Back to Journals » Open Access Emergency Medicine » Volume 9
High-fidelity medical simulation training improves medical students' knowledge and confidence levels in septic shock resuscitation
Authors Vattanavanit V , Kawla-ied J, Bhurayanontachai R
Received 16 September 2016
Accepted for publication 19 November 2016
Published 22 December 2016 Volume 2017:9 Pages 1—7
DOI https://doi.org/10.2147/OAEM.S122525
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Hans-Christoph Pape
Veerapong Vattanavanit, Jarernporn Kawla-ied, Rungsun Bhurayanontachai
Division of Critical Care Medicine, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Background: Septic shock resuscitation bundles have poor compliance worldwide partly due to a lack of knowledge and clinical skills. High-fidelity simulation-based training is a new teaching technology in our faculty which may improve the performance of medical students in the resuscitation process. However, since the efficacy of this training method in our institute is limited, we organized an extra class for this evaluation.
Purpose: The aim was to evaluate the effect on medical students’ knowledge and confidence levels after the high-fidelity medical simulation training in septic shock management.
Methods: A retrospective study was performed in sixth year medical students during an internal medicine rotation between November 2015 and March 2016. The simulation class was a 2-hour session of a septic shock management scenario and post-training debriefing. Knowledge assessment was determined by a five-question pre-test and post-test examination. At the end of the class, the students completed their confidence evaluation questionnaire.
Results: Of the 79 medical students, the mean percentage score ± standard deviation (SD) of the post-test examination was statistically significantly higher than the pre-test (66.83%±19.7% vs 47.59%±19.7%, p<0.001). In addition, the student mean percentage confidence level ± SD in management of septic shock was significantly better after the simulation class (68.10%±12.2% vs 51.64%±13.1%, p<0.001). They also strongly suggested applying this simulation class to the current curriculum.
Conclusion: High-fidelity medical simulation improved the students’ knowledge and confidence in septic shock resuscitation. This simulation class should be included in the curriculum of the sixth year medical students in our institute.
Keywords: medical simulation, medical students, septic shock, resuscitation
Introduction
Septic shock is a crucial medical emergency problem around the world. There have been many attempts to improve the world-class sepsis guidelines.1,2 The latest version is the Surviving Sepsis Campaign 20123 to decrease overall mortality. However, compliance is poor, partly because of a lack of knowledge and resuscitation skills in medical personnel.4
To date, medical simulation has been popular, especially in anesthesiology, medical emergency, and critical care fields.5,6 There are many courses using simulation such as in patient safety7 and practice of skills in emergency conditions.8,9 It has many benefits for students that include meeting a real experience, no harm to patients, and it is a student-centered learning style. A study showed that a medical simulation course helps students understand better compared with a case-based discussion in the management of shock.10 Students gained more knowledge and skill in emergency situations than in problem-based learning.11 A recent randomized study suggested that high-fidelity simulation improves students’ knowledge and communication about advanced life support.12 Moreover, in septic shock resuscitation, students had better knowledge and skills in resuscitation compared with a pre-course assessment.13 The Division of Critical Care Medicine in the Faculty of Medicine at Prince of Songkla University launched a simulation course for sixth year medical students in July 2015. However, there was no study to evaluate the effectiveness of this course. The objective of this study is to compare the students’ pre- and post-course knowledge and confidence levels.
Methods
Study design
This study was a retrospective analysis, performed at a university-based medical simulation center in the Faculty of Medicine at Prince of Songkla University. This simulation center consists of several simulation labs with infant, pediatric and adult patient simulators, a skills lab, computer-based simulators, multimedia debriefing room, and high-fidelity medical mannequins. The simulation system includes simulation software programs for electrocardiography, noninvasive and invasive blood pressure monitoring, central venous pressure (CVP), oxygen saturation, and pulmonary artery pressure.
All sixth year medical students were invited to participate in the resuscitation course from November 2015 to March 2016 during rotation through internal medicine without selection. Descriptions of the study and course objectives were provided to the students. All students had 1-hour lecture on septic shock resuscitation in the fifth year of the medical curriculum and everyone passed the exam. A septic shock resuscitation handout was provided to all students. Participants were grouped in teams for the resuscitation course. A Laerdal SimMan® high-fidelity patient simulator represented a realistic septic shock patient. Computer-controlled connections with the mannequins showed the hemodynamics and respiratory parameters on a monitor. The case scenario was written by the authors. To validate the scenario, two experts received the scenario prior to the student participation. They were interviewed and their feedback was used to improve the simulation.
The septic shock scenario began with a 60-year-old male with a history of hypertension and diabetes mellitus. His chief complaint was a productive cough for 2 days associated with shortness of breath, fever, and malaise. He did not have any other symptoms. His vital signs were temperature 40°C, heart rate 112 per minute, blood pressure 85/50 mmHg, respiratory rate 22 per minute, and pulse oxygen saturation 92%. The patient was then treated by a team of four to five medical students. The team was given 15 minutes to complete the simulation. The team members played the roles of leader, nurse, and proceduralist. The course instructors assumed the roles of family member, paramedic, consultant, and lab technician, as needed. An instructor was present in the room to evaluate the team performance and another instructor was in the computer control room (Figure S1). At the end of the session, instructors gave a post-action reflection (debriefing) to evaluate much of the learning during the team-based medical simulation.
Measurements
The students completed a pre-test at the beginning of the simulation course and a post-test at the end of the course. The tests consisted of a case scenario and five multiple choice questions to test the knowledge on indications for intubation, sepsis management bundles, fluid, and vasopressor administration (Table S1). Task performance was evaluated by a simulation instructor using a 12-item checklist (Table 1). The performance scores ranged from 0 to 4, with 0 representing not done, 1 representing poor, 2 representing fair, 3 representing good, and 4 representing very good. At the end of the course, the participants were given a survey questionnaire regarding their attitude to the simulation course utilizing a Likert scale.
  | Table 1 Simulation task checklist for septic shock resuscitation Abbreviations: CVP, central venous pressure; ICU, intensive care unit; ScvO2, central venous oxygen saturation. |
Data analysis
Descriptive statistics were generated from the test scores, performance task scores, and attitude scales. Data are presented as mean ± standard deviation (SD). Proportions are presented as percentages (95% confidence interval). Comparisons between the pre-test and post-test scores and pre- and post-course confidence levels were analyzed using Student’s t-test or Wilcoxon rank sum test with significance set at a p value <0.05. We used SPSS version 16 to analyze the data.
Ethical approval
The study was approved by the Ethics Committee (EC) at the Faculty of Medicine, Prince of Songkla University (EC number 59-087-14-1). A waiver of written informed consent was granted by the Ethics Committee at the Faculty of Medicine, Prince of Songkla University because it was a retrospective study involving existing curriculum in an educational setting.
Results
Seventy-nine medical students were enrolled during rotation through internal medicine. All students participated in a high-fidelity simulation session. Knowledge of the students was represented by the pre-test and post-test scores (Table 2). The overall mean percentage score ± SD of the post-test examination was statistically significantly higher than the pre-test score (66.83%±19.7% vs 47.59%±19.7%, p<0.001). When analyzed topic by topic, the students’ knowledge improved significantly in every topic except identifying the need for intubation and selecting the choice of fluid resuscitation, but these were not statistically significant.
  | Table 2 Students’ knowledge pre- and post-test (n=79) |
Resuscitation skills were evaluated during simulation. Seventy-nine students were divided into 15 groups. The 12-task performance scores during simulation are shown in Table 3. Less than half of all groups had a score ≥3 (good) in almost all tasks except blood culture obtained prior to antibiotic and antibiotic administered. Only four groups ordered lactate measurement, identified a need for CVP/ScvO2 monitoring and fluid challenge test and only three groups had correctly ordered a dose of vasopressor (Table 3). The overall scores were fair. The maximum score was in the antibiotic administration task. The students had quite low scores in the lactate measurement request, fluid challenge test, and calculating the dose of a vasopressor.
  | Table 3 Students’ resuscitation skills (n=15 groups) Abbreviations: CVP, central venous pressure; ICU, intensive care unit; ScvO2, central venous oxygen saturation; SD, standard deviation. |
In addition, the student mean percentage confidence level ± SD in the management of septic shock was significantly better after the simulation class (68.10%±12.2% vs 51.64%±13.1%, p<0.001; Table 4).
  | Table 4 Students’ confidence levels before and after simulation course (n=79) Note: Confidence level: level 1 (not at all) to 5 (very confident). |
The majority of students strongly agreed that simulation class was useful for gaining knowledge and suggested applying this simulation class to the current curriculum. The overall experience was fun (Table 5).
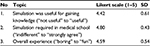  | Table 5 Students’ attitudes (n=79) Abbreviation: SD, standard deviation. |
Discussion
From our retrospective study, the simulation course was an effective learning tool to provide knowledge and increase the confidence level. As septic shock resuscitation requires a team approach, the participants could gain knowledge, skills, and experience from this method.
The overall knowledge of the students improved after the course. However, when we analyzed each item, identification for intubation and choice of fluid for resuscitation did not improve much. We found that most of the students hesitated to intubate simulated patients and initially tried the oxygen mask. Most students initially selected the right choice for fluid resuscitation (crystalloids), so the scores did not increase significantly. Our findings were similar to a study that reported that the final-year medical students had low self-competence in the intubation procedure.14 However, our scenario or mannequins did not represent real patterns of respiratory failure, so students were reluctant to intubate.
Since all students had previously had a full lecture course and reading in resuscitation skills, their skills were quite fair. This showed that septic shock resuscitation skills can be taught not only by lecture but also by simulation training. A study confirmed that a lecture before simulation training did not improve the performance skill scores.15
The participants did not do well in the fluid challenge test. They were confused whether to wait 10 minutes or continue fluid loading. Some students loaded fluid until the magic number of 20 or 30 mL/kg body weight of the simulated patient without a safety margin. This finding was similar to fluid challenge tests and optimal fluid resuscitation surveys that showed many physicians did not follow the guidelines and gave inadequate fluid resuscitation.16
The students neglected to order a lactate level. Some ordered a lactate level but did not follow the lactate clearance. They did not show a concern for microcirculation. This was compatible with a study that revealed poor compliance in lactate measurement before an education program and found that the measurement of plasma lactate was associated with lower in-hospital mortality.17 The students were also confused in ordering a dose of vasopressive agent. This result confirmed the importance of a standard intravenous drug dosing protocol to minimize dosing errors.18 We also found that the students did not request intensive care unit (ICU) care for close monitoring. A possible reason was that the students did not fully accept this course as a true situation. However, the students freely chose to assume different roles. It was probably an impact on performance skill as a whole picture. A study revealed that students who were leaders tend to understand and appreciate the process much better.19
Results from our study had an impact on teaching septic shock resuscitation to medical students and on other medical personnel. We should be much more concerned about airway management, fluid challenge techniques, the importance of lactate measurement, how to calculate and order vasopressive agents and transfer to ICU care.
Most students significantly improved their confidence levels. Simulation training improved students’ confidence levels in many studies.20–22 Our results were similar to a previous simulation course study that showed students’ confidence level improvement in the same Likert-type scales.13 This showed the value of a simulation course that simulated a true scenario for the participants. The medical mannequins could respond to their treatment and all monitoring and responses reacted immediately when they managed the patient.
The participants indicated that the course should be incorporated into the medical curriculum. Most of the students reported they had a lot of fun.
Limitations
The sample size of the students was quite small. We could not bring all sixth year medical students to take the simulation course. The multiple-choice questions in the knowledge test were not rearranged which possibly led to recall bias. The test was not done again later to test the remote memory of the students. We did not reevaluate the participants’ skills after the course. Further, we had neither a control group nor a comparison with other forms of learning patterns because of the retrospective nature of the study. Measurement of skill represents the students’ performance in these groups but was not compared to other groups of students with a different scenario or method, so the results for skill gave limited information. However, many studies showed that simulation was superior to case-based or problem-based learning.10,23 We suggest that further studies should have a control group and recommend retesting these students to judge retention of knowledge of sepsis management.
Conclusion
High-fidelity medical simulation improved the knowledge and confidence of students in septic shock resuscitation. This simulation class should be included in the curriculum of sixth year medical students in our institute.
Acknowledgments
The authors are grateful to the International Affairs Department, Faculty of Medicine, Prince of Songkla University for the language correction services.
This study was fully funded by the Faculty of Medicine, Prince of Songkla University.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Dellinger RP, Carlet JM, Masur H, et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–873. | ||
Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296–327. | ||
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. | ||
Levy MM, Rhodes A, Phillips GS, et al. Surviving sepsis campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med. 2014;40(11):1623–1633. | ||
Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment in medical education. J Gen Intern Med. 2008;23(Suppl 1):46–49. | ||
McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A c ritical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63. | ||
Nishisaki A, Keren R, Nadkarni V. Does simulation improve patient safety? Self-efficacy, competence, operational performance, and patient safety. Anesthesiol Clin. 2007;25(2):225–236. | ||
Bond WF, Lammers RL, Spillane LL, et al. The use of simulation in emergency medicine: a research agenda. Acad Emerg Med. 2007;14(4):353–363. | ||
Bond W, Kuhn G, Binstadt E, et al. The use of simulation in the development of individual cognitive expertise in emergency medicine. Acad Emerg Med. 2008;15(11):1037–1045. | ||
Littlewood KE, Shilling AM, Stemland CJ, Wright EB, Kirk MA. High-fidelity simulation is superior to case-based discussion in teaching the management of shock. Med Teach. 2013;35(3):e1003–e1010. | ||
Smithburger PL, Kane-Gill SL, Ruby CM, Seybert AL. Comparing effectiveness of 3 learning strategies: simulation-based learning, problem-based learning, and standardized patients. Simul Healthc. 2012;7(3):141–146. | ||
Cortegiani A, Russotto V, Montalto F, et al. Effect of high-fidelity simulation on medical students’ knowledge about advanced life support: a randomized study. PLoS One. 2015;10(5):e0125685. | ||
Nguyen HB, Daniel-Underwood L, Van Ginkel C, et al. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: an evaluation for medical student training. Resuscitation. 2009;80(6):674–679. | ||
Katowa-Mukwato P, Banda S. Self-perceived versus objectively measured competence in performing clinical practical procedures by final year medical students. Int J Med Educ. 2016;7:122–129. | ||
Lighthall GK, Bahmani D, Gaba D. Evaluating the impact of classroom education on the management of septic shock using human patient simulation. Simul Healthc. 2016;11(1):19–24. | ||
Courtney M, Gopinath B, Toward M, Jain R, Rao M. Are adequate fluid challenges prescribed for severe sepsis? Int J Health Care Qual Assur. 2014;27(8):719–728. | ||
Herran-Monge R, Muriel-Bombin A, Garcia-Garcia MM, et al. Mortality reduction and long-term compliance with Surviving Sepsis Campaign: a nationwide multicenter study. Shock. 2016;45(6):598–606. | ||
Jung B, Couldry R, Wilkinson S, Grauer D. Implementation of standardized dosing units for i.v. medications. Am J Health Syst Pharm. 2014;71(24):2153–2158. | ||
Baranowski M, Weir K. Power and politics in the classroom: the effect of student roles in simulations. J Politic Sci Educ. 2010;6(3):217–226. | ||
Van Dillen CM, Tice MR. Trauma simulation training increases confidence levels in prehospital personnel performing life-saving interventions in trauma patients. Emerg Med Int. 2016;2016:5437490. | ||
Hogg G, Miller D. The effects of an enhanced simulation programme on medical students’ confidence responding to clinical deterioration. BMC Med Educ. 2016;16:161. | ||
Todd JD, McCarroll CS, Nucci AM. High-fidelity patient simulation increases dietetic students’ self-efficacy prior to clinical supervised practice: a preliminary study. J Nutr Educ Behav. 2016;48(8):563–567. | ||
Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151–157. |
Supplementary materials
  | Table S1 Pre-test and post-test Abbreviations: V/S, vital signs; BT, body temperature; PR, pulse rate; RR, respiratory rate; BP, blood pressure; SpO2, pulse oxygen saturation; D/W, dextrose in water. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

