Back to Journals » ClinicoEconomics and Outcomes Research » Volume 11
Heart failure hospitalization reduction and cost savings achieved by improved delivery of effective biventricular pacing: economic implications of the OLE study under the US setting
Authors Hernández-Madrid A, Lu X, Tsintzos SI , Fagan DH , Klepfer RN , Matía R, Chung ES
Received 15 February 2019
Accepted for publication 30 April 2019
Published 6 June 2019 Volume 2019:11 Pages 385—393
DOI https://doi.org/10.2147/CEOR.S205501
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Antonio Hernández-Madrid,1 Xiaoxiao Lu,2 Stelios I Tsintzos,3 Dedra H Fagan,2 Ruth Nicholson Klepfer,2 Roberto Matía,1 Eugene S Chung4
1Arrhythmia Unit, Cardiology Department, Ramón y Cajal Hospital, Alcalá University, Madrid, Spain; 2Medtronic, plc, Mounds View, MN, USA; 3Medtronic, Tolochenaz, Switzerland; 4The Christ Hospital Heart and Vascular Center, The Lindner Center for Research and Education, Cincinnati, OH, USA
Background: The hOLter for Efficacy analysis (OLE) study demonstrated that current device pacing diagnostics overestimate the amount of cardiac resynchronization therapy (CRT) pacing that effectively stimulates the cardiac tissue. Sub-optimal pacing increases mortality, hospitalizations, and associated health-care costs. We sought to estimate the expected number of hospital admissions due to heart failure (HF) and its respective financial impact in patients with maximized effective pacing versus conventional pacing.
Methods: A Markov model was developed to project HF hospitalizations and quantify the costs that could be avoided if pacing was maximally effective. OLE data were used to inform the prevalence of ineffective pacing among CRT patients and and average loss of pacing by causes. Adaptive CRT trial data quantified the reduction in underlying hospitalization risk by increasing effective pacing delivered. Survival was informed by a meta-analysis of 5 randomized clinical trials. Costs were analyzed from a US payer perspective.
Results: Projected average hospitalizations totaled 4.58 over a lifetime horizon for CRT patients with conventional pacing. Maximizing effective pacing delivery was projected to avoid 1.83 HF admissions/patient over the lifetime. This equates to a savings of 40% (US$22,802) compared with conventional pacing from the Medicare perspective. In a sensitivity analysis, CRT with effective pacing was projected to provide cost savings in all scenarios.
Conclusions: Maximized effective pacing leads to a lower number of HF hospitalizations, thus allowing significant cost offsets in the US setting.
Keywords: heart failure, ventricular pacing, effective pacing, hospitalization reduction, cost savings
Introduction
Heart failure (HF) is a complex disease in which the heart has an impaired ability to pump or fill with blood. Globally, an estimated 26 million people have heart failure, a number which is expected to increase with the aging population.1 In 2012, the total cost for HF in the USA was estimated to be US$30.7 billion dollars.2 The impact on the healthcare system and the patient is substantial, with approximately 1.1 million emergency department visits, 1 million hospitalizations, and 80,000 deaths due to primary HF in the USA in 2014 alone.3 Patients with HF experience significant impairment in both physical and mental aspects of quality of life along with a decline in day-to-day physical functioning.4
Cardiac resynchronization therapy (CRT) is an established treatment for patients with symptomatic HF and reduced left ventricular ejection fraction (LVEF).5–7 Randomized, controlled clinical trials have consistently demonstrated a benefit in mortality, reduction in heart failure hospitalization (HFH), and symptomatic improvement.8–10 Although CRT has proven to be beneficial, not all patients respond to CRT, with nearly one-third of patients being classified as non-responders due to failure to respond symptomatically and/or lack of ventricular reverse remodeling.11,12 Failure to respond results in progression of HF, worsening of symptoms, increased hospitalization for HF, and increased mortality.13 Reasons for suboptimal response include both patient factors, such as arrhythmia, scar burden, lead location, and QRS morphology and duration as well as device factors, such as suboptimal atrioventricular (AV) timing and <90% biventricular (BiV) pacing.14 Maintaining delivery of CRT pacing is essential to these benefits, as even <10% reductions in pacing percentage have been shown to reduce survival benefit.15–17 In addition, ventricular pacing percentage as recorded by the device may not be an accurate index of consistent capture of the myocardium, which is required for effective pacing. The hOLter for Efficacy analysis (OLE) CRT study showed that the average percent ventricular (%V) pacing as reported by the device significantly overestimated the percent effective CRT (%e-CRT) pacing that captured the myocardium (94.8% vs 87.5%, P<0.001).18 A significant minority of subjects (18%) had a discrepancy of at least 3% points between the device recorded %V pacing and the %e-CRT pacing (mean 39%±41%). When patients receive suboptimal CRT, more adverse events would be expected to increase the cost of care, primarily through increased hospitalizations. We sought to determine the impact of maximizing effective pacing delivery on HF hospitalizations and associated health-care expenditures from the US payer perspective.
Methods
Simulation model description
We used a Markov model to perform a decision analysis comparing two treatment strategies for patients with HF: CRT with conventional pacing and CRT with maximized percent effective (%Effective) pacing (hereinafter effective pacing), achieved via the EffectivCRT Diagnostic (Medtronic, Minneapolis, MN, USA) and AdaptivCRT algorithm (Medtronic), both features have previously been described in detail.19,20 The model estimated the expected number of hospital admissions due to HF, and respective financial impact in patients with effective pacing versus conventional pacing, over a lifetime (30 years) horizon. Figure 1 shows the Markov model structure that describes the health states used in the model and the possible transitions among them, with a 1-month cycle length used to evaluate lifetime costs and benefits. HF patients with CRT may or may not experience pacing disruption. The clinical reasons for a pacing disruption included: atrial fibrillation (AF), poor pacing substrate identified by observed conduction latency, variable AV nodal conduction, frequent premature ventricular contractions (PVCs), and intermittent loss of capture. Health states were defined by survival (“alive” and “dead”). Monthly, a parametric survival function was used to predict the probability of death at a given time point. Contingent on being alive, parameters were used to inform the specific probabilities of HF-related hospitalization and other pacing events in each arm. We assumed that survival rates and device-related costs were similar across the two treatments. This is a conservative approach, since a higher percentage of effective pacing would improve patients’ long-term health outcomes. The EffectivCRT and non-EffectivCRT devices are generally being paid for by the same funding code, ie, diagnosis related grouping (DRG) to the implant facility, making the payer cost for the implant equal in both compared arms. Additionally, we assumed the rate of effective pacing for the conventional pacing group to be 87.5%, which could be increased to 95% for the effective pacing group, based upon results from the OLE CRT study.18
 | Figure 1 Markov model structure. Depiction of model structure used for analysis. |
A Medicare payer perspective was adopted since a majority of CRT patients are 65 years or older. A monthly cycle length was used in the model, thus ensuring transitions can occur only once per cycle. Model development and analyses were performed with TreeAge Pro 2018 (TreeAge Software, Williamstown, MA, USA).
Study population
The model used data from the OLE CRT study, a prospective, multi-center, observational study that examined the correlation between %V pacing and %Effective pacing using a device-based algorithm.18 Patients were enrolled if they had been implanted with a Viva or Brava cardiac resynchronization therapy defibrillator (CRT-D) device (Medtronic plc) or would have one implanted within 30 days of signing the informed consent. The patient population reflected the characteristics of patients in the OLE CRT study. The patients were on average 70±9 years of age and 79% male. They had underlying heart failure with 51% ischemic heart failure, 90% New York Heart Association (NYHA) class II/III, mean LV ejection fraction of 31±6, and QRS duration of 157±26.
Model inputs
The clinical input parameters were derived from the OLE CRT study, and additional model inputs were derived from published literature (Table 1).
 | Table 1 Base case model parameters |
Clinical inputs
The key clinical data on effective pacing came from the OLE study, including parameters on probabilities of various pacing disruptions and the % effective pacing associated with each type of pacing disruption.18 The average percentage of ventricular pacing (94.8±8%) significantly overestimated the percent of effective CRT pacing (87.5±23%, P<0.001). The clinical reasons for the difference included: AF with an average % effective pacing of 69.5%; poor pacing substrate, identified by observed conduction latency with an average % effective pacing of 2.6%; variable AV nodal conduction with an average % effective pacing of 39.6%; frequent PVCs with an average % effective pacing of 71.9%; and intermittent loss of capture with an average % effective pacing of 87.1%.
Mortality
The baseline mortality risk was derived from a pooled analysis of 5 prospective trials that included NYHA Class III patients (MIRACLE, MIRACLE ICD, InSync III Marquis, PROSPECT, and Adaptive CRT).21 Extrapolated survival beyond the clinical trial was used in order to capture the long-term benefits of CRT therapy. Specifically, we assumed that patients surviving throughout the clinical trials had an expected additional lifetime that was determined by fitting a parametric survival function to the clinical trial data, accounting for age.
HF hospitalization risk
The baseline rate of HF hospitalization was 2% per month, based upon findings from Mealing et al22.
We quantified the association between percent LV (%LV) pacing delivered and HF hospitalization using data from the Adaptive CRT study.23 The Adaptive CRT trial randomized 478 subjects 2:1 to either Adaptive CRT (n=318) or echo optimization (n=160). A one-unit increase in %LV pacing was associated with a reduction of 2.3% (HR: 0.977; 95% CI: 0.965, 0.990) in the rate of HF-related hospitalization.
Cost of HF hospitalization
We examined the cost of HF hospitalization through a payer perspective. Medicare (2014–2016) data were used to establish the cost of an HF hospitalization. The estimated cost of an HF hospitalization for a CRT patient was $15,770. Device implantation costs and associated complications costs were not considered in this model. All the costs were inflation-adjusted to 2016. All cost estimates were tested in sensitivity analyses and costs were discounted at a rate of 3% per year. The discount rate was adjusted to the cycle length used.
Sensitivity analysis
Two types of sensitivity analyses were used to assess the impact of changes in the input parameters on outcomes, including one-way and probabilistic sensitivity analyses. One-way sensitivity analysis was undertaken to explore the impact of uncertainty in specific model parameters and to use data from alternative sources. Parameter estimates were varied over a plausible range according to data from prior literature, 95% CI, or by adding/deducting 25% of the deterministic values. In addition, a probabilistic sensitivity analysis was performed that incorporated uncertainty in the different parameters. Uncertainty was characterized by specifying a probability distribution for each model parameter. The probability distributions used were selected to be appropriate for the type of parameter. Monte-Carlo simulation was then used to sample a value from each parameter’s distribution and propagate the uncertainty through the model to generate a set of plausible outputs. Ten thousand simulations were undertaken to ensure that the effect of the uncertainty was fully captured.
Results
Extrapolation of clinical endpoints
The projected survival and HF hospitalization rate are reported in Table 2. The projected lifetime mean survival for all patients was 7.8 years. Poisson models were identified as the most appropriate approach to model HF hospitalizations in the patient groups since there was no overdispersion. The projected lifetime mean HF hospitalization rate in patients who had CRT with effective pacing (ie, absence of ineffective pacing) was 2.75 HF hospitalizations per patient, while the rate was 4.58 among patients with conventional pacing. This resulted in 1.83 HF hospitalizations avoided per patient over the lifetime horizon when comparing CRT with effective pacing versus conventional pacing.
 | Table 2 Clinical projections and economic results |
Economic results
Base-case analysis
The base-case results of the cost-effectiveness analysis are shown in Table 2, based on lifetime horizons with costs discounted at 3% per year. For Medicare patients, the projected lifetime cost of hospital admissions due to heart failure was 40% lower in the CRT with effective pacing group compared with the conventional pacing group ($57,233 vs $34,431). CRT with effective pacing led to a lower number of HF hospital admissions, allowing important hospital cost offsets, with savings of $22,802 per patient from a Medicare perspective.
One-way sensitivity analysis
The results of the one-way sensitivity analysis are shown in Figure 2. The x-axis represents the per-patient cost savings in the CRT with effective pacing group over a lifetime horizon. The vertical line in the center of the chart represents the deterministic cost savings for the CRT with effective pacing group ($22,802), and the bars towards the top of the chart show the parameters whose uncertainty have the most influence upon this outcome. Based on this analysis, the key parameters whose uncertainty have the most influence upon the outcome appear to be: the HR for HF hospitalization associated with each percent increase in ventricular pacing, and baseline hazard of HF hospitalization. The parameter of the HR for the risk of HF hospitalization associated with each % increase in ventricular pacing was varied based on 95% CI. If the HR was 0.965, the cost savings of CRT with effective pacing was $60,060. If the HR was as high as 0.990, the cost savings was reduced to $8,694. Varying baseline risk of HF hospitalization per month also yielded a substantial variation in the cost impact. If the risk of HF hospitalization was decreased by 25% of the base case estimate, the cost savings was reduced to $12,243. Alternatively, if the risk of HF hospitalization was raised by 25% of the base case estimate, then the cost savings increased to $42,010. CRT with effective pacing was projected to provide cost savings in all scenarios.
 | Figure 2 Tornado diagram (one-way sensitivity analysis; US$). Numbers in brackets represent the lower and upper bounds of the value used for each parameter. |
Probabilistic sensitivity analysis
Based on the set of 10,000 sampled input parameter values, the mean lifetime savings for CRT with effective pacing compared with conventional CRT were $30,163 per patient. Figure 3 shows a histogram of the cost impact (effective pacing vs conventional pacing) for the 10,000 probabilistic simulations – it can be observed that the significant majority (90.2%) of these resulted in cost savings in the effective pacing group.
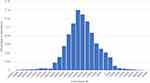 | Figure 3 Probabilistic analysis results (US$). |
Discussion
Using a Markov model, we quantified the incremental benefit of CRT with effective pacing and found 1.83 HF hospitalizations avoided over the projected survival time of 7.8 years. The reduction in HF hospital admissions allows for important hospital cost offsets from a Medicare perspective, which was 40% lower than the costs associated with conventional pacing. Furthermore, one-way sensitivity analyses also projected cost savings in the CRT with effective pacing group across all scenarios analyzed. While prior reports have addressed the cost-effectiveness of CRT, to our knowledge, this is the first report to quantify the incremental benefit associated with maximizing the %Effective pacing.
The cost-effectiveness of CRT using a within-trial analysis from a prospective, randomized, controlled trial was first demonstrated in NYHA III/IV patients from the CARE-HF trial. Clinical results from the trial demonstrated a benefit in mortality, quality of life, symptoms, and echo parameters compared with optimal medical therapy.24 In a follow-up report, the incremental cost-effectiveness of CRT therapy was found to be €19,319 per quality-adjusted life year (QALY).25 Shortly thereafter, an analysis from the COMPANION trial evaluated the cost-effectiveness of CRT-P and CRT-D for patients living with NYHA III/IV heart failure.26 Over a two-year follow-up duration, all-cause hospitalizations were reduced by 29% for CRT-D and 37% for CRT-P compared with optimal medical therapy. In addition, the incremental cost-effectiveness ratio (ICER) was $19,600 per QALY for CRT-P and $43,000 per QALY for CRT-D, both relative to optimal pharmacological therapy using a seven-year base-case time period. Cost-effectiveness findings were later extended to the mildly symptomatic (NYHA I/II) HF population with an analysis of the REVERSE trial.27 The CRT ON group gained 0.80 QALYs compared with CRT OFF, resulting in an ICER of €12,278 per QALY gained, suggesting that patients with mildly symptomatic HF experience a similar cost-effectiveness benefit as those with more severe HF symptoms. More recently, the cost-effectiveness of CRT was demonstrated across a pool of 12,638 patients from 13 randomized trials, encompassing devices across manufacturers.22 Specifically, CRT-D was cost-effective for all left bundle-branch block morphology patients with NYHA I-III.
The above-referenced studies analyzed outcomes and cost–benefit for the trial population as a whole. It is important to highlight that differences in pacing delivery may impact patient outcomes. For example, analyses have also shown that reductions in percentage of pacing can impact outcomes, including heart failure hospitalizations and mortality.15,28 More detailed results from the Adaptive CRT trial specifically quantified the incremental benefit for each percentage point increase in %LV pacing.23 For each unit increase in the overall %LV pacing, the risk for time to HF-related hospitalization decreased by 2.3%. As the use of the Adaptive CRT algorithm has been correlated with increased %Effective pacing delivery, compared with echo-optimized CRT,29 this was incorporated into our resource use inputs in order to quantify the incremental benefit of maximizing LV pacing. In addition, the trials estimating cost-effectiveness likely included a mix of patients that had both ineffective and effective pacing. The OLE trial showed that 18% of subjects had a discrepancy of ≥3% between %V pacing reported by the device and %Effective CRT pacing (mean 39±41%).18 Reasons for ineffective pacing include atrial fibrillation, poor pacing substrate, viable AV nodal conduction, frequent premature ventricular complexes, and intermittent loss of capture. Each of these factors was input into our model to calculate the cost savings achievable with maximum effective pacing delivery. Using this, we found an average cost savings of $22,802 per patient from a Medicare perspective.
Effective CRT thus serves as a tool for identifying patients with suboptimal response to CRT. By determining the mechanism of ineffective pacing, the physician may be able to take actions to potentially increase the %Effective pacing. For example, LV conduction latency may be resolved via reprogramming to an alternate pacing vector or changing pacing output at very little cost. Additionally, in feature-equipped devices, programming on algorithms, such as AdaptivCRT, could also be performed with little cost.30 This algorithm provides dynamic adjustment of the AV interval and potentially corrects inappropriately sensed and paced AV intervals; thus it is correlated with increased %Effective CRT pacing delivery.29 These relatively low-cost adjustments are in contrast to other less cost-effective interventions. For example, if a patient has a 1% gap in effective pacing due to lead placement, it would not likely be beneficial from a cost or benefit perspective to perform a lead revision; however, if the gap was 90%, this cost–benefit ratio would likely be met.
Limitations
Our analysis has several important limitations to consider when interpreting the data presented. First, the model calculates the incremental benefit of increasing %Ventricular pacing based upon a study that included both effective and ineffective pacing, that is, not all data used for calculations were from patients with 100% effective pacing. However, data used were from the Adaptive CRT trial, and as mentioned above, the use of this algorithm has been shown to be correlated with a higher percentage of effective pacing compared with standard CRT. Additionally, our model is based upon the assumption that every percentage point of increase in pacing is equally valuable (a linear relationship). Likely, there is both an upper threshold and a lower threshold where there are benefit and loss of benefit. Importantly, both of these limitations actually underestimate the actual benefit in the reduction of HF hospitalizations with maximizing %Effective pacing. Lastly, our analytic approach was based on trial-collected data that were used to generate risk equations informing long-term predictions, and external data were limited to the costs. While this approach maximized the internal validity of the analyses, it potentially limits the generalizability of our study findings.
Conclusion
Maximizing effective pacing results in a substantial decrease in healthcare costs by reducing avoidable hospitalizations. Although CRT has already proven to be cost-effective, there is a sizeable opportunity to further improve upon this as evidenced by the number of avoidable hospitalizations, especially in light of the ability to correct ineffective pacing with simple device reprogramming. Use of a diagnostic algorithm to identify ineffective CRT can result in early identification and intervention, and lead to improved outcomes and cost-effectiveness.
Disclosure
AHM received consulting fees/honoraria from Medtronic; XL is an employee/shareholder of Medtronic. SIT is an employee/shareholder of Medtronic. DHF is an employee/shareholder of Medtronic. RNK is an employee/shareholder of Medtronic; she also has a patent 86613848 pending. ESC received consulting fees/honoraria from Medtronic. He also received personal fees from Abbott and Boston Scientific, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3:7–11. doi:10.15420/cfr.2016:25:2
2. Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi:10.1161/HHF.0b013e318291329a
3. Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11:e004873. doi:10.1161/CIRCHEARTFAILURE.117.004873
4. Hobbs FD, Kenkre JE, Roalfe AK, Davis RC, Hare R, Davies MK. Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002;23:1867–1876.
5. Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34:2281–2329. doi:10.1093/eurheartj/eht150
6. Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51:e1–e62. doi:10.1016/j.jacc.2008.02.032
7. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e385–e484. doi:10.1161/CIRCULATIONAHA.106.178233
8. Cleland JG, Abraham WT, Linde C, et al. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J. 2013;34:3547–3556. doi:10.1093/eurheartj/eht290
9. Freemantle N, Tharmanathan P, Calvert MJ, Abraham WT, Ghosh J, Cleland JG. Cardiac resynchronisation for patients with heart failure due to left ventricular systolic dysfunction – a systematic review and meta-analysis. Eur J Heart Fail. 2006;8:433–440. doi:10.1016/j.ejheart.2005.11.014
10. Linde C, Abraham WT, Gold MR, et al. Predictors of short-term clinical response to cardiac resynchronization therapy. Eur J Heart Fail. 2017;19:1056–1063. doi:10.1002/ejhf.795
11. Pitzalis MV, Iacoviello M, Romito R, et al. Cardiac resynchronization therapy tailored by echocardiographic evaluation of ventricular asynchrony. J Am Coll Cardiol. 2002;40:1615–1622.
12. Yu CM, Fung WH, Lin H, Zhang Q, Sanderson JE, Lau CP. Predictors of left ventricular reverse remodeling after cardiac resynchronization therapy for heart failure secondary to idiopathic dilated or ischemic cardiomyopathy. Am J Cardiol. 2003;91:684–688.
13. Daubert C, Behar N, Martins RP, Mabo P, Leclercq C. Avoiding non-responders to cardiac resynchronization therapy: a practical guide. Eur Heart J. 2017;38:1463–1472. doi:10.1093/eurheartj/ehw270
14. Mullens W, Grimm RA, Verga T, et al. Insights from a cardiac resynchronization optimization clinic as part of a heart failure disease management program. J Am Coll Cardiol. 2009;53:765–773. doi:10.1016/j.jacc.2008.11.024
15. Hayes DL, Boehmer JP, Day JD, et al. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm. 2011;8:1469–1475. doi:10.1016/j.hrthm.2011.04.015
16. Koplan BA, Kaplan AJ, Weiner S, Jones PW, Seth M, Christman SA. Heart failure decompensation and all-cause mortality in relation to percent biventricular pacing in patients with heart failure: is a goal of 100% biventricular pacing necessary? J Am Coll Cardiol. 2009;53:355–360. doi:10.1016/j.jacc.2008.09.043
17. Ruwald AC, Kutyifa V, Ruwald MH, et al. The association between biventricular pacing and cardiac resynchronization therapy-defibrillator efficacy when compared with implantable cardioverter defibrillator on outcomes and reverse remodelling. Eur Heart J. 2015;36:440–448. doi:10.1093/eurheartj/ehu294
18. Hernandez-Madrid A, Facchin D, Klepfer RN, et al. Device pacing diagnostics overestimate effective cardiac resynchronization therapy pacing results of the hOLter for Efficacy analysis of CRT (OLE CRT) study. Heart Rhythm. 2017;14:541–547. doi:10.1016/j.hrthm.2017.01.022
19. Ghosh S, Stadler RW, Mittal S. Automated detection of effective left-ventricular pacing: going beyond percentage pacing counters. Europace. 2015;17:1555–1562. doi:10.1093/europace/euv062
20. Krum H, Lemke B, Birnie D, et al. A novel algorithm for individualized cardiac resynchronization therapy: rationale and design of the adaptive cardiac resynchronization therapy trial. Am Heart J. 2012;163:747–752 e741. doi:10.1016/j.ahj.2012.02.007
21. Chung ES, Singh JP, Martin DO, et al. Clinical and economic value of maximizing response to cardiac resynchronization therapy (CRT): evidence from five randomized controlled trials. Circulation. 2014;130:A16318. Abstract.
22. Mealing S, Woods B, Hawkins N, et al. Cost-effectiveness of implantable cardiac devices in patients with systolic heart failure. Heart. 2016;102:1742–1749. doi:10.1136/heartjnl-2015-308883
23. Hayes DL, Monteiro JV, Tsintzos SI, Eggington S, Mittal S. Abstract The relationship between percentage left ventricular (LV) pacing and cardiac resynchronization therapy (CRT) outcomes: each percentage matters. Heart Rhythm. 2016;13:S427–S514.
24. Cleland JG, Daubert JC, Erdmann E, et al. Cardiac resynchronization-heart failure study I. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–1549. doi:10.1056/NEJMoa050496
25. Calvert MJ, Freemantle N, Yao G, et al. Cost-effectiveness of cardiac resynchronization therapy: results from the CARE-HF trial. Eur Heart J. 2005;26:2681–2688. doi:10.1093/eurheartj/ehi662
26. Feldman AM, de Lissovoy G, Bristow MR, et al. Cost effectiveness of cardiac resynchronization therapy in the comparison of medical therapy, pacing, and defibrillation in heart failure (COMPANION) trial. J Am Coll Cardiol. 2005;46:2311–2321. doi:10.1016/j.jacc.2005.08.033
27. Linde C, Mealing S, Hawkins N, Eaton J, Brown B, Daubert JC. Cost-effectiveness of cardiac resynchronization therapy in patients with asymptomatic to mild heart failure: insights from the European cohort of the REVERSE (Resynchronization reverses remodeling in systolic left ventricular dysfunction). Eur Heart J. 2011;32:1631–1639. doi:10.1093/eurheartj/ehq408
28. Gasparini M, Galimberti P, Ceriotti C. The importance of increased percentage of biventricular pacing to improve clinical outcomes in patients receiving cardiac resynchronization therapy. Curr Opin Cardiol. 2013;28:50–54. doi:10.1097/HCO.0b013e32835b0b17
29. Varma N, Stadler RW, Ghosh S, Kloppe A. Influence of automatic frequent pace-timing adjustments on effective left ventricular pacing during cardiac resynchronization therapy. Europace. 2017;19:831–837. doi:10.1093/europace/euw108
30. Martin DO, Lemke B, Birnie D, et al. Investigation of a novel algorithm for synchronized left-ventricular pacing and ambulatory optimization of cardiac resynchronization therapy: results of the adaptive CRT trial. Heart Rhythm. 2012;9:1807–1814. doi:10.1016/j.hrthm.2012.07.009
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
