Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
HIV Positivity Disclosure Among Children Living with HIV/AIDS and Currently on HAART in Dessie, Northeast Ethiopia
Authors Chanie MG , Abebe A, Muche A , Worku N
Received 3 February 2022
Accepted for publication 18 September 2022
Published 7 October 2022 Volume 2022:14 Pages 461—472
DOI https://doi.org/10.2147/HIV.S356507
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Muluken Genetu Chanie,1 Abenezer Abebe,2 Amare Muche,3 Nigusu Worku4
1Department of Health Systems and Policy, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Pediatrics, Dessie Specialized Hospital, Dessie, Ethiopia; 3Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 4Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Nigusu Worku, Email [email protected]
Background: Disclosure of HIV/AIDS positive test result to children is a continuing routine problem in the health care setting. Some of the families as well as the health care workers are negligent to inform children of their HIV status. This study was aimed at identifying the prevalence of HIV-positivity disclosure and the factors among 6– 15-year-old children currently on HAART in Dessie, Ethiopia.
Methods: A facility based cross-sectional study design was performed in Dessie from January 21 to March 12, 2020 among 346 parents/caregivers with children living with HIV and currently on HAART. The data were collected using pre-tested, structured and self-administered questionnaires. The collected data were entered into Epi info v.7.1 and exported into SPSS version 23 for further analysis. Binary and multivariable logistic regression was employed and statistically significant factors were identified at 95% CI and at p-value < 0.05.
Results: HIV positivity disclosure was found to be 29.2% (26.3– 34.7%). Being widowed mothers/caregivers, 11– 15-year-old children, child received support from NGOs and having a mother with a negative HIV test were found to be statistically significant factors for disclosure.
Conclusion: The overall HIV positivity disclosure to children living with HIV was found to be low in contrast to the WHO standard. In other ways, it was comparable with the Ethiopian figures. Health workers and managers need to focus on strengthening child support, make known the maternal/caregivers’ HIV status, and child age specific effective interventions to improve disclosure of HIV positivity status for children living with HIV for better ART adherence and treatment outcomes.
Keywords: HIV positivity, disclosure, children living with HIV/AIDS, HAART, Dessie
Background
Worldwide, more than 76 million people have lived with HIV/AIDS, and it has resulted in over 35 million deaths since its emergence. Globally, by the end of 2018, out of 37.9 million people living with HIV/AIDS, approximately 3.4 million children under 15 years old were found to be living with HIV/AIDS.1 Sub-Saharan Africa accounts to nearly 2/3 of the global HIV/AIDS cases. Around 90% of children living with HIV live in sub-Saharan Africa where, out of this, 2% are in Ethiopia.1,2
In several highly burdened countries, HIV/AIDS is increasingly harming the health of children and negatively affecting hard-won gains in child life.3 The exact prevalence of HIV in children is not well known.4,5 Antiretroviral treatment (ART) was started in 2003 and as a free therapy in 2005. According to the WHO and UNICEF 2018 report, 613,000 Ethiopians were found to be HIV infected, however, only 436,000 were taking antiretroviral (ARV) drugs.6
Expanding access to HAART brought a rapid change in the global HIV/AIDS prevalence. As a result, HIV/AIDS associated deaths are declining. In LMICs from 2002 to 2012, HAART prevented an estimated 4.2 million deaths, and the number of children (<15 years), taking ART had increased from 566,000 in 2011 to 630,000 in 2012.7 A survey conducted in many African countries indicated that more than 50% of the participants were found to be infected with HIV, however, they did not know their HIV status.8,9 HIV/AIDS positivity disclosure is a crucial issue for arguments because of its linkage to privacy and confidentiality of humanity. Therefore; ending discrimination and stigma against people living with HIV/AIDS is critical.10 Because of HAART, HIV infected children are surviving to adulthood. Although, the benefits of HIV/AIDS positivity disclosure, and understanding how parents and health care workers communicate with children to maximize the positive psychosocial and clinical benefits is emerging.10,11 In Africa, studies showed that the prevalence of children infected with HIV/AIDS positivity disclosure is low extending from 1.7% to 28%.6,9,11,12 A study in Ethiopia showed, HIV/AIDS positivity disclosures were heterogeneously displayed, varying from 16% to 60%.13–15 One of the biggest psychosocial challenges that families and/or health workers of children living with HIV/AIDS encounter is the disclosure of a HIV/AIDS positivity result to children.2 Making disclosure demands action to whom, when, what, and how much to disclose.16,17 Child HIV/AIDS positivity disclosure is a more important and critical task because of its benefits for the child and their family.18 Disclosure is better for ART medication adherence and helps to involve children in their healthcare decision-making.19 Some of the benefits of HIV/AIDS positivity disclosure are higher self-esteem, high coping skills, lesser feelings of depression, better adherence, and increased CD4 cells among children.20,21 Making disclosure is a challenging task to physicians and/or families because of its potential blame, stigma, and fear linked with HIV infection and its social consequence; however, disclosure is important for long-term HIV/AIDS interventions.22 Studies showed that there are delayed disclosures and/or non-disclosures for HIV-positive children, in other words how and when parents and/or physicians need to disclose to the child is not well articulated.19,23,24 Even though studies are conducted in several countries and resulted in heterogeneous results, there are limited studies on HIV/AIDS positivity disclosure among children living with HIV/AIDS in this study area. Therefore, this study was aimed to determine the prevalence of HIV/AIDS positivity disclosure and to identify factors among 6–15-year-old children currently on HAART in Dessie, Ethiopia.
Methods
Study Design and Setting
A facility based cross-sectional study design was employed in Dessie, South Wollo, from January 21 to March 12, 2020. Dessie has eight sub-cities, with a total population of 301,204. Out of these, 29,854 are children and 1346 are children living with HIV/AIDS. Dessie has 54 registered health facilities ranging from health posts to referral hospitals. There are eight health centers; two government hospitals; three private hospitals, and two specialized clinics. Out of these, thirteen health facilities (HF) were ART centers, but PMTCT services were provided in all health facilities (Dessie health bureau report, 2019).
Population of the Study
The source population for the study included all parents/caregivers of children aged six to fifteen years who were HIV-positive and were receiving follow-up treatment and started HAART at health facilities in Dessie.
Eligibility Criteria
Parents/caregivers of children living with HIV/AIDS whose age is of 6–15 years old that were on follow-up in ART departments were included, while all parents/caregivers of those children who cannot communicate or were seriously ill because of their condition during data collection were excluded from the study.
Sampling and Its Procedures
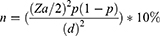
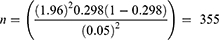
Sample size was determined by applying the formula as shown below considering the following assumptions. These are P = 29.8%,16 with 95% CI, degree of margin 5% and adding a 10% non-respondent rate.
The final sample size used for this study was 355 participants.
Four pediatric HAART and child caring health facilities were selected. As a sampling procedure, first, four cites were selected using simple random sampling technique (lottery method). Second, the sampling frame (for those HFs included) was obtained from the registration book of the respective health facilities (HFs). Third, the sample size was proportionally allocated to the four HFs (Dessie Specialized Hospital 316 (89%), Ethio-General Hospital 19 (5.2%), Bambowuha 8 (2.3%), and Dessie HC 12 (3.5%)). Eventually, during data collection systematic random sampling (at k =2) study participants were selected and accessed in each health facility after proportional allocation of samples were done.
Tools, Procedures, and Quality Control
Tools were adapted based on an earlier related literature review. Three qualified BSc nurses with experience in data gathering who work out of the research sites were recruited, along with one health office supervisor who also had data collection experience. The supervisor and data collectors each received one day training on the objectives and quality data collection techniques. Daily checks for data quality, including consistency and completeness, for early corrections were performed. Data collection was done on the date of appointment of the respondents from the HFs.
To ensure the tool was clearly articulated, study objectives and the responses of the participants were relevant and comprehensive; a pre-test for 18 (5%) respondents was done in Selam and Bati hospitals before the data collection. Visual scanning was performed to check the completeness of the questionnaires before the data entry.
Operational Definition
Disclosure: refers to when the child is aware of his/her HIV/AIDS status regardless of who disclosed the result. Child disclosure: A process whereby a child gains awareness of his/her HIV status.25
Study Variables
HIV/AIDS positivity disclosure was the outcome variable whereas; socio-demographic characteristics of the parents/caregivers; socio-cultural factors of the child; personal factors of the parent/caregiver (caregivers’ relation to the child); clinical factors of the parent/caregivers and children were considered as the predictor variables of the study.
Data Analysis
The collected data were entered into Epi info v.7.1 and exported into SPSS version 23 for further analysis. Findings like frequencies, mean (SD) were determined and presented in tables and figures. Binary analysis results with a p-value <0.25 were fitted to a multivariable logistic regression for identifying statistically significant factors at 95% CI and at a p-value <0.05.
Ethical Consideration
Ethical confirmation and clearance were gained from the Institutional Review Committee (IRC) of Wollo University, College of Medicine, and Health Sciences with a reference number CMHS 419/02/11 on 8 May 2011. Letter of offer to do the study was taken from the Amhara public health institute (Dessie Branch) after submitting the ethical clearance letter. Written informed consent was provided to parents/caregivers. Interviews were done in secured private rooms. It was a voluntary participation of participants. Withdrawing from the study was assured as a right at any time during the interview. Confidentiality and privacy were secured. All the procedures of the ethical evaluation of this study followed the Helsinki Declaration.
Results
Socio-Demographic Characteristics of Parents/Caregivers
Three hundred and forty six parents/caregivers of children living with HIV/AIDS completed the questionnaires, making a response rate of 97.5%. The mean (SD) age of parents/caregivers was 38 (±7.4) years. Two hundred forty-five (70.8%) parents/caregivers were females; more than half of the parents/caregivers were Muslim by religion 179 (51.7%); the majority of the parents/caregivers were Amhara in ethnicity 266 (76.9%). Majority of parents/caregivers can read and write 321 (92.8%). More than half of the parents/caregivers were married 238 (68.8%). Among the participants the median monthly income was 1500 Ethiopian Birr (ETB)/month (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Parents/Caregivers in Dessie, Northeast Ethiopia, 2020 (n = 346) |
Socio-Demographic Profiles of Children
The majority of children were females. Almost half of the children’s age was between 11–15 years. More than half had attended kindergarten (KG) while more than three-quarters of the children were living with biological parents (Table 2).
 |
Table 2 Socio-Demographic Characteristics of Children in Dessie, Northeast Ethiopia, 2020 (n = 346) |
Clinical Characteristics of Participants
More than three-quarters of the parents/caregivers were HIV positive and were on HAART. More than half of the children were diagnosed at the age of 6–10 years, 213 (61.6%); the mean (SD) age at diagnosis was 5.7 (±3.24) years. The mean (SD) age of children starting HAART was 6.7 (±2.4) years. Of all the children currently on HAART, only 239 (69.1%) adhered to ART drugs. Two hundred eighty-five (82.4%) were hospitalized previously. Despite all parents/caregivers and their children who were counseled for HIV/AIDS disclosure was only made for 103 (29.8%) of the children (Table 3).
 |
Table 3 Clinical Characteristics of Parents/Caregivers and Their Children in Dessie, Northeast Ethiopia, 2020 (n = 346) |
Prevalence of Children’s HIV Positivity Disclosure
Based on parents/caregivers’ responses, 101 (29.2%) of the children knew about their HIV positive diagnosis. The mean (SD) age at disclosure was 6.9 years (±2.51); more than half of the disclosures were made accidentally, 57 (56.5%). The majority of parents/caregivers did not know the right age to disclose, 197 (56.9%) (Table 4).
 |
Table 4 Information on HIV Diagnostic Disclosure Among Children Living with HIV in Dessie, Northeast Ethiopia, 2020 (n = 346) |
Out of 245 (71%) parents/caregivers, the major reported reasons for not disclosing the child’s HIV positive diagnosis were: 210 (85.7%) parents reported a lack of the required knowledge and skill; 192 (78.4%) said fear of self-discrimination; and 168 (68.6%) reported that the child is too young to disclose. About 25 (10.3%) parents/caregivers delayed disclosure because they believed s/he may feel hopelessness that was among one of the sensitive reasons.
Participant’s replied that health workers have the major responsibility to do HIV/AIDS positivity disclosure for children living with HIV/AIDS (Figure 1).
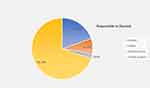 |
Figure 1 Responsible person to disclose to the child about their HIV+ diagnosis in Dessie, Northeast Ethiopia, 2020 (n = 346). |
Factors Associated with HIV+ Diagnosis Disclosure
In multivariable logistic regression, results indicated that four factors were statistically significant with HIV/AIDS positivity disclosure among children living with HIV/AIDS and on HAART. Being widowed parents/caregivers, 11–15 years age of the child, child received support from NGOs, and parents/caregivers negative for HIV/AIDS were the factors that affect HIV/AIDS positivity disclosure among children (Table 5).
 |
Table 5 A Multivariable Analysis of Factors That Affect the Disclosure of HIV Diagnosis Among Children Living with HIV in Dessie, Northeast Ethiopia, 2020 (n = 346) |
Discussion
Ethiopia has seen a dramatic decrease in the mortality and morbidity of people living with HIV/AIDS as a result of recent advances in high coverage with ART therapy.17 The prospect of children living with HIV/AIDS introduces disclosure challenges on physical and psychological health.26
According to the findings of this study, 29.2% of children on HAART had been disclosed their HIV/AIDS positive result. In comparison to studies conducted in Europe, this finding was low (75–82%).10 The possible reason is attributed to an insufficient knowledge and skill to approach their HIV-positive children, as well as fear of discrimination and stigma, by families, friends and neighbors.27 It is possible that health care providers are unsure of how to handle disclosure.
This finding was lower than a study finding conducted in East Arsi zone, Oromia region (59.9%), Dire Dawa, Eastern Ethiopia (60.6%).28,29 The possible reason might be if there is a lot of limitation of the guideline; however, it shows that there was good adherence of healthcare workers with the national guideline.
This finding was consistent with the findings of United States and Canada, where the disclosure rate was 25% to 75%,8,30 Uganda (29%),31 Addis Ababa, Ethiopia (29.8%),14 Southeast Ethiopia (28.5%),32 Debre Markos (33.3%)33 and Bahir Dar (30.1%).34
The prevalence of HIV/AIDS positivity disclosure among children was higher as compared to studies conducted in Ghana (23.3%),12 Nigeria (13.5%),24 Kenya (19%)30 and Addis Ababa, Ethiopia (17.4%).11 Differences in the period could be a factor, and over time caregivers’ awareness to disclosure benefits will be improved. Furthermore, while this study examined disclosure status in children aged 6–15; the Addis Ababa study included all pediatric age groups. The possible justification might be caregivers’ belief that their children are not mentally capable to understand the issue. In this study, a question “who should be responsible for disclosing HIV status to children” was provided to mothers and approximately 69.7% said health care providers and 19.7% said biological mother but, in practice, only 6% of the children were disclosed by health workers, and 39% by mothers, which is lower than the study results in Debre Markos, East Gojjam, and Addis Ababa, Ethiopia, where 21% and 41.4% were disclosed by health workers respectively.15,33
Widowed mothers were twice as likely as married ones to disclose HIV/AIDS positivity results. The possible reason is the mother's impending mortality. Parents disclosing the child’s HIV result was to ensure that the child would be cared for in the event of the parent’s death.19 The caregivers also revealed since children inquired about the loss of their bloodline mothers/fathers.23
Older children (11–15 years) were 2.8 times more likely to be disclosed about their HIV/AIDS positivity result than younger children (6–10 years). This finding is in line with the study findings in developing countries.12,14,16,34
HIV/AIDS negative parents/caregivers were six times more likely to disclose than HIV positive caregivers. This is because HIV/AIDS is a sensitive issue by nature and challenging to disclose as it is linked with stigma and blame, as well as the parent-child relationship issues.23,30
Children who received support from organizations (NGOs) were twice as likely to be informed of their HIV-positive diagnosis as compared to children who did not receive support. This might be because of information accessed from the supporting organizations. This finding was consistent with the findings of the South African study.23
Parents/caregivers who disclosed the HIV-positive result to their children were asked to explain the reason for disclosing, the most frequently given response was that their children were thought to be mature enough 54 (53.4%). Studies conducted in South Africa, Ghana, Kenya, and Uganda backed up this finding.18,23,30,31
Two hundred and forty five (70.8%) parents/caregivers had not informed their children on their HIV/AIDS positivity status. Most of the caregivers 210 (85.7%) responded that they had neither the knowledge and/or the skills on how to disclose, and 192 (78.4%) reported fear of self-discrimination. This result was supported by other study findings in Nigeria, Kenya, and Ethiopia.16,24,30
Limitation of the Study
Because of its cross-sectional study design, the cause effect relationship was not identified. Another limitation worth noting is the inclusion of parent/caregiver/child pairs who were engaged in their pediatric HIV/AIDS care and whose child was well enough to meet the eligibility criteria, as those less engaged in care and who may have different disclosure patterns are not represented in these results.
Conclusion and Recommendation
According to the findings of this study, the rate of HIV/AIDS positivity disclosure to children living with HIV/AIDS was lower when compared to WHO standards. Being widowed parents/caregivers, being an 11–15 year old child, receiving child support from organizations, and having HIV negative parents/caregivers were found to be statistically significant as a factor for disclosure. Managers and health workers need to focus on linking children to supporting organizations, working on parents/caregivers’ to know their HIV/AIDS status and child age specific interventions to improve disclosure practice of parents/caregivers and health workers for a better ART adherence and treatment outcome among children.
Abbreviations
AIDS, acquired immune- deficiency syndrome; ART, anti-retroviral therapy; CLHIV, children living with HIV; DHS, demographic and health survey; ETB, Ethiopian birr; HIV, human immune deficiency virus; HART, highly active antiretroviral therapy; UNAIDS, United Nations Program on HIV/AIDS; HC, health center; HCW, health care worker; HCP, health care provider; PLWA, people living with AIDS; PI, principal investigator; WHO, World Health Organization.
Data Sharing Statement
All the data supporting the findings are within the manuscript.
Acknowledgment
We would like to extend our gratitude to Wollo University for providing this research opportunity, APHI for their approval of the research process and the data collectors, HFs staff, and study participants at the various ART clinics, where the study was conducted with their cooperation in providing us the relevant information and essential resources, as well as to the employees at the district health office for their assistance and cooperation in providing the necessary background information.
Author Contributions
All authors made a significant contribution to the work reported in all areas such as the conception, study design, execution, acquisition of data, analysis and interpretation, and took part in drafting, critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Self-sponsored by the postgraduate student (the secondary author).
Disclosure
The authors have approved and declared that no competing interests exist in the publication of this paper.
References
1. Case KK, Johnson LF, Mahy M, Marsh K, Supervie V, Eaton JW. Summarizing the results and methods of the 2019 Joint United Nations Programme on HIV/AIDS HIV estimates. AIDS. 2019;33(Suppl 3):S197S201. doi:10.1097/QAD.0000000000002440
2. UNAIDS Fact Sheet. UNAIDS report on the global AIDS epidemic 2013; 2013.
3. HAPCO. HIV prevention in Ethiopia national road map; (Placeholder2); 2018. Available from: https://ethiopia.unfpa.org/en/./hiv-prevention-ethiopia-national-road-map.
4. Central Statistical Agency. Ethiopia demographic and health survey preliminary report. Addis Ababa. Ethiopia. 2013;44:125–126.
5. Survey; 2016. Available from: https://dhsprogram.com/pubs/pdf/FR255/FR255.
6. World Health Organization and UNICEF. Scale-up of HIV-related prevention, diagnosis, care, and treatment for infants and children: a Programming Framework. Geneva: World Health Organization, and UNICEF; 2018.
7. Federal HIV/AIDS Prevention and Control Office. Country progress report on HIV/AIDS response; 2012.
8. Weinberg GA. Disclosure of HIV to prenatally infected children and adolescents. HIV clinical guideline. New York; 2010: 9–11.
9. Staveteig S, Peter D, Bronesen K. Demographic patterns of HIV testing uptake in sub-Saharan Africa. Calverton, MD: ICF International; 2013. (DHS Comparative Reports No. 30).
10. Vaz LM, Maman S, Eng E, Barbarin OA, Tshikandu T, Behets F. Patterns of disclosure of HIV-status to infected children in a sub-Saharan African setting. JDBP. 2011;32(4):307. doi:10.1097/DBP.0b013e31820f7a47
11. Biadgilign S, Deribew A, Amberbir A, Escudero HR, Deribe K. Factors associated with HIV/AIDS diagnosis disclosure to HIV infected children receiving HAARA multicenter study in Addis Ababa, Ethiopia. PLoS One. 2011;6(3):17572.
12. Hayfron-Benjamin A, Obiri-Yeboah D, Ayisi-Addo S, Siakwa PM, Mupepi S. HIV diagnosis disclosure to infected children and adolescents; challenges of family caregivers in the Central Region of Ghana. BMC Pediatr. 2018;18(1):1–11. doi:10.1186/s12887-018-1330-5
13. Negese D, Addis K, Awoke A, et al. HIV-positive status disclosure and associated factors among children in North Gondar, Northwest Ethiopia. Int Scholar Res Notices. 2012;2012:54.
14. Biadgilign S, Deribew A, Amberbir A. Factors associated with HIV/AIDS diagnostic disclosure to HIV-infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia. PLoS One. 2011;6:175. doi:10.1371/journal.pone.0017572
15. Abebe Wand TS. Disclosure of diagnosis by parents and caregivers to children infected with HIV: prevalence associated factors and perceived barrier in Addis Ababa. Ethiopia. 2012;2012:1097–1102.
16. Negese D, Addis K, Awoke A, Birhanu Z, Muiuye D, Yiferu S. HIV-positive status disclosure and associated factors among children. ISRN AIDS. North Gondar, Northwest Ethiopia; 2012:1–9.
17. Jerene D, Næss A, Lindtjørn B. Antiretroviral therapy at a district hospital in Ethiopia prevents death and tuberculosis in a cohort of HIV patients. AIDS Res Ther. 2006;3(1):4. doi:10.1186/1742-6405-3-10
18. Joseph R, Cissy L, Mbasaalaki M, et al. Challenges faced by health workers in providing counseling services to HIV-positive children. J Int AIDS Soci Uganda. 2010;13(9):2–9.
19. Mahloko JM, Madiba S. Reasons for disclosure and non-disclosure. Afr J Odi Distr South Afr. 2012;4(1):1–7.
20. Nostlinger C, Jonckheer T, Debelder E. Families affected by HIV: parents’ and children’s characteristics and disclosure to the children. AIDS Care. 2008;16:641–708. doi:10.1080/09540120410001716432
21. Mellins C, Brackish E, Dolezal C. Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psychiatry. 2010;7:101–114. doi:10.1177/1359104502007001008
22. Geoffrey A, Weinberg M. Disclosure of HIV to perinatally infected children and adolescents. New York City: HIV Clinical Guidelines development of Health AIDS Institute; 2010.
23. Madiba S. Patterns of HIV diagnosis disclosure to infected children and family members: data from a pediatric antiretroviral program. Johannesburg, South Africa; 2012: 212–221.
24. Odiachi A, Abegunde D. Prevalence and predictors of pediatric disclosure among HIV-infected Nigerian children on treatment. AIDS Care. 2016;28(8):1046–1051. doi:10.1080/09540121.2016.1147018
25. Elizabeth Glaser Pediatric AIDS Foundation. Disclosure of pediatric and adolescent HIV status toolkit. Washington, DC: Elizabeth Glaser Pediatric AIDS Foundation; 2018.
26. Zhang L, Li X, Zhao J, Zhao G, Kaljee L, Stanton B. Disclosure of parental HIV infection to children and psychosocial impact on children in China: a qualitative study. Asia Pacific J Couns Psychother. 2013;4(2):163–174. doi:10.1080/21507686.2013.826261
27. Yami DB, Tuji TS, Gelete BWM, Beyene Workie K. Disclosure status of HIV-positive children and associated factors among children in public health facilities in East Arsi zone, Oromia regional state, South Eastern Ethiopia: a cross-sectional study. SAGE Open Med. 2022;10:20503121211068725. doi:10.1177/20503121211068725
28. Guta A, Areri HA, Anteab K, Abera L, Umer A. HIV-positive status disclosure and associated factors among children in public health facilities in Dire Dawa, Eastern Ethiopia: a cross-sectional study. PLoS One. 2020;15(10):e0239767. doi:10.1371/journal.pone.0239767
29. American Academy of Pediatrics. Committee on Pediatric AIDS disclosure of illness status to children and adolescents with HIV infection. Pediatrics. 2015;103:164–166.
30. Grace C, John S, Grace W, Mea K. Prevalence, Perceptions, and correlates of pediatric HIV disclosure in an HIV treatment program in Kenya. Psychol Socio-Med Aspects HIV/AIDS. 2013;25(9):1067–1076.
31. Namasopo-Oleja M S, Bagenda D, Ekirapa-Kiracho E. Factors affecting disclosure of serostatus to children attending Jinja Hospital Paediatric HIV clinic, Uganda. Afr Health Sci. 2015;15(2):344–351. doi:10.4314/ahs.v15i2.6
32. Lencha B, Ameya G, Minda Z, Lamessa F, Darega J. Human immunodeficiency virus infection disclosure status to infected school aged children and associated factors in Bale zone, Southeast Ethiopia: cross sectional study. BMC Pediatr. 2018;18(1):1–8. doi:10.1186/s12887-018-1336-z
33. Tamir Y, Aychiluhem M, Jara D. Disclosure status and associated factors among children living with HIV. Debre Markos University, Debre Markos, Ethiopia; 2014.
34. Alemu A, Berhanu B, Emishaw S. Challenges of caregivers to disclose their children’s HIV positive status receiving highly active anti-retroviral therapy at pediatric anti-retroviral therapy clinics in Bahir Dar, North West Ethiopia. J AIDS Clin Res. 2013;4:253. doi:10.4172/21556113.1000253
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.