Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Higher Neutrophil to Lymphocyte Ratio at Admission is Association with Post-PCI Depressive Symptoms in Patients with ACS
Authors Li C , Wan S, Li W, Wang Y, Li B, Chen Y, Sun P, Lyu J
Received 21 September 2022
Accepted for publication 6 December 2022
Published 22 December 2022 Volume 2022:18 Pages 2981—2990
DOI https://doi.org/10.2147/NDT.S387582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Cexing Li,1 Shaozhi Wan,1 Wenqian Li,1 Yue Wang,1 Bingqing Li,1 Yuwen Chen,1 Peiyuan Sun,1 Jianfeng Lyu2
1ChinaThree Gorges University, Yichang, People’s Republic of China; 2Affiliated Renhe Hospital of China Three Gorges University, Department of Cardiology, Yichang, People’s Republic of China
Correspondence: Jianfeng Lyu, Affiliated Renhe Hospital of China Three Gorges University, Department of Cardiology, No. 410 Yiling Avenue, Yichang, Hubei Province, People’s Republic of China, Tel +86-15671319660, Fax +86 0717-6558362, Email [email protected]
Background: Depression and elevated blood biomarkers of inflammation are common in patients with acute coronary syndrome (ACS) after percutaneous coronary intervention (PCI). Neutrophil to lymphocyte ratio (NLR) is an indicator of peripheral inflammation and has been proved to be associated with both ACS and depression.
Purpose: Our aim was to evaluate the possible association between NLR at admission and post-PCI depressive symptoms at 1 month.
Patients and Methods: A total of 224 patients with ACS who underwent PCI for the first time were recruited and completed 1-month follow-up. The 24-item Hamilton Depression Scale (HAMD-24) was used to measure depressive symptoms at 1 month after PCI. Logistic regression was used to analyze the relationship between different NLR levels and post-PCI depressive symptoms. A receiver operating characteristic (ROC) curve analysis was performed to assess the value of NLR for predicting post-PCI depressive symptoms and to determine its critical value.
Results: Of the 224 enrolled patients, 52 (23.2%) patients were diagnosed with depressive symptoms at 1 month after PCI. Patients with depressive symptoms showed significantly higher level of NLR at admission than patients without depressive symptoms (4.33 (3.26, 7.01) vs 2.57 (1.72, 3.91), P < 0.001). The proportion of depressive symptoms in post-PCI patients increases progressively along with NLR quartile. In the results of multivariate-adjusted logistic regression analysis, the odds ratio (OR) of post-PCI depressive symptoms was 12.028 (95% CI, 2.642– 54.752) for the lowest quartile of NLR compared with the highest quartile. According to the receiver operating characteristic curve (ROC), the area under the curve (AUC) for predicting post-PCI depressive symptoms was 0.716 (95% CI, 0.641– 0.791; P < 0.001), and the optimal cutoff of NLR levels was 3.235 (sensitivity: 76.9%, specificity: 66.9%).
Conclusion: Higher NLR levels at admission were associated with post-PCI depressive symptoms at 1 month, suggesting that NLR might be useful inflammatory markers to predict post-PCI depressive symptoms at 1 month.
Keywords: neutrophil to lymphocyte ratio, post-PCI depressive symptoms, acute coronary syndrome
Introduction
Depression is a common complication in patients with acute coronary syndrome (ACS) after percutaneous coronary intervention (PCI), which can occur at any time after PCI, with incidence rates ranging from 23% to 48%.1 Some studies have reported that patients with ACS have the lowest incidence of depressive symptoms 3–5 days after PCI and the highest incidence of depressive symptoms 1 month after PCI.2,3 However, compared with the higher prevalence, the clinical screening, diagnosis and treatment of post-PCI depressive symptoms are obviously insufficient. Post-PCI depressive symptoms will not only reduce the therapeutic effect and increase the difficulty of treatment, it will also seriously affect the prognosis of PCI maneuvers. Previous studies revealed that a strong association between post-PCI depressive symptoms with poor cardiovascular outcome, increased mortality and lower quality of life.4 A prospective study found that the all-cause mortality of post-PCI patients with depressive symptoms increased by 77% compared with those without depressive symptoms.5 Therefore, early diagnosis and timely treatment of post-PCI depressive symptoms are vital to reduce the incidence of major cardiovascular adverse events (MACEs) and improve the quality of life.
However, the potential pathogenesis of post-PCI depressive symptoms is still unclear. Previous studies have shown that the levels of interleukin (IL)-1β, IL-18 and IL-6 in ACS patients are significantly increased, and PCI can further induces or promotes the inflammatory response.6 In addition, we also observed that the levels of tumor necrosis factor (TNF)-α, IL-6 and IL-8 in cerebrospinal fluid of patients with depression increased significantly, and neuroinflammation was widely considered as a potential pathological mechanism of depression.7 In a word, ACS and depression are both related to inflammatory reaction. However, the above inflammatory indicators are often difficult to obtain in clinical practice. The neutrophil to lymphocyte ratio (NLR), an easily available marker of systemic inflammation, has been reported to be associated with various diseases, including cardiovascular diseases, psychiatric disorders, tumors, end-stage renal disease, peripheral artery disease, COVID-19, etc.8–15 but the detailed mechanisms have not been completely explored. Tahto et al found that NLR was significantly increased in patients with ACS, and NLR correlated significantly positive with the value of high sensitive troponin I (hs-TnI), creatine kinase MB (CK-MB) and C-reactive protein (CRP).16 Marazziti et al found that NLR levels were essentially higher in patients with major depression (MDD).17 Interestingly, We observed that the level of NLR increased significantly in both ACS and depression, and it is reported that many inflammatory markers in peripheral blood are highly correlated with inflammatory markers in cerebrospinal fluid, it is suggested that peripheral inflammatory signals may drive the inflammatory activity of central nervous system (CNS),18 it can be inferred that peripheral inflammation contributes, at least in part, to the development of post-PCI depressive symptoms. Up until now, there has been no study exploring the relationship between NLR and post-PCI depressive symptoms, so we assumed that the NLR could be used as a predictor of patients with post-PCI depressive symptoms. At present, the clinical diagnosis of post-PCI depressive symptoms mainly depends on the clinical manifestations and depression scale,19 and there is a lack of objective and accurate laboratory biochemical indicators. Therefore, the purpose of this study was to investigate the association between NLR at admission and post-PCI depressive symptoms and to further explore the predictive value of NLR in post-PCI depressive symptoms at 1 month.
Materials and Methods
Subjects
We included 224 consecutive patients who were admitted in the Department of Cardiovascular Medicine of Renhe Hospital affiliated to China Three Gorges University, diagnosed with ACS and treated with primary or elective PCI for the first time during the period from June 2020 to February 2022 into a prospective registry. ACS was diagnosed according to American College of Cardiology (ACC)/American Heart Association (AHA) guidelines.20 The patients were included in the study if they met the following criteria: (1) age of 18 years or greater; (2) the ability and eagerness to provide informed consent; (3) Patients undergoing PCI for the first time due to ACS. The exclusion criteria were as follows for the participants: (1) patients with a history of depression or other psychiatric disorders and currently taking antipsychotic drugs; (2) patients with a family history of depression or other psychiatric disorders; (3) patients with malignant tumor or immune system disorders; (4) patients with severe hepatic or renal disease; (5) patients with an active infection history 2 weeks before PCI; (6) patients with blood system diseases; (7) patients lost to follow-up, died, and clinical data are incomplete (Figure 1). This study was approved by the Ethics Committee of the Renhe Hospital Affiliated to China Three Gorges University, where all participants signed an informed consent form before participation, and complied with the Helsinki Declaration.
 |
Figure 1 Study recruitment profile. Abbreviations: ACS, acute coronary syndrome; PCI, percutaneous coronary intervention. |
Data Collection
Our researchers collected the patients’ demographics (age, sex, BMI, marital status, education level), past medical history (hypertension, diabetes), personal history (smoking and drinking) and angiographic findings of patients at admission through the hospital electronic medical record system. The body mass index (BMI) is defined as the individaul's body weight (kg) divided by the square of the height (m). The level of education is measured by the highest degree they receive and is divided into three grades, including below high school, high school and above. Marital status is divided into married or unmarried, divorced and widowed. Smoking was defined as smoking at least 1 cigarette per day for the past 6 months. Drinking was defined as having at least one alcohol intake per week for the past 6 months. Hypertension is defined as measuring SBP ≥ 140mmHg and/or DBP ≥ 90mmHg three times on different days, or any history of hypertension and currently taking antihypertensive drugs. Diabetes is defined as fasting blood glucose (FBG) ≥7.0mmol/L, glycated hemoglobin (HbA1c) ≥7.0%, or 2-h post-load glucose concentration ≥11.1 mmol/L, or any history of T2DM and currently taking hypoglycemic drugs. All patients were required to take aspirin for lifetime and a P2Y12 inhibitor for at least 1 year after PCI. Coronary angiography and PCI were performed using standard techniques. The severity of coronary artery was assessed by certified cardiologists using the Gensini scoring system through coronary angiography after admission.21 Patients were followed 1 month after PCI (See Supplementary Materials).
Blood Collection and Laboratory Test
Blood samples were collected from the patient’s elbow vein on the day of admission or next morning after fasting for at least 8 hours by trained nurses, and collected in a 3 mL EDTA-K2 tube. Which were tested in our hospital’s laboratory by the Sysmex XN-9000 (Sysmex, Kobe, Japan) Hematology Automated Analyzer, the examiner knows nothing about all clinical information. The NLR was calculated by another researcher by dividing neutrophil count by lymphocyte count.
Psychological Measurement
All psychological evaluations were conducted independently by two researchers trained by psychiatrists. At one-month follow-up, the severity of post-PCI depressive symptoms was measured by HAMD−24 through face-to-face interview or telephone interview. The Cronbach’s coefficient of Chinese version of HAMD scale is larger than 0.8, and the test-retest reliability and duplicate reliability larger than 0.7, indicating good internal consistency and stability. In addition, its content validity, criterion validity and construct validity are also acceptable.22 Patients having moderate or more depression (HAMD-24 scores >20) were diagnosed with clinically relevant post-PCI depressive symptoms. The diagnosis of post-PCI depressive symptoms was in accordance with the diagnostic criteria of depression in CCMD-3 published by the Chinese Society of psychiatry.23 The full name of CCMD-3 is China’s Classification and Diagnosis Standards of Mental Disorders 3 Edition, which is a diagnostic standard with China characteristics formulated with reference to the international diagnostic standards of mental disorders and the Diagnostic criteria for mental disorders in the United States.
Statistical Analysis
All statistical analyses were performed by SPSS22.0 statistical software (SPSS, Inc., Chicago, IL, USA). Continuous variables are presented as mean ± SD or as the median with the inter quartile range (IQR), Student’s t-test and the Mann–Whitney U-test were used to compare continuous variables. Categorical variables are presented as the relative frequency with percentage. The Chi-square test was used to compare categorical variables.
To compare characteristics by quartile of NLR levels, one-way analysis of variance (ANOVA) or the Kruskal–Wallis was used to compare continuous variables and Pearson’s Chi-square test or Fisher’s exact test was used to compare categorical variables. Multivariable regression analyses were performed using 3 different models to assess the relationship between baseline NLR and incidence of post-PCI depressive symptoms at 1 month. The models were adjusted for variables with P < 0.10 in the univariate analysis and conventional confounding factors. Furthermore, we performed tests for linear trend by entering the median value of each quartile of NLR as a continuous variable in the models. A receiver operating characteristic (ROC) curve analysis was used to identify the cutoff point of NLR levels at admission for the diagnosis of post-PCI depressive symptoms at the 1-month follow-up. In this study, statistical significance was defined as a two-tailed P < 0.05.
Results
Baseline Characteristics According to Post-PCI Depressive Symptoms
This study enrolled 272 ACS patients treated with primary or elective PCI for the first time in Renhe Hospital Affiliated to China Three Gorges University from June 2020 to February 2022. Ultimately, 224 patients were included in the final analysis, excluding 6 cases with History of depression or other psychiatric disorders, 1 case with family history of depression or other psychiatric disorders, 3 cases with malignant tumor or immune system disorders, 5 cases with severe hepatic or renal disease, 12 cases with active infection history 2 weeks before PCI, 3 cases with blood system diseases, and 18 cases with incomplete data, lost to followed-up or died. Of all patients followed up, there were 165 (73.7%) males and 59 (26.3%) females, with an average age of (62.34±10.54) years. Overall, the number of patients who were diagnosed with post-PCI depressive symptoms at the 1-month follow-up was 52 (23.2%).
The characteristics of included participants are shown in Table 1.Compared with subjects without post-PCI depressive symptoms, those with post-PCI depressive symptoms had higher proportions of female (P < 0.001), higher ages (P = 0.007), higher proportions of widowed and divorced (P = 0.002), higher proportions of hypertension history (P = 0.001), higher number of coronary lesions (P < 0.001), higher gensini score (P < 0.001), lower counts of lymphocyte (P = 0.008), higher levels of neutrophils (P = 0.006) and NLR (P < 0.001). In terms of BMI, education, history of diabetes, smoking, drinking, monocyte and platelet counts, there were no significant differences between the groups.
 |
Table 1 Patient Characteristics According to Post-PCI Depressive Symptoms |
Baseline Characteristics of the Patients According to NLR Quartile
The patients were divided into four subgroups according to the quartile of NLR at admission: Quartile 1 (n = 57): ≤1.95, Quartile 2 (n = 56): 1.96–2.84, Quartile 3 (n = 55): 2.85–4.46, Quartile 4 (n = 56): ≥4.47. As shown in Table 2, we summarized the demographic, medical history, laboratory, and coronary angiography findings of the post-PCI patients by NLR quartile. The proportions of married, HAMD score, counts of Lymphocyte and Neutrophil among the patients with different quartiles of NLR were significantly different (all P < 0.05). Other baseline characteristics have no significant difference according to the NLR quartile.
 |
Table 2 Baseline Characteristics of Post-PCI Patients in NLR Quartiles |
In addition, we compared the proportion of depressive symptoms among PCI patients stratified by NLR quartiles. The proportion of post-PCI depressive symptoms increased with ascending quartiles of NLR (P for trend <0.001). The numbers of patients with post-PCI depressive symptoms at 1 month follow-up were 4 (7.02%) in quartile 1, 8 (14.29%) in quartile 2, 18 (32.73%) in, quartile 3 and 22 (39.29%) in quartile 4 respectively (Figure 2).
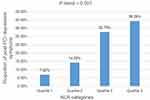 |
Figure 2 The proportion of post-PCI depressive symptoms for the quartiles of NLR at admission. Abbreviations: NLR, neutrophil to lymphocyte ratio; PCI, percutaneous coronary intervention. |
Association Between NLR Level and Depressive Symptoms After PCI
In unadjusted multivariate logistic regression analyses, the ORs for the post-PCI depressive symptoms risk of patients in quartiles 2, 3 and 4 compared with those in quartile 1 were 2.208 (0.625, 7.802), 6.446 (2.017, 20.602) and 8.574 (2.717, 27.053), respectively. After adjusting for conventional factors and significant variables in the univariate analyses, including age, sex, marital status, hypertension, Gensini score, number of lesion, diabetes and smoking, patients in the highest quartile had elevated risk of post-PCI depressive symptoms compared to patients in the lower quartile (Model 1: OR = 9.633, 95% CI 2.915–31.838, P for trend <0.001; Model 2: OR = 12.208, 95% CI 2.698–55.241, P for trend <0.001; Model 3: OR = 12.028, 95% CI 2.642–57.752, P for trend <0.001) (Table 3).
 |
Table 3 Multivariate Adjusted Odds Ratios for the Association Between NLR Levels and Post-PCI Depressive Symptoms |
ROC Curves for Predicting of Post-PCI Depressive symptoms
According to the ROC curve, the area under the curve for predicting post-PCI depressive symptoms with NLR was 0.716 (95% CI, 0.641–0.791; P < 0.001). By calculating the Jorden index, the optimal cutoff of NLR levels as an indicator for the prediction of post-PCI depressive symptoms was 3.235, with a sensitivity of 76.9% and a specificity of 66.9% (Figure 3).
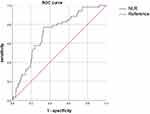 |
Figure 3 ROC curves for predicting of post-PCI depressive symptoms. Abbreviations: NLR, neutrophil to lymphocyte ratio; ROC, receiver operating characteristic. |
Discussion
As far as we know, this is the first study exploring the prospective association between NLR levels and the development of post-PCI depressive symptoms. In our study, we found that higher levels of NLR at admission were significantly related to post-PCI depressive symptoms of patients at 1 month follow-up. After adjusting for potential confounders, individuals in the highest quartile of NLR had a 12.028-fold (95% CI: 2.642–57.752) higher risk of post-PCI depressive symptoms than those with the lowest quartile of NLR. Furthermore, our findings revealed that the NLR level has a high accuracy in predicting the depressive symptoms of patients with ACS after PCI.
In addition, the incidence of post-PCI depressive symptoms at 1-month follow-up was 23.2%, which was consistent with the results of the previous studies.3 The diagnosis of post-PCI depressive symptoms is a dynamic process, with different manifestations in different time stages, and the conclusions of different studies are quite different, which may be related to the timing of post-PCI depressive symptoms determination, psychological assessment methods, and different criteria for evaluation.24 The gensini scores reflect the severity of coronary artery stenosis. Our results showed that gensini scores were risk factors for the development of post-PCI depressive symptoms, which was broadly consistent with the recent studies.25
As we all know, neuroinflammation is recognized as one of the most important pathogenesis of psychiatric or neurological disorders. Accumulating evidence shows that peripheral inflammation can induce central neuroinflammation and is closely related to the pathogenesis and progression of psychiatric or neurological disorders.26 The NLR serves as a marker of peripheral inflammation and has been proved to be related to the diagnosis and prognosis of a variety of psychiatric or neurological disorders. Chen et al found that increased NLR is associated with post-stroke depression (PSD), NLR ≥3.701 were independently associated with the development of PSD.27 Hou et al also found that elevated NLR is associated with an increased risk of mild cognitive impairment (CI) in patients with cerebral small vessel disease (CSVD).28 In addition to NLR, other peripheral inflammatory markers such as systemic immune inflammatory index (SII), platelet-lymphocyte ratio (PLR), mean platelet volume (MPV) and platelet distribution width (PDW) also have been widely studied. Oyama and Pasqui et al found that SII, PLR, MPV and PDW can predict the occurrence of postoperative delirium (POD).29,30 However, the relationship between peripheral and central neuroinflammation is not completely clear. It is reported that acute myocardial infarction induced peripheral inflammation, such as TNFα, IL-1β and IL-6, increases blood-brain barrier (BBB) permeability by affecting endothelial cells. These peripheral inflammatory cells and inflammatory cytokines may reach the CNS passing through a disrupted BBB and activate microglia, and the triggered microglia release nitric oxide (NO), prostaglandin E2 (PGE2), reactive oxygen species (ROS), and cytokines such as IL-1β, IL-6, and TNF-α, which may induce neuroinflammation to impair the function of limbic system areas and lead to depressive symptoms.31,32
Neutrophils are usually the first immune cells to be recruited to the site of inflammation. They can not only remove pathogens and debris by phagocytosis, but also release a variety of pro-inflammatory factors to activate other types of inflammatory cells. Lymphocytes also play an important role in inflammation. Sheng et al found that the neutrophil count and proportion at 24 hours after PCI in patients with ACS were significantly higher than those before PCI, while platelet and lymphocyte counts were significantly decreased.33 Additionally, a recent study also reported that the absolute counts of neutrophils, intermediate monocytes and CD4 + (helper) T cells were significantly increased in the depressed group.34 In view of that decreased lymphocyte and increased neutrophil count are both found in post-PCI patients and depression subjects, which might partly explain the increased NLR levels observed in post-PCI depression patients. Aydin et al found that patients with higher HAMD score had significantly higher NLR levels compared to patients with lower HAMD score, and NLR more than 1.57 was an independent predictor of severe or very severe depression.35 As our research shows, post-PCI patients with higher NLR values at admission were inclined to have depressive symptoms, the best cut-off value for NLR at admission was 3.235 in predicting post-PCI depressive symptoms, with sensitivity of 76.9% and specificity of 66.9%. Consequently, the NLR, which reflects the immune response and systemic inflammation based on peripheral neutrophil and lymphocyte, could be adopted as an easily available predictor for the occurrence of post-PCI depressive symptoms. In addition, Luo et al found that the normal reference interval for NLR among healthy adults is (0.88–4.0).36 In our study, the median NLR for patients with post-PCI depressive symptoms was 4.33 (3.26–7.01), which was significantly higher than that in healthy subjects.
Our study had several limitations. First, NLR levels were examined only once at admission, and we cannot assess the relationship between dynamic changes in NLR and post-PCI depressive symptoms. Second, our follow-up period of 1 month may be too short for us to explore the long-term effects of NLR on depressive symptoms after PCI. Follow-up visits were performed at 3 days, 1 month, 3 months, and 6 and 12 months after PCI is necessary. Finally, this is a single-center-based prospective study, We need to be cautious in generalizing this conclusion, larger sample size and multi-center research are needed in the future to support our findings and apply them clinically. Despite these limitations, this study will provide a scientific basis for further understanding the pathogenesis and pathological process of post-PCI depressive symptoms, and provide objective laboratory biochemical indicators for clinicians to predict the risk of post-PCI depressive symptoms.
Conclusion
Our current research shows that the higher NLR level at admission is significantly related to the development of post-PCI depressive symptoms at 1 month follow-up. The NLR measured at admission can be used as a potential diagnostic biomarker to predict post-PCI depressive symptoms.
Data Sharing Statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary Materials.
Ethics Statement
This study was approved by the Ethics Committee of the Renhe Hospital Affiliated to China Three Gorges University (2021YJ22), and complied with the Helsinki Declaration.
Acknowledgments
This study was supported by the Scientific Research Project of Hubei Provincial Health Committee (WJ2021F061).
Disclosure
The authors declare that they have no conflicts of interest in this study.
References
1. Saini RK, Chaudhury S, Singh N, et al. Depression, anxiety, and quality of life after percuataneous coronary interventions. Ind Psychiatry J. 2022;31(1):6–18. doi:10.4103/ipj.ipj_126_21
2. Kala P, Hudakova N, Jurajda M, et al. Depression and anxiety after acute myocardial infarction treated by primary PCI. PLoS One. 2016;11(4):e0152367. doi:10.1371/journal.pone.0152367
3. Gu G, Zhou Y, Zhang Y, Cui W. Increased prevalence of anxiety and depression symptoms in patients with coronary artery disease before and after percutaneous coronary intervention treatment. BMC Psychiatry. 2016;16:259. doi:10.1186/s12888-016-0972-9
4. Zhang Y, Zhai Y, Niu B, et al. Association between depression and clinical outcomes following percutaneous coronary intervention: a meta-analysis. Psychopathology. 2022;55(5):251–257. doi:10.1159/000524228
5. van Dijk MR, Utens EM, Dulfer K, et al. Depression and anxiety symptoms as predictors of mortality in PCI patients at 10 years of follow-up. Eur J Prev Cardiol. 2016;23(5):552–558. doi:10.1177/2047487315571889
6. Martínez GJ, Robertson S, Barraclough J, et al. Colchicine acutely suppresses local cardiac production of inflammatory cytokines in patients with an acute coronary syndrome. J Am Heart Assoc. 2015;4(8):e002128. doi:10.1161/JAHA.115.002128
7. Nettis MA, Pariante CM. Is there neuroinflammation in depression? Understanding the link between the brain and the peripheral immune system in depression. Int Rev Neurobiol. 2020;152:23–40. doi:10.1016/bs.irn.2019.12.004
8. Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. 2016;14(5):573–577. doi:10.1586/14779072.2016.1154788
9. Brinn A, Stone J. Neutrophil-lymphocyte ratio across psychiatric diagnoses: a cross-sectional study using electronic health records. BMJ Open. 2020;10(7):e036859. doi:10.1136/bmjopen-2020-036859
10. Cupp MA, Cariolou M, Tzoulaki I, et al. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020;18(1):360. doi:10.1186/s12916-020-01817-1
11. Pasqui E, de Donato G, Lazzeri E, et al. High neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are associated with a higher risk of hemodialysis vascular access failure. Biomedicines. 2022;10:9. doi:10.3390/biomedicines10092218
12. Delcea C, Buzea CA, Dan GA. The neutrophil to lymphocyte ratio in heart failure: a comprehensive review. Rom J Intern Med. 2019;57(4):296–314. doi:10.2478/rjim-2019-0018
13. Russu E, Mureșan AV, Arbănași EM, et al. The predictive role of NLR and PLR in outcome and patency of lower limb revascularization in patients with femoropopliteal disease. J Clin Med. 2022;11:9. doi:10.3390/jcm11092620
14. Pasqui E, de Donato G, Giannace G, et al. The relation between neutrophil/lymphocyte and platelet/lymphocyte ratios with mortality and limb amputation after acute limb ischaemia. Vascular. 2022;30(2):267–275. doi:10.1177/17085381211010012
15. Yang AP, Liu JP, Tao WQ, et al. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504. doi:10.1016/j.intimp.2020.106504
16. Tahto E, Jadric R, Pojskic L, et al. Neutrophil-to-lymphocyte ratio and its relation with markers of inflammation and myocardial necrosis in patients with acute coronary syndrome. Med Arch. 2017;71(5):312–315. doi:10.5455/medarh.2017.71.312-315
17. Marazziti D, Torrigiani S, Carbone MG, et al. Neutrophil/lymphocyte, platelet/ lymphocyte, and monocyte/lymphocyte ratios in mood disorders. Curr Med Chem. 2022;29(36):5758–5781. doi:10.2174/0929867328666210922160116
18. Felger JC, Haroon E, Patel TA, et al. What does plasma CRP tell us about peripheral and central inflammation in depression? Mol Psychiatry. 2020;25(6):1301–1311. doi:10.1038/s41380-018-0096-3
19. Jha MK, Qamar A, Vaduganathan M, et al. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(14):1827–1845. doi:10.1016/j.jacc.2019.01.041
20. Amsterdam EA, Wenger NK, Brindis RG, et al. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–e228. doi:10.1016/j.jacc.2014.09.017
21. Rampidis GP, Benetos G, Benz DC, et al. A guide for Gensini score calculation. Atherosclerosis. 2019;287:181–183. doi:10.1016/j.atherosclerosis.2019.05.012
22. Sun XY, Li YX, Yu CQ, et al. 中文版抑郁量表信效度研究的系统综述 [Reliability and validity of depression scales of Chinese version: a systematic review]. Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38(1):110–116. Chinese. doi:10.3760/cma.j.issn.0254-6450.2017.01.021
23. Chen YF. Chinese classification of mental disorders (CCMD-3): towards integration in international classification. Psychopathology. 2002;35(2–3):171–175. doi:10.1159/000065140
24. Liu X, Fowokan A, Grace SL, et al. Chinese patients’ clinical and psychosocial outcomes in the 6 months following percutaneous coronary intervention. BMC Cardiovasc Disord. 2021;21(1):148. doi:10.1186/s12872-021-01954-2
25. Wang D, Dai F, Liu W, et al. Longitudinal change and prognostic value of anxiety and depression in coronary heart disease patients. Ir J Med Sci. 2021;190(1):107–116. doi:10.1007/s11845-020-02302-7
26. Mishra A, Bandopadhyay R, Singh PK, et al. Neuroinflammation in neurological disorders: pharmacotherapeutic targets from bench to bedside. Metab Brain Dis. 2021;36(7):1591–1626. doi:10.1007/s11011-021-00806-4
27. Chen H, Luan X, Zhao K, et al. The association between neutrophil-to-lymphocyte ratio and post-stroke depression. Clin Chim Acta. 2018;486:298–302. doi:10.1016/j.cca.2018.08.026
28. Hou L, Zhang S, Qi D, et al. Correlation between neutrophil/lymphocyte ratio and cognitive impairment in cerebral small vessel disease patients: a retrospective study. Front Neurol. 2022;13:925218. doi:10.3389/fneur.2022.925218
29. Oyama T, Kinoshita H, Takekawa D, et al. Higher neutrophil-to-lymphocyte ratio, mean platelet volume, and platelet distribution width are associated with postoperative delirium in patients undergoing esophagectomy: a retrospective observational study. J Anesth. 2022;36(1):58–67. doi:10.1007/s00540-021-03007-6
30. Pasqui E, de Donato G, Brancaccio B, et al. The predictive role of inflammatory biochemical markers in post-operative delirium after vascular surgery procedures. Vasc Health Risk Manag. 2022;18:747–756. doi:10.2147/VHRM.S368194
31. Liu H, Luiten PG, Eisel UL, et al. Depression after myocardial infarction: TNF-α-induced alterations of the blood-brain barrier and its putative therapeutic implications. Neurosci Biobehav Rev. 2013;37(4):561–572. doi:10.1016/j.neubiorev.2013.02.004
32. Guo L, Zhu L. Multiple roles of peripheral immune system in modulating ischemia/hypoxia-induced neuroinflammation. Front Mol Biosci. 2021;8:752465. doi:10.3389/fmolb.2021.752465
33. Sheng J, Liu N, He F, et al. Changes in the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios before and after percutaneous coronary intervention and their impact on the prognosis of patients with acute coronary syndrome. Clinics. 2021;76:e2580. doi:10.6061/clinics/2021/e2580
34. Lynall ME, Turner L, Bhatti J, et al. Peripheral blood cell-stratified subgroups of inflamed depression. Biol Psychiatry. 2020;88(2):185–196. doi:10.1016/j.biopsych.2019.11.017
35. Aydin Sunbul E, Sunbul M, Yanartas O, et al. Increased neutrophil/lymphocyte ratio in patients with depression is correlated with the severity of depression and cardiovascular risk factors. Psychiatry Investig. 2016;13(1):121–126. doi:10.4306/pi.2016.13.1.121
36. Luo H, He L, Zhang G, et al. Normal reference intervals of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and systemic immune inflammation index in healthy adults: a large multi-center study from Western China. Clin Lab. 2019;65:3. doi:10.7754/Clin.Lab.2018.180715
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
