmed that the app helped them when consulting their physician for their BP evaluation. Majority (87%) perceived the software to be reliable. Furthermore, 71 (87%) said they trust the system and 51 (62%) declared that performing HBPM and self-interpret their readings was “reassuring” whereas 6 (7%) felt that it was “a concern”.
Conclusion: This study shows that the majority (88%) of pregnant women performed HBPM and successfully used the Hy-Result software for self-interpretation of the BP readings. The use of the validated Hy-Result system by pregnant women may thus be recommended in common practice by healthcare professionals and patient associations.
Keywords: hypertension, home blood pressure monitoring, health informatics, pregnancy, e-health, telemedicine, self-monitoring
Introduction
Hypertensive disorders in pregnancy affect 5–10% of pregnancies worldwide and remain a major cause of maternal, fetal, and neonatal morbidity and mortality.1 Maternal risks include placental abruption, stroke, multiple organ failure, and disseminated intravascular coagulation. The fetus is at high risk of intrauterine prematurity, growth retardation, and intrauterine death, seen in 27%, 25%, and 4% of cases of pre-eclampsia respectively.2 Blood pressure (BP) should be measured at every antenatal visit. However, even frequent antenatal consultations cannot predict nor identify fulminant preeclampsia because its onset and progression can be rapid and often, asymptomatic. Thus, the “European Society of Hypertension (ESH) Working Group on Blood Pressure Monitoring and cardiovascular variability” highlights the substantial role of home BP monitoring (HBPM) for early diagnosis and management of pre-eclampsia.3 The ESH Guidelines for the management of arterial hypertension recommend Home Blood Pressure Monitoring (HBPM) in pregnancy, a well-accepted method that allows the diagnosis of white coat hypertension.4 Measurements at home during pregnancy appear to be similar to those in clinic; thus, management thresholds can be similar. Despite this, white-coat hypertension is still commonly diagnosed.5
When asked about their preferences, many women choose to self-monitor their BP during pregnancy. Physicians should therefore encourage them and provide them with improved information regarding HBPM to give them a better knowledge about their BP and empowered them in their own care.3,6 Therefore, self-management is a useful way to improve detection and BP control.
Nowadays, in this digital technology era, start-ups are developing interactive digital tools that give the general population access to medical information in order to improve treatment compliance and health behavior. New tools, available online or via smartphones applications (apps), are even offering personalized feedback to patients. With mHealth, new possibilities exist to improve self-monitoring and allow pregnant women to be more empowered in their own care and wellness.7,8 However, despite their potential advantages, these applications are two-edged swords and very little is known about the reliability of many algorithms that remain a trade secret.9
A systematic review published in 2015 identified around 850-anglophone smartphone apps devoted to hypertension.10 An analysis of the first 107 smartphone apps developed for hypertension showed that, although intended primarily for the general population, only three of them were developed by healthcare professionals. The remaining are turning smartphones into medical devices without any medical or governmental control under the pretext that they are developed within the heading of ‘fitness’ or “wellness’.11 Many users do not assess the validity and reliability of the apps” content with their physicians. In our experience, a third of women using an mHealth app during pregnancy monitored their BP at home, but the majority did not seek any medical advice.12
Thus, we need to provide pregnant women with trustworthy apps for hypertension based on scientific research and established guidelines.13,14 A good example, the Hy-Result system, a validated software that analyses HBPM and provides users with a report that interprets their BP measurements based on algorithm according to the ESH 2018 international guidelines.13 In 2020, a patient’s perception study showed that most of the users described Hy-Result as an easy-to-use and useful tool, but pregnant women were excluded from the evaluation.14 The aim of this study is to evaluate the practice and the experience women using the Hy-result system during and after pregnancy.
Materials and Methods
Hy-Result App
Hy-Result is a rule management system designed to help patients to be compliant with the HBPM protocol and to understand their BP readings. This coaching app generates a patient-friendly report according to the ESH recommended BP thresholds [1,3]. Reliability of the system was evaluated through a clinical study published in 2016.13
Patients must follow several steps: i) Self-measure their BP at home; ii) report them in an online form along with their medical profile; iii) click the icons “calculate” and “report” to obtain the automated interpretation of BP readings and personalized text messages, generated by the Hy-Result algorithm. The mean BP for the whole self-measurement sequence is displayed as numerical and color-coded results (grey, green, orange, and red, referring to the degree of the hypertension control, with red being the worst). The final report (graphics + text messages) can then be downloaded and saved in a portable document format (PDF) allowing it to be sent by email, printed, or transferred to a computer, smartphone, or tablet. This report indicates: i) the total number of measurements; ii), the overall systolic BP average and the diastolic BP average (overall, morning and evening); iii) the daily averages in graph form (see screenshot Figure 1). It confirms the patient’s compliance with the self-measurement recommended monitoring schedule. This app is free, and available in French and English at www.hy-result.com.
 |
Figure 1 Screenshot of the Hy-Result report. |
Study Design and Data Collection
We conducted a prospective descriptive, multicentric study between May 2019 and April 2021 in France. Overall, 10 centers were included: 5 maternity units, 2 European Society Hypertension (ESH) excellence hypertension centers, 1 primary care center, 2 patients’ associations network. We recruited 107 pregnant women, aged over 18-years-old, who agreed to perform HBPM and send their BP reports to the researcher. The exclusion criteria were: having no internet access or personal email, an arm circumference > 32 cm and having arrhythmia or visual/cognitive impairment that prevents the correct use of the sphygmomanometer.
Participants were asked to: i) measure their BP at home (3 measurements in the morning and 3 in the evening over a minimum of 3 consecutive days (maximum 7 days), while sitting, after a rest period of at least 10 minutes; ii) send their PDF report to the researcher; iii) answer anonymously 3 online independent questionnaires (Q) with closed questions. In this observational work, the protocol left users free to continue self-monitoring their BP after childbirth; some women chose to do so on their own.
Each questionnaire, developed in french based on expert knowledge of HBPM, was independent from the other, without any tracking system, for anonymity purpose. Q1 validated the inclusion to the study and summed the HBPM past history; Q2 detailed sociodemographic characteristics and past medical and obstetrical history. It evaluated also HBPM experience using Hy-Result system during pregnancy; Q3, completed after delivery, tackled the medical practice and BP evaluation and control in the post-partum.
There were 2 researchers (N.P.-V, D.S.) in this study that had the role of only retrieving the PDF files and extracting the data from the questionnaires without having any medical intervention. Women could withdraw from the study at any time. For regulatory reasons, the investigators were not allowed access to the medical files and the participants were free to share their BP readings with their treating physician or midwife.
Statistical Analysis
Statistical analysis was performed using the IBM SPSS Statistics software, version 26. Categorical variables were summarized as frequency and percentage. Continuous variables were presented as means, standard deviation, median, minimum and maximum.
Ethical Consideration
The oral consent was obtained by the healthcare team after information about the study. Women confirmed their agreement by an email sent to the researcher. The “Ile de France II” People Protection Committee approved the protocol (number 2012-10-18- MS1).
Results
Among the 107 women (mean age 34.2 years old ± 4.7), (see Table 1, Baseline Characteristics) who accepted to measure their BP, 82 (77%) responded to Q2 after using successfully the Hy-Result system. Among them, 24 (29%) declared having a hypertension treatment during pregnancy (see Table 2). Seventy-two participants (88%) shared to the investigator their PDF report by email. At the end of the study 64 post-partum Q3 were collected (see Figure 2, flow chart).
 |
Table 1 Included Population, Baseline Characteristics |
 |
Table 2 Description of the Participants Who Responded to Q 2 (N = 82) |
 |
Figure 2 Flow chart of included participants. |
Out of the 107 pregnant women included, 76% declared that they had already monitored their BP before the survey, with 56% having done so before the current pregnancy. Out of these, 41% decided to control it on their own initiative, whereas 59% did it at the request of their treating physician or midwife.
Compliance to HBPM Monitoring Schedule
Out of the 72 e-mailed Hy-Result PDF report, 60 patients (83%) measured their BP 3 times in the morning, 3 times in the evening, for at least 3 days as recommended by ESH guidelines. The mean number of consecutive days of monitoring was 5 (CI 95% 4.57–5.43); 12 participants (17%) did not respect the recommended monitoring schedule. Figure 3 shows the number of participants that were compliant (6 measurements per day) or not, according to the total number of consecutive days count during which HBPM was performed. Sixty-four women answered Q3 after giving birth. Among them, 48 (75%) shared their BP reports with their doctor or midwife (even when their measurements were in “Green”; 5 (8%) only when their measurements were in “Orange” or “Red”). After delivery, 31 women (48%) continued to self-monitor their BP, half of them upon their physician’s request and the others on their own initiative.
 |
Figure 3 Compliance according to the consecutive number of days of HBPM. |
Experience, Comprehension and Opinion
Women’s experience is analyzed with Q2 responses. Seventy-eight women (95%) considered the app “easy” or “very easy” to use and 76 (93%) confirmed that the app helped them when consulting their physician for their BP evaluation. Furthermore, 71 (87%) said they trusted the system and perceived the software to be reliable (Figure 4) and 51 (62%) declared that performing HBPM and self-interpreting their readings was “reassuring” whereas 6 (7%) felt that it was “a concern”.
 |
Figure 4 Experience and comprehension regarding the Hy-Result system. |
The majority of women (93%) agreed or partly agreed that the software helped them to monitor their BP more effectively (Figure 5). Of the total number of women enrolled in the study (included lost to follow-up) 77% of them performed HBPM and used the software.
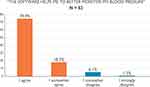 |
Figure 5 Women’s opinions regarding the Hy-result system’s usefulness. |
Impact on Communication with the Healthcare Professional
When analyzing the responses to Q 2, we found that 56 women (68%) declared that “the software helps me talk to my doctor or midwife about my BP readings”; 26 (32%) felt that it “has no impact on communication with my healthcare professional”. No women found that the software negatively interfered with the dialogue. Color-codes and text messages were considered to be “clear” or “very clear” for 82 users (94%); only 3 women (4%) did not understand the instructions generated by the system.
When seeing the green color-code, 70 women (85%) were reassured and did not contact their doctor; 10 patients (12%) planned to visit their doctor (whether they understood the text messages or not) and 2 (2%) did not understood the text messages and did not contact their doctor. If BP measurements were in the red zone, all the users would seek medical advice: 33 (40%) would go immediately to the emergency department, 42 (51%) would visit their physician within 48 hours and 7 (9%) within the week (Figure 6).
 |
Figure 6 Participants’ reaction toward green ranked readings. |
 |
Figure 7 Participants’ opinion about the usefulness of the software. |
Anxiety
In this study, we asked patients not only to self-measure their BP, but also to interpret their BP readings. Hence, we were interested to see if this task generated anxiety. Q2 responses showed that 7% reported feeling anxious whereas 62% were reassured.
Discussion
Recommending the use of the validated Hy-Result software is feasible in a clinical setting and daily life conditions among pregnant women. These results converge with those obtained previously with hypertensive patients or in a population using the Hy-Result app linked to their BP monitor but from which pregnant women were excluded.13,14 A large majority of responders declared that Hy-Result software helps to monitor their BP more effectively. Even with the hypothesis that the 25 women lost to follow-up would have reported a negative opinion about self-monitoring of BP with the software, the favorable opinions would remain in the majority: 76/107 (72%) of the participants would consider the software useful (Figure 7).
Digital Care Pathway
In our study, the majority of women consider that the app is helpful. In fact, previous studies showed that the BP measures helps patients to self-interpret their results and may allow them to correctly self-titrate their treatment.15–17 When the means of the BP readings are in green based on the Hy-Result algorithm, 85% of women perceive the message as reassuring and do not contact their doctor or midwife (Figure 6). A study published in 2018 showed that HBPM had the potential to reduce the number of hospital visits.18 In this perspective, we expect that the Hy-Result app could improve BP surveillance and antenatal care pathway. However, when the Hy-Result BP classification appears in “Red”, all participating women understood that they should seek medical advice. Our study was not designed to confirm if they had informed their physicians/mid-wife or not. Therefore, the potential impact of the Hy-Result App on the medical pathway with an evaluation of an action plan is being studied in an ongoing study.
The percentage of women who communicated their results to the physicians was more than 80% if we consider only consider the Q3 subgroups. It remains significant even if estimated from the initial inclusion population (62%) which has a practical clinical impact for current practice. These rates are higher than what was found in our previous work in chronic hypertensive patients or in pregnant women, where 23% of participants used Hy-Result app linked to a connected BP monitoring by their self-motivation without any medical advice.13,14 In this study we explain this higher rate by the fact that the use of the Hy-Result software was recommended by the doctor or midwife and was not found by the patients themselves on the web. This medical recommendation improves compliance and confidence in the tool as shown in other studies.19,20
Compliance to Monitoring Schedule
Having a reliable HBPM is crucial for a correct management. However, the monitoring schedule and protocol may not be respected by patients or clearly explained by health professionals. According to a French study published in 2011, only 17% of general practitioners teach their patients how to perform correct and standardized HBPM.21 By using the Hy-Result coaching app, most of the women respected the monitoring schedule (83% of the participants did respect 3 consecutive measurements in the morning, 3 in the evening, for at least 3 days).
Anxiety
Several studies show that HBPM is feasible during pregnancy and reduces anxiety by creating a sense of reassurance and empowerment.22–24 A randomized comparative study24 found a lower level of anxiety with self-measurement, versus usual follow-up in consultation. In our study, we asked patients not only to self-measure their BP, but also to interpret their BP readings. This additional task did not seem to increase their anxiety.
Hy-Result and BP Thresholds in Pregnancy
International guidelines lack consensus regarding BP thresholds in pregnant women. A recent review of the literature suggests that HBPM thresholds for pregnant women should be the same as office BP because they assume that there would be no difference between measurements at home and in consultation settings.5 The threshold for switching from green to orange for the Hy-Result algorithm is BP> 135/85, following the European Society of Hypertension (ESH) and the Canadian college guidelines.1,3,25 For hypertension during pregnancy the French society of hypertension (SFHTA) guidelines recommend starting treatment when the office BP ≥ 160/110mmHg, is classified as a “Red” code by the Hy-Result algorithm. The targeted BP after treatment is ≤160mmHg for Systolic BP and between 85 to 100mmHg for diastolic BP.26 To date, the Hy-Result algorithm does not integrate these recommendations, but the app gives this text message: “according to the CHIPS study a DBP under treatment between 80 and 85mmHg is associated with reduced complications compared to higher diastolic BP levels”.27 As suggested by the ESH guidelines, more studies are needed to define the BP target thresholds.1,3
Study Strengths and Limitations
This prospective study focuses on the contribution of new information and communication technologies in the practice of HBPM and self-interpretation of BP readings during pregnancy. To our knowledge, this is the first study that evaluated a patient-centered model and clinical self-decision support tool in pregnant women. Recent studies mainly focus on remote monitoring and not self-management.28–30 However, the present study has some limitations. First, the self-reporting bias. Although women were recruited from different centers, results cannot be generalized to the whole of the pregnant women’s population. All the women included in the study (except 2) had a computer or a smartphone. This high rate constitutes a selection bias. Second, because the responses were anonymous, we could not investigate why women quit the survey after responding to Q1. In addition, each patient responded to each questionnaire separately. Thus, the collection of the results was done independently and we could not identify the patients’ identity nor analyze the results according to the BP levels, age or pregnancy stages. These correlations should be done in a future work.
Perspectives
Hy-Result coaching app advocate seeking medical advice in the case of elevated measurements. Self-measurement may reduce the number of unnecessary consultations but evaluation of the clinical impact of self-interpretation of the readings with Hy-Result coaching app on the care pathway remains to be done in daily conditions. The current version of the software includes only the arterial BP parameter without taking into consideration other major clinical signs in preeclampsia (eg pain, proteinuria) which will help early diagnoses of pre-eclampsia. They will be taken into account in a future version of the algorithm. As stated in the PDF reports, the software’s automated analysis does not replace that of a physician or midwife. The text-messages are not medical advice but are only a support in self-management. Over the last years, the use of digital health for home-based monitoring and telemonitoring is increasing to replace antenatal hospital admissions.31 We suggest considering the self-management Hy-Result system as a first step preceding telemonitoring or medical consultation if necessary.
Conclusion
This study shows that the majority (88%) of pregnant women performed HBPM and successfully used the Hy-Result software for self-interpretation of the BP readings. The use of the validated Hy-Result system by pregnant women may thus be recommended in common practice by healthcare professionals and patient associations.
Acknowledgments
We would like to thank the Pre-eclampsia Association, La Fondation de l’avenir, Fondation Robert Debré pour la recherche médicale and the North French Cardiology Foundation, Pas de Calais/Picardie).
Disclosure
Nicolas Postel-Vinay is one of the academic authors of the Hy-Result system. Professor Laurence Amar reports Fees for traveling for a medical presentation from Ipsen, and Board on hypertension control from Servier, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165–3241. doi:10.1093/eurheartj/ehy340
2. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–e333. doi:10.1016/S2214-109X(14)70227-X
3. Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the Working Group on blood pressure monitoring and cardiovascular variability of the European Society of Hypertension. J Hypertens. 2021;39(9):1742–1767. doi:10.1097/HJH.0000000000002922
4. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi:10.1093/eurheartj/ehy339
5. Tucker KL, Bankhead C, Hodgkinson J, et al. How do home and clinic blood pressure readings compare in pregnancy? Hypertension. 2018;72(3):686–694. doi:10.1161/HYPERTENSIONAHA.118.10917
6. Tucker KL, Hodgkinson J, Wilson HM, et al. Current prevalence of self-monitoring of blood pressure during pregnancy: the BUMP Survey. J Hypertens. 2021;39(5):994–1001. doi:10.1097/HJH.0000000000002734
7. Hughson J-AP, Daly JO, Woodward-Kron R, et al. The rise of pregnancy apps and the implications for culturally and linguistically diverse women: narrative review. JMIR Mhealth Uhealth. 2018;6(11):e189. doi:10.2196/mhealth.9119
8. Wang N, Deng Z, Wen LM, et al. Understanding the use of smartphone apps for health information among pregnant Chinese women: mixed methods study. JMIR Mhealth Uhealth. 2019;7(6):e12631. doi:10.2196/12631
9. Postel-Vinay N, Bobrie G, Savard S, et al. Home blood pressure measurement and digital health: communication technologies create a new context. J Hypertens. 2018;36(11):2125–2131. doi:10.1097/HJH.0000000000001860
10. Burke LE, Ma J, Azar KMJ, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132(12):1157–1213. doi:10.1161/CIR.0000000000000232
11. Kumar N, Khunger M, Gupta A, Garg N. A content analysis of smartphone- based applications for hypertension management. J Am Soc Hypertens. 2015;9(2):130–136. doi:10.1016/j.jash.2014.12.001
12. Postel-Vinay N, Jouhaud P, Bobrie G, et al. Home blood pressure measurement and mobile health app for pregnant and postpartum women. J Hypertens. 2019;37:e280. doi:10.1097/01.hjh.0000573576.89014.cb
13. Postel-Vinay N, Bobrie G, Ruelland A, et al. Automated interpretation of home blood pressure assessment (Hy-Result software) versus physician’s assessment: a validation study. Blood Press Monit. 2016;21(2):111–117. doi:10.1097/MBP.0000000000000162
14. Postel-Vinay N, Steichen O, Pebelier E, et al. Home blood pressure monitoring and e-Health: investigation of patients’ experience with the Hy-Result system. Blood Press Monit. 2020;25(3):155–161. doi:10.1097/MBP.0000000000000436
15. Steurer-Stey C, Zoller M, Chmiel Moshinsky C, Senn O, Rosemann T. Does a colour-coded blood pressure diary improve blood pressure control for patients in general practice: the CoCo trial. Trials. 2010;11:38. doi:10.1186/1745-6215-11-38
16. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376(9736):163–172. doi:10.1016/S0140-6736(10)60964-6
17. McManus RJ, Little P, Stuart B, et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. 2021;372:m4858. doi:10.1136/bmj.m4858
18. Perry H, Sheehan E, Thilaganathan B, Khalil A. Home blood-pressure monitoring in a hypertensive pregnant population. Ultrasound Obstet Gynecol. 2018;51(4):524–530. doi:10.1002/uog.19023
19. Peng W, Kanthawala S, Yuan S, Hussain SA. A qualitative study of user perceptions of mobile health apps. BMC Public Health. 2016;16(1):1158. doi:10.1186/s12889-016-3808-0
20. Vo VA, Auroy L, Sarradon-Eck A. Patients’ perceptions of mHealth apps: meta-ethnographic review of qualitative studies. JMIR Mhealth Uhealth. 2019;7(7):e13817. doi:10.2196/13817
21. Boivin JM, Tsou-Gaillet TJ, Fay R, et al. Influence of the recommendations on the implementation of home blood pressure measurement by French general practitioners: a 2004–2009 longitudinal survey. J Hypertens. 2011;29(11):2105–2115. doi:10.1097/HJH.0b013e32834b7efb
22. Tucker KL, Taylor KS, Crawford C, et al. Blood pressure self-monitoring in pregnancy: examining feasibility in a prospective cohort study. BMC Pregnancy Childbirth. 2017;17(1):442. doi:10.1186/s12884-017-1605-0
23. Hinton L, Tucker KL, Greenfield SM, et al. Blood pressure self-monitoring in pregnancy (BuMP) feasibility study; a qualitative analysis of women’s experiences of self-monitoring. BMC Pregnancy Childbirth. 2017;17(1):427. doi:10.1186/s12884-017-1592-1
24. Pealing LM, Tucker KL, Mackillop LH, et al. A randomised controlled trial of blood pressure self-monitoring in the management of hypertensive pregnancy. OPTIMUM-BP: a feasibility trial. Pregnancy Hypertens. 2019;18:141–149. doi:10.1016/j.preghy.2019.09.018
25. Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P; SOGC Hypertension Guideline Committee. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014;36(7):575–576. doi:10.1016/S1701-2163(15)30533-8.
26. Mounier-Vehier C, Amar J, Boivin J-M, et al. Hypertension and pregnancy. Expert consensus statement from the French Society of Hypertension, an affiliate of the French Society of Cardiology. Presse Med. 2016;45(7–8 Pt 1):682–699. doi:10.1016/j.lpm.2016.05.012
27. Magee LA, von Dadelszen P, Rey E, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372(5):407–417. doi:10.1056/NEJMoa1404595
28. Dougall G, Franssen M, Tucker KL, et al. Blood pressure monitoring in high-risk pregnancy to improve the detection and monitoring of hypertension (the BUMP 1 and 2 trials): protocol for two linked randomised controlled trials. BMJ Open. 2020;10(1):e034593. doi:10.1136/bmjopen-2019-034593
29. Chappell L, Tucker K, Yu L-M, et al. Bump Study Group. Self-monitoring of blood pressure in women with pregnancy hypertension: the BUMP2 multicentre randomised controlled trial. J Hypertens. 2021;39:e9. doi:10.1097/01.hjh.0000744452.18575.74
30. Van den Heuvel JFM, Lely AT, Huisman JJ, et al. SAFE@HOME: digital health platform facilitating a new care path for women at increased risk of preeclampsia – a case-control study. Pregnancy Hypertens. 2020;22:
31. Van den Heuvel JFM, Ayubi S, Franx A, et al. Home-based monitoring and telemonitoring of complicated pregnancies: nationwide Cross-Sectional Survey of current practice in the Netherlands. JMIR mHealth uHealth. 2020;8(10):e18966. PMID: 33112250; PMCID: PMC7657725. doi:10.2196/18966
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
