Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Herpes Zoster Ophthalmicus Clinical Presentation and Risk Factors for Lesion Recovery
Authors Xiao Z , Wu H , Chen X, Chen X, Yu R, Chen A
Received 15 October 2023
Accepted for publication 17 December 2023
Published 29 December 2023 Volume 2023:16 Pages 3767—3773
DOI https://doi.org/10.2147/CCID.S444766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jeffrey Weinberg
Zupeng Xiao, Hanyi Wu, Xin Chen, Xiaoli Chen, Rentao Yu, Aijun Chen
Department of Dermatology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China
Correspondence: Aijun Chen; Rentao Yu, Department of Dermatology, The First Affiliated Hospital of Chongqing Medical University, 1 Youyi Road, Yuzhong District, Chongqing, 400016, People’s Republic of China, Tel +86 13062377863; +86-18123303562, Email [email protected]; [email protected]
Purpose: Herpes zoster ophthalmicus (HZO) causes trouble in patients’ daily life and work. In severe cases, it may even lead to a decrease or loss of vision. To understand the demographic information and ocular symptoms of hospitalized patients with HZO, and to find potential factors related to improvement time of skin rash and duration of ocular symptoms at discharge, we design this study.
Patients and Methods: This is a retrospective study. All patients diagnosed with HZO who were hospitalized in the Department of Dermatology of a hospital in Chongqing, China from January 1, 2015 to December 30, 2021 were included in this study. A total of 189 patients were included in this study. Clinical manifestations of the disease during hospitalization, improvement time of ocular skin lesions, and whether ocular skin lesions disappeared completely at discharge were recorded.
Results: The most common ocular symptom was eyelid swelling (92.6%), followed by eye pain (48.7%). The most common ocular sign was conjunctivitis (78.3%), followed by keratitis (15.9%). There were 149 cases without residual ocular symptoms and 40 cases with residual ocular symptoms. There was no statistically significant difference in demographic characteristics between the two groups (P> 0.05). Age ≥ 70 years (B=0.381, − 0.061~0.022, P=0.005), use of glucocorticoids (B=0.260, 0.024~0.496, P=0.031), and use of topical antiviral drugs (B=0.380, 0.054~0.705, P=0.023) were factors affecting the time interval from admission to improvement of skin rash. Tearing (HR, OR=4.827, 1.956~11.909, P< 0.001) and blood urea nitrogen (OR=0.787, 0.620– 1.000, P=0.050) were factors influencing residual ocular symptoms.
Conclusion: This study could help clinicians gain a deeper understanding of the clinical manifestations and partial influencing factors of HZO patients, which may contribute to future clinical work.
Keywords: herpes zoster ophthalmicus, clinical manifestations, disease outcome, risk factors
Introduction
Herpes zoster (HZ), also known as shingles, is a contagious skin disease caused by the reactivation of the varicella-zoster virus (VZV), which lies dormant in spinal or cranial nerve ganglia after a previous infection with chickenpox.1 With the accelerated aging process and increased stress in daily work and life, as well as decreased immunity, the incidence of HZ has shown a significant upward trend in China.2 Herpes zoster ophthalmicus (HZO) is a special type of HZ, accounting for 10–20% of HZ cases, which involves the first division of the trigeminal nerve (ophthalmic division).3 It often presents as unilateral eyelid swelling, erythema and blisters along nerve roots, tearing, photophobia, and ipsilateral headache, and can involve the eye, including conjunctivitis, keratitis, scleritis, uveitis, etc.3,4 In recent decades, the incidence and related eye complications of HZO has increased according to some previous reports.5 The most common complication of HZO is postherpetic neuralgia (PHN), which had a significant impact on patients’ physical, psychological, functional and social health.6 HZO can also lead to severe complications such as depression secondary to postherpetic neuralgia, persistent pain severe vision loss and even permanent vision loss.5,6 The main risk factors include advancing age, pain in the affected skin area, rash condition and eye involvement.7 However, there are few studies on herpes zoster ophthalmicus.
This study aims to investigate the clinical manifestations and risk factors of rash recovery and eye symptoms after leaving hospital in patients with HZO.
Materials and Methods
Inclusion Criteria for Participants
This study is a retrospective study approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (ID: K2023-564). And it has the informed consent of the patient. To identify participants, this search was conducted in the discharge records of subjects reviewed at the Department of Dermatology, First Affiliated Hospital of Chongqing Medical University, between January 1, 2015, and December 31, 2021, using keywords “herpes zoster” or “herpes zoster ophthalmicus”. And they would generally be considered for discharge when the rash darkens in color, blisters dry up and form scabs without new skin lesions developing. Patients with HZO were selected according to the guideline of Werner RN if they had a typical rash of herpes zoster with primary diagnosis of HZO.8 Patients without typical skin rash or non-v1 HZ were excluded. We identified 1105 participants through the search, of which 916 were excluded as they either did not have V1 nerve involvement or did not exhibit typical skin rash. Ultimately, a total of 189 participants were included in this study.
All hospitalized patients will receive standardized, sufficient dosage and duration of antiviral treatment. The dermatologists in the inpatient department will select appropriate antiviral medications and administration methods after evaluating the condition of patients. Topical ocular medication will be administered under the guidance of ophthalmologists.
Outcome Measures
We defined the improvement of rash as the relief of eye swelling, pain, tearing, vision problems after admission. Then we recorded the time interval from admission to the improvement of rash as the primary outcome. We defined patients who still had eye symptoms at discharge, such as pain, swelling, tearing, and photophobia, as having residual eye symptoms and used it as a secondary outcome. Patients were divided into two groups based on whether they had residual eye symptoms at discharge.
Methods Used in Statistical Analysis
Demographic data, medical history, clinical presentation, ocular signs, treatment, and outcomes of enrolled patients were reviewed and analyzed. Statistical analysis was performed using IBM/SPSS software version 23. Statistical analysis included independent sample t-tests and Chi-square test to compare baseline demographics and clinical characteristics between patients with residual eye symptoms and patients without residual eye symptoms at discharge. A linear regression model was established to evaluate the risk factors of the improvement time of ocular symptoms. Binary logistic regression model was used to analyze the factors influencing the presence of residual ocular symptoms. A two-sided P value <0.05 was considered statistically significant.
Result
Demographic Characteristics and Underlying Diseases of Patients
A total of 189 patients with HZO were included in the analysis, and their demographic characteristics are shown in Table 1. The median age at presentation was 61 years (mean 59.9±14.5 years), ranging from 14 to 93 years. 85 subjects (45.0%) were over 60 years old, while 19 cases (10.1%) were under 40 years old. The male-to-female ratio was 1.59. There were 47 current smokers (24.9%), 23 former smokers (12.1%), and 119 never smokers (63.0%). Fifty-four cases (28.6%) had hypertension or coronary heart disease, 34 cases (18.0%) had diabetes, 16 cases (8.5%) had hepatitis, 11 cases (5.8%) had cancer, 11 cases (5.8%) had kidney disease, and 4 cases (2.1%) had autoimmune diseases. None of the subjects had a record of previous vaccination against herpes zoster or HIV infection.
 |
Table 1 Patient Demographics |
Ocular Signs and Symptoms of Patients
The clinical manifestations of the study population are shown in Table 2. The median time from the rash onset to ocular symptoms was 2 days (IQR 1–4 days), and the median time from rash onset to antiviral therapy was 4 days (IQR 3–6 days). The ratio of involvement between left and right sides was 1.84. All subjects presented with rashes on the head and face, with 164 cases (86.8%) having ocular symptoms, followed by 126 cases (66.7%) on the forehead, 103 cases (54.5%) on the cheeks, 82 cases (43.4%) on the scalp, and 32 cases (17.0%) at the nose and lips. Most subjects had eyelid edema (92.6%), 92 cases (48.7%) had eye pain, 35 cases (18.5%) had tearing, 25 cases (13.2%) had blurred vision, 19 cases (10.1%) had difficulty closing their eyes, 10 cases (5.3%) had photophobia, and 6 cases (3.2%) had a foreign body sensation in the eyes. The most common ocular presentation was conjunctivitis (78.3%), followed by keratitis (15.9%), scleritis (4.7%), and uveitis (1.1%). There were no cases of acute retinal necrosis or blindness among all patients.
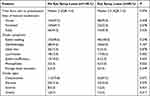 |
Table 2 Clinical Presentation of Individuals with Herpes Zoster Ophthalmicus |
Types of Antiviral Drugs
The antiviral treatment status of this study is shown in Table 3. All subjects received adequate antiviral therapy, with 109 cases receiving only oral administration, 44 cases receiving only intravenous administration, and 36 cases receiving intravenous treatment before oral administration. Among them, 148 patients used acyclovir or famciclovir, 29 cases used foscarnet sodium injection, and 12 cases used brivudine. Topical antiviral drugs were used by 161 patients. The median time from the rash onset to antiviral therapy was 4 days (IQR 3–6 days). The median duration of antiviral therapy was 7 days (IQR 5–8 days). There was no significant difference between the two groups in terms of antiviral treatment.
 |
Table 3 Treatment Profile of Patients with HZO |
Data Analysis of Outcome Measures
Table 4 and Table 5 display the influencing factors for the gap from admin to rash recover and eye symptom leave. A linear regression model was used to examine the risk of time interval from hospital admission to resolution of rash caused by HZO. In the multivariate analysis, age (β=0.381, P=0.005), glucocorticoids (β=0.260, P=0.031) and topical antiviral (β=0.380, P=0.023) were found to be significant factors affecting the time interval from admission to resolution of rash. As age increases, the use of glucocorticoids and local antiviral drugs can increase the time interval. A logistic regression model was used to identify risk factors for residual ocular symptoms in HZO patients at discharge. In multivariate analysis, tearing (OR=4.827, P<0.001) and BUN (OR=0.787, P=0.050) were identified as significant factors affecting residual ocular symptoms at discharge.
 |
Table 4 Factors Associated with the Gap from Admin to Rash Recover |
 |
Table 5 Factors Associated with Eye Symptom Leave |
Discussion
HZO is a serious condition characterized by various symptoms and complications, including postherpetic neuralgia, conjunctivitis, keratitis, uveitis, and even retinal vasculitis and necrosis.9,10 All HZO patients exhibited ocular manifestations in this study. Previous studies have reported an incidence rate of ocular symptoms in HZO patients ranging from around 50% to 80%.7,11,12 This may be attributed to the fact that hospitalized patients generally have more severe symptoms. Patients with more pronounced and severe ocular involvement are more likely to be advised for hospitalization by doctors. Hence, the incidence rate of ocular symptoms among our patients is expected to be higher. Conjunctivitis, keratitis, and uveitis have been reported as the most common ocular manifestations of HZO.4,7 In our study, conjunctivitis was the most frequent manifestation, followed by keratitis and scleritis. However, some of our patients did not undergo professional ophthalmic examinations, which may have resulted in certain ophthalmic symptoms being undetected in a timely manner.
Aging is a known risk factor for HZO.7 This study identified advanced age as an independent risk factor for delayed skin lesion recovery. Emma et al’s study13 analyzed HZO patients at the Massachusetts Eye and Ear Infirmary (MEEI), dividing the cases into two groups: 71 cases in 2007 vs 195 cases in 2013, with the average age of the latter group dropping significantly by almost six years. Carlos et al’s recent study14 also analyzed the incidence rate of HZO in Columbia and found that its proportion increases with age in a total of 100,000 residents. We speculate that herpes zoster is showing a trend of getting younger. Additionally, the older a person is, the higher the likelihood of contracting the disease. More importantly, previous studies have shown that the specific cellular-mediated immunity to VZV may decrease with age, leading to an increasing incidence and severity of HZO.15 And Anthony and Himal found that the herpes zoster vaccine can reduce the risk of developing herpes zoster and postherpetic neuralgia in individuals aged 50 and older, as well as those aged 70 and older.16,17 Therefore, we believe that older adults with normal immune function should receive vaccination against herpes zoster.
Currently, there is a debate whether corticosteroids should be used in the treatment plan for HZO. Whitley and Han18,19 analyzed 5 RCTs and conducted a Meta-analysis suggesting that early use of corticosteroids is ineffective for preventing HZO but can inhibit inflammation, alleviate acute phase pain, and accelerate skin lesion healing. Li et al’s study20 suggested that prolonged steroid use may help with eye muscle paralysis recovery. And Langston’s study21 indicated a noticeable acceleration in the recovery of rash recovery and acute pain relief for patients undergoing prednisone treatment, leading to an improvement in the quality of life. In our study, steroids were found to be meaningful in alleviating ocular skin lesions. Additionally, topical application of corticosteroid eye drops or ointments recommended by an ophthalmologist can be used.1 The specific indicators for the use of corticosteroids, the selection of specific types, and the method of use still require further research.
It has been reported that topical acyclovir cream or penciclovir cream is ineffective in the treatment of HZ.1 However, in our study, it was found that topical antiviral had a shortening effect on the improvement time of rash (P=0.005). This may be because the topical antiviral drug used in our hospital is interferon gel, which has been proved by Miyoshi et al22 in eight cancer patients that while it did not relieve pain, it reduced the time it took for herpes to disappear. However, the sample size of this study was small and no statistical analysis was conducted. And it only studied the therapeutic effects of interferon gel in HZ, not in HZO. Whether external interferon gel can be effective in the treatment of HZO needs to be further designed and analyzed.
In addition, tearing (OR=4.827, 1.956–11.909, P< 0.001) and blood urea nitrogen (OR=0.787, 0.620–1.000, P=0.050) were the remaining influencing factors of ocular symptoms in our study. However, there is no literature on the relationship between tearing and urea nitrogen and herpes zoster. We speculate that tearing may be related to the involvement of the ophthalmic branch of the trigeminal nerve, affecting the lacrimal gland. Additionally, impaired BUN may suggest that it is not only the facial nerve that is affected. We should pay more attention to patients with renal impairment who have herpes zoster ophthalmicus. We hope to further validate this in the future.
The limitations of this study are retrospective analysis bias, as it only included HZO patients admitted to a hospital in Chongqing, China with relatively limited data collection, and some HZO patients might not have had their eye symptoms fully recognized. Additionally, some patients did not undergo complete ophthalmologic examinations, lack of relevant eye data, nor were they followed up afterwards. The main advantage of this study was that all patients were examined by at least one associate chief physician and chief physician, with diagnoses accurately determined beyond doubt. Patients’ basic information, clinical symptoms and laboratory indicators were recorded in an electronic medical record system, making comprehensive data and inflammatory indicators analysis of influencing factors for HZO possible.
Conclusions
This study provides the demographics, clinical manifestations and some risk factors of HZO patients. HZO can lead to severe sequelae, most unfavorably involving the eyes, which may need more aggressive treatment for patients with severe rashes on the face. For those whose symptoms persist even after discharge, further studies and follow-up are necessary. This will help to gain a more comprehensive understanding of the long-term effects on patients with herpes zoster ophthalmicus and potential treatment options.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of the First Affiliated Hospital, Chongqing Medical University (ID: K2023-564). This article don’t involve the disclosure of patient privacy. Therefore, the ethics committee don’t require patient consent to review their medical records.
Acknowledgments
The patients in this manuscript have given written informed consent to publication of their case details. The authors would like to thank the patients who participated in this study.
Funding
This study was supported by Special Foundation for Postdoctoral Research Projects of Chongqing (2021XM3080), Natural Science Foundation General Program of Chongqing (cstc2021jcyj-msxmX0182) and Natural Science Foundation General Program of China (81874238).
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Schmader K. Herpes Zoster. Ann Intern Med. 2018;169:897. doi:10.7326/L18-0558
2. Sauerbrei A. Diagnosis, antiviral therapy, and prophylaxis of varicella-zoster virus infections. Eur J Clin Microbiol Infect Dis. 2016;35:723–734. doi:10.1007/s10096-016-2605-0
3. Ting DSJ, Ghosh N, Ghosh S. Herpes zoster ophthalmicus. BMJ. 2019;364:k5234. doi:10.1136/bmj.k5234
4. Szeto SK, Chan TC, Wong RL, Ng AL, Li EY, Jhanji V. Prevalence of ocular manifestations and visual outcomes in patients with herpes zoster ophthalmicus. Cornea. 2017;36:338–342. doi:10.1097/ICO.0000000000001046
5. Yawn BP, Wollan PC, St Sauver JL, Butterfield LC. Herpes zoster eye complications: rates and trends. Mayo Clin Proc. 2013;88:562–570. doi:10.1016/j.mayocp.2013.03.014
6. Johnson RW, Bouhassira D, Kassianos G, Leplège A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8:37. doi:10.1186/1741-7015-8-37
7. Liesegang TJ. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology. 2008;115:S3–12.
8. Werner RN, Steinhorst NI, Nast A, Pleyer U. Diagnostik und Management des Herpes zoster ophthalmicus. Ophthalmology. 2017;114:959–972. doi:10.1007/s00347-017-0562-3
9. Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82:1341–1349. doi:10.4065/82.11.1341
10. Kaufman SC. Anterior segment complications of herpes zoster ophthalmicus. Ophthalmology. 2008;115(2 Suppl):S24–32. PMID: 18243929. doi:10.1016/j.ophtha.2007.10.010
11. Borkar DS, Tham VM, Esterberg E, et al. Incidence of herpes zoster ophthalmicus: results from the pacific ocular inflammation study. Ophthalmology. 2013;120:451–456. doi:10.1016/j.ophtha.2012.09.007
12. Lam FC, Law A, Wykes W. Herpes zoster ophthalmicus. BMJ. 2009;339:b2624.
13. Davies EC, Pavan-Langston D, Chodosh J. Herpes zoster ophthalmicus: declining age at presentation. Br J Ophthalmol. 2016;100:312–314. doi:10.1136/bjophthalmol-2015-307157
14. Cifuentes-González C, Rojas-Carabali W, Fonseca-Mora MA, Mejia-Salgado G, Reyes-Guanes J, de-la-Torre A. Colombian ocular infectious epidemiology study: herpes zoster ophthalmicus prevalence and sociodemographic characterization, 2015–2019. Int J Infect Dis. 2022;116:27–33. doi:10.1016/j.ijid.2021.12.332
15. Miller AE. Selective decline in cellular immune response to varicella-zoster in the elderly. Neurology. 1980;30:582–587. doi:10.1212/WNL.30.6.582
16. Cunningham AL, Lal H, Kovac M, et al.; ZOE-70 Study Group. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 375;2016:1019–1032. doi:10.1056/NEJMoa1603800
17. Lal H, Cunningham AL, Godeaux O, et al.; ZOE-50 Study Group. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med. 372;2015:2087–2096. doi:10.1056/NEJMoa1501184
18. Whitley RJ, Cloud G, Gruber W, et al. Ganciclovir treatment of symptomatic congenital cytomegalovirus infection: results of a Phase II study. National institute of allergy and infectious diseases collaborative antiviral study group. J Infect Dis. 1997;175:1080–1086. doi:10.1086/516445
19. Han Y, Zhang J, Chen N, He L, Zhou M, Zhu C, Corticosteroids for preventing postherpetic neuralgia. Cochrane Database Syst Rev. 2013;3:CD005582. doi:10.1002/14651858.CD005582.pub4
20. Li A, Tandon A, Dinkin M, Oliveira C. The use of systemic steroids in the treatment of herpes zoster ophthalmicus-related ophthalmoplegia: case report and case meta-analysis. Am J Ophthalmol. 2021;223:241–245. doi:10.1016/j.ajo.2020.10.022
21. Pavan-Langston D. Herpes zoster antivirals and pain management. Ophthalmology. 2008;115(2 Suppl):S13–20. PMID: 18243927. doi:10.1016/j.ophtha.2007.10.012
22. Miyoshi H, Hirotsuji N, Kino T, Katsu K. Interferon alpha gel for herpes zoster. Dermatology. 1997;194:306. doi:10.1159/000246139
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
