Back to Journals » Open Access Emergency Medicine » Volume 15
HEAR SCORE: A Proposal to Use Only Anamnestic and EKG Data to Evaluate Patients with Very Low Risk Chest Pain
Authors Mosso ML, Montemerani S
Received 3 October 2022
Accepted for publication 7 January 2023
Published 19 January 2023 Volume 2023:15 Pages 29—36
DOI https://doi.org/10.2147/OAEM.S391929
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Maria Lucia Mosso,1 Sara Montemerani2
1S.C. Medicina e Chirurgia d’Accettazione ed Urgenza (MeCAU) – Pronto Soccorso, Dipartimento Emergenza Urgenza. Ospedale S. Andrea, Vercelli, Italia; 2UOC Medicina d’Urgenza e Pronto Soccorso, Dipartimento Emergenza Urgenza. Ospedale San Donato, Arezzo, Italia
Correspondence: Sara Montemerani, UOC Medicina d’Urgenza e Pronto Soccorso, Dipartimento Emergenza Urgenza. Ospedale San Donato, Arezzo, Italia, Tel +39 0575-255002, Email [email protected]
Purpose: Chest pain in a common symptom in patients attending Emergency Department worldwide and can be related to an extensive variety of disorders, so it represents a diagnostic and logistic challenge for Emergency physicians. The aim of this study is to identify a subgroup of patients with a low pre-test probability of major adverse cardiac events, for which there is no need of troponin testing, to avoid potential harm from false-positive testing and long length stay in ED.
Patients and Methods: We retrospectively analyzed data of patients that attended ED of Siena complaining chest pain from January 2019 to August 2021. We used a modified HEART score, only evaluating history, EKG, age and risk factors. A 0– 1 HEAR score was considered at very low risk for adverse cardiac events. Sensitivity, specificity, PPV, NPV and incidence of adverse cardiac events were calculated. The accuracy of HEAR score was evaluated with ROC curve. The correlation of adverse cardiac events with HEAR score 0– 1 was evaluated with Fisher test.
Results: In this study, we included 2046 patients, of which 279 were classified at very low risk. The incidence of adverse cardiac events in this population was 0.36%. Sensibility was 97.5%, sensitivity 61%, PPV 36.8%, NPV 99.1%. The AUC for global accuracy of HEAR score was 0.945. Chi-square’s P value for the association between adverse cardiac events and HEAR score 0– 1 was < 0.001.
Conclusion: The draft presented in this study answers to the necessity to make a personalized path for patients attending ED with chest pain. The choice to avoid troponin testing may appear risky, but data from this study and from other similar show that a careful evaluation of clinical data and EKG allows to correctly discriminate which patients will not have adverse cardiac events, reducing the length of stay in ED.
Keywords: chest pain, HEAR score, emergency medicine, troponin, electrocardiogram
Introduction
Chest pain in a common symptom in patients attending Emergency Department (ED) worldwide.1,2 An extensive variety of disorders can be related, ranging from life-threatening syndromes such as acute coronary syndromes (ACS), acute aortic diseases and PE, to conditions that are relatively harmless. According to a recent European Society of Cardiology review,1 half of patients presenting with acute chest pain was discharged with a diagnosis of non-cardiac related chest pain; while on average only 25% of patients who are admitted to hospital have a final diagnosis of acute coronary syndrome. Moreover, 2% of chest pain patients with ACS are erroneously discharged from the ED, with a twofold increase in 30-days morbidity and mortality.2 Therefore, chest pain represents a diagnostic and logistic challenge for Emergency Doctors. To help clinicians with the evaluation of this heterogeneous population, a lot of risk stratification tools have been proposed and the more relevant are GRACE score, TIMI score, HEART score, ADAPT and EDACS. HEART score was specifically developed for unselected patients with chest pain presenting at the ED and is considered the best to use in this setting.3
As in the work of Smith et al,4 the aim of this study is to identify a subgroup of patients complaining chest pain with a low pre-test probability of major adverse cardiac events (MACE), for which there is no need of troponin testing, to avoid potential harm from false-positive testing and long length stay in ED. We decided to use a modified HEART score,5 only evaluating history, EKG, age and risk factors. This represents a comprised version of HEART score that allow to immediately evaluate patients with very low-risk chest pain, only using anamnestic and EKG data. A HEAR score of 0–1 was considered at very low risk for adverse cardiac events. We chose the threshold for missed MACE <1%.
Materials and Methods
Study Design
This is an observational study in which we retrospectively analyzed data extracted from medical records of patients who attended Emergency Department of Azienda Ospedaliera Universitaria Senese (AOUS) complaining chest pain, from January 2019 to August 2021. The AOUS is a reference point (2nd level Emergency Department) for the entire South-East Area of Tuscany for patients with high complexity or with time-dependent pathologies such as stroke, myocardial infarction, major trauma, sepsis. Patients with acute chest pain represent the 8% of the Emergency Room accesses. These patients are evaluated through a validated pathway of acute chest pain that added to the standard clinical evaluation the blood analysis of high sensitivity troponins.
Selection of Population
We extracted from ED software all medical records of patients complaining chest pain, from January 2019 to August 2021. We included all patients that have been classified by triage with “chest pain” as the main reason to come to ED. Subsequently, the following exclusion criteria were applied: age <18, pregnancy, SARS-CoV-2 positivity, post traumatic chest pain, no troponin testing, patients transferred from other hospitals for cardiological evaluation.
Data Collection
By consulting electronic medical records, we collected for each patient data regarding chest pain characteristic (typical vs atypical), EKG, age and cardiovascular risk factors. With these data, we calculated the HEAR score and we divided the population in two groups: very low cardiovascular risk (HEAR score 0–1) and at major cardiovascular risk (HEAR score >1). Regarding to history, we used the Chest pain score to attribute the score and this assessment was blinded from the outcome and troponin level. Regarding cardiovascular risk factors, their absence in medical records was counted as not being present.
A subgroup of patient was excluded because medical records were incomplete (mainly, there were not enough data to score history and/or there were not EKG referrals).
Measures and Statistical Analysis
The definition of myocardial infarction used in this study is the fourth universal definition by ESC 2018. Troponin assay was a high-sensitivity test.
We calculated the incidence of adverse cardiac events in the HEAR 0–1 group. We considered “adverse cardiac events” both MACE (a composite endpoint of death for any reason, myocardial infarction and revascularization) and unstable angina. The follow-up period was 6 weeks after discharge and has been done evaluating the patients that re-attended ED of AOU Siena and/or patients that were evaluated in Cardiological Office of AOU Siena.
For statistical testing, we randomly selected 106 patients in each group. Statistical analyses were performed using SPSS Statistics© software, version 28 (IBM©). Continuous variables were expressed as average values and standard deviations. Qualitative variables were expressed as absolute values and percentages. Sensitivity, specificity, PPV, NPV for adverse cardiac events were calculate for 0–1 HEAR score. The accuracy of HEAR score has been evaluated with ROC curve. The correlation of adverse cardiac events with HEAR score 0–1 has been evaluated with Fisher’s exact test, with a statistical significance threshold of p <0.05.
Results
From January 2019 to August 2021, 4915 patients attended ED AOU Siena complaining chest pain. After the application of exclusion criteria, we included in the study 2608 patients. Of them, 562 patients were also excluded because data reported in medical records were not exhaustive to calculate HEAR score. So, in the end, 2046 patients were included and were divided in two groups based on HEAR score (Figure 1).
 |
Figure 1 Population selection and division based on risk stratification. |
Very low-risk HEAR score (0–1) was attributed to 279 patients (13.6%), while HEAR >1 to 1767 patients. The average length of stay in ED was 275 ± 144 minutes for HEAR 0–1 group (minimum 69 minutes - maximum 1286 minutes), while in HEAR >1 group was 470 ± 340 minutes (minimum 5 minutes - maximum 2577 minutes). Clinical characteristics of the study population are summarized in Figure 2. Patients in HEAR >1 group are older and have more comorbidities, these factors are all related with the clinical outcome.
 |
Figure 2 Clinical characteristics of the study population. |
Patient’s Characteristics in Very Low Risk Group
The HEAR 0–1 group counted 279 patients, of which male were 160 (57%), the average age was 38 ± 10 years. Particularly, 104 patients (37.3%) got an HEAR score 0, while the others 175 patients (62.7%) got HEAR score 1. The history was evaluated not suspicious in 92.1% of patients and EKG was normal in 93.5%. 211 (75.6%) patients had no risk factors, while 61 (21.9%) had one risk factor and 7 (2.5%) had two risk factors. Regarding risk factors, smoking was the prevalent factor (42 patients), followed by hypertension (11 patients) and family history of CAD (10 patients). In this population, dyslipidemia, diabetes and obesity affected only few patients. Figure 3 summarizes HEAR characteristics in this group.
 |
Figure 3 HEAR score characteristics in patients with very low risk. |
Troponin testing in HEAR 0–1 group was normal in 271 patients (97.1%). Three of eight patients with abnormal troponin values were discharged, two of them had negative follow-up, while one had ventricular hypertrophy in an echocardiographic evaluation. Four patients with abnormal troponin values were admitted in Cardiology Department or in Intensive Short Observation with a diagnosis of myocarditis or pericarditis; all of them had associated symptoms like fever and/or dyspnea that could suggest these diseases. Finally, only one patient with abnormal troponin testing was admitted to Cardiology Unit with a diagnosis of unstable angina. So, the incidence of adverse cardiac events in the population at very low risk was 0.36%, below the threshold value <1%.
Diagnostic Characteristics of HEAR 0–1
For statistical testing, due to the great diversity of the sample size in the two groups, we randomly selected 106 patients in each group. Sensitivity of HEAR 0–1 score for adverse cardiac events was 97.5% (95% CI 86.84% to 99.94%) and sensitivity 61% (95% CI 53.33% to 68.38%). Positive predictive value was 36.8% (95% CI 32.42% to 41.4%), while negative predictive value was 99.1% (95% CI 93.97% to 99.86%).
The accuracy of HEAR score was evaluated with ROC curve (Figure 4). The AUC was 0.945 (95% C.I. 0.906–0.984), so it is a very accurate test. The association of adverse cardiac events and HEAR score 0–1 was evaluated with Fisher’s exact test. P value was <0.00001.
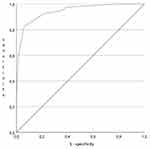 |
Figure 4 ROC curve for HEAR score. |
Discussion
The aim of this study was the identification of a subgroup of patients in which the pre-test probability of acute coronary syndrome was low enough to justify no troponin testing. In analogy with a previous study,4 we use a modification of HEART score, only evaluating anamnestic and EKG data. The HEAR score 0–1 was selected to identify patients at very low risk. In this subgroup of patients, the incidence of adverse cardiac events was 0.36%, far below the threshold value <1%.
Statistical testing showed very good sensitivity (97,5%) and very good negative predictive value (99.1%), so HEAR score 0–1 is really related to absence of adverse cardiac events.
A posteriorly revaluation of the clinical history of the only one patient that had the event in the very low-risk group, lead to a reclassification. The patient was 39 years old and attended ED complaining moderately suspicious chest pain, no known risk factors were notified in medical record. So, the HEAR score was 1. Troponin testing was abnormal and the Cardiologist performed an echocardiographic evaluation reporting an uncertain hypokinesia of interventricular septum and suggested admission in hospital. The patient refused and was voluntary discharged. After 5 days, he returned to ED complaining the same symptom, the troponin testing was again abnormal, so he was admitted to Cardiology Unit. Here, a more comprehensive medical history was performed: 3 risk factors (obesity, smoke and family history of CAD) were reported and furthermore he was diagnosticated with hypertension and mild dyslipidemia. With these data, the HEAR score was 3. The patient was tested with pharmacologic stress echocardiography, that resulted negative. In the end, this was a patient that could not be classified at very low risk, but stress echocardiography led to exclude coronary artery disease.
After the reclassification of this case, we can assert that no events were recorded in HEAR 0–1 group.
Troponin testing in HEAR 0–1 group was normal in 97.1%. Abnormal values were recorded in all patients diagnosticated with myocarditis or pericarditis; all of them had also associated symptoms like dyspnea and fever that suggest performing blood test. So, we can assert that, in this group of patients, troponin testing is more useful when a non-coronary disease is suspected.
The average length of stay in ED for patients with very low risk was 4 hours and 35 minutes. All of them were tested with a first troponin test, but most of them were also tested with 3 hours later troponin test, even if the first was normal. So, we can assert that routine troponin testing lead to a long stay in ED, without a better clinical outcome.
The results of this study are comparable to those of other studies on this topic. Smith et al,4 in their study with 3809 patients of which 447 classifieds at very low risk, got a sensitivity of 97.8% and VPN of 99.1%. The incidence of MACE was a little higher, 0.9%. O’Rielly et al6 classified 202 patients of 1150 at very low risk, only one patient had a MACE, so the incidence was 0.49% and sensitivity 99.2%. In another bigger study7 with 22,109 patients, the incidence rate for MACE was 0.1%. In all this studies, patients at very low risk were classified with HEAR score of 0–1. Tscherny et al8 tried to answer to the same question of this study with a modified Grace score: using only Killip classification, systolic blood pressure, heart rate, age, presentation with cardiac arrest and ST deviation, they considered at very low-risk patients with modified Grace score <108 without ST deviation. They included in the study 2755 patients and 2562 were classified at very low risk. The incidence rate of MACE was 0.2%, sensitivity 96.1% and VPN 99.8%. In Figure 5 are compared and summarized the results of these studies.
 |
Figure 5 Comparison of results of studies on patients complaining chest pain at a very low risk of adverse cardiac events. |
Limitation
This study has some limitations. Data have been analyzed retrospectively and HEAR score has been calculated posteriorly from data in medical records, so this could have led to underestimation of score. Follow-up has been done evaluating the patients that re-attended ED of AOU Siena and/or patients that were evaluated in Cardiological Office of AOU Siena; this could have led to potentially lose data of patients that had the follow-up evaluation elsewhere.
Conclusion
The draft presented in this study answers to the necessity to make a personalized path based on characteristics of patients that come to ED complaining chest pain, to avoid excessive tests that are expensive and subjects low-risk patients to potential harm from false-positive testing, without clinical improvement.
The choice to avoid troponin testing may appear risky, but data from this study and from other similar show that a careful evaluation of clinical data and EKG allows to correctly discriminate which patients will not have adverse cardiac events, reducing the length of stay in ED.
Currently, this path has been proposed in some studies. Other research could confirm these data and be subsequently considered in future chest pain guidelines.
Abbreviations
ACS, Acute Coronary Syndrome; AOUS, Azienda Ospedaliera Universitaria Senese; CAD, Coronary Artery Disease; ED, Emergency Department; EKG, Electrocardiogram; HEAR, History, ECG, Age, Risk factors; MACE, major adverse cardiac events; NPV, negative predictive value; PPV, positive predictive value.
Ethics Approval and Consent to Participate
Ethics approval was acquired by the Hospital Healthcare Management of the AOUS. We were allowed from the dataset owner to use the information in databases for the purposes of the research. The present study did not involve the use of confidential or sensitive personal health information therefore the patient consent was not required. The study was conducted in compliance with the Helsinki Declaration of 975, as revised in October 2013 and all data were kept anonymous.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Aalam AA, Alsabban A, Pines JM. National trends in chest pain visits in US emergency departments (2006–2016). Emerg Med J. 2020;37(11):696–699. PMID: 32900857. doi:10.1136/emermed-2020-210306
2. Ko DT, Dattani ND, Austin PC, et al. Emergency department volume and outcomes for patients after chest pain assessment. Circ Cardiovasc Qual Outcomes. 2018;11(11):e004683. PMID: 30354285. doi:10.1161/CIRCOUTCOMES.118.004683
3. Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the acute cardiovascular care association. Eur Heart J Acute Cardiovasc Care. 2020;9(1):76–89. PubMed PMID: 31958018. doi:10.1177/2048872619885346
4. Smith LM, Ashburn NP, Snavely AC, et al. Identification of very low-risk acute chest pain patients without troponin testing. Emerg Med J. 2020;37(11):690–695. PubMed PMID: 32753395; PubMed Central PMCID: PMC7952041. doi:10.1136/emermed-2020-209698
5. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191–196. PubMed PMID: 18665203; PubMed Central PMCID: PMC2442661. doi:10.1007/BF03086144
6. O’Rielly CM, Andruchow JE, McRae AD. External validation of a low HEAR score to identify emergency department chest pain patients at very low risk of major adverse cardiac events without troponin testing. CJEM. 2022;24(1):68–74. PubMed PMID: 34273102. doi:10.1007/s43678-021-00159-y
7. Moumneh T, Sun BC, Baecker A, et al. Identifying patients with low risk of acute coronary syndrome without troponin testing: validation of the HEAR score. Am J Med. 2021;134(4):499–506.e2. PubMed PMID: 33127371. doi:10.1016/j.amjmed.2020.09.021
8. Tscherny K, Kienbacher C, Fuhrmann V, et al. Early identification of patients with chest pain at very low risk of acute myocardial infarction using clinical information and ECG only. Int J Clin Pract. 2020;74(8):e13526. PubMed PMID: 32383504; PubMed Central PMCID: PMC7507208. doi:10.1111/ijcp.13526
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
