Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
Healthcare Resource Utilization and Associated Costs in New Users of Empagliflozin versus DPP-4 Inhibitors and GLP-1 Agonists: A Comparative Analysis Based on Retrospective Real-World Data from German Sickness Funds
Authors Wilke T , Picker N, Müller S , Stürmlinger A, Deiters B, Dittmar A, Aberle J, Gabler M
Received 21 January 2022
Accepted for publication 21 April 2022
Published 2 May 2022 Volume 2022:14 Pages 319—332
DOI https://doi.org/10.2147/CEOR.S357540
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Thomas Wilke,1 Nils Picker,2 Sabrina Müller,2 Anna Stürmlinger,3 Barthold Deiters,4 Axel Dittmar,1 Jens Aberle,5 Maximilian Gabler3
1IPAM e.V., Wismar, Germany; 2Ingress-Health HWM GmbH, Wismar, Germany; 3Boehringer Ingelheim Pharma GmbH & Co.KG, Ingelheim, Germany; 4GWQ ServicePlus AG, Düsseldorf, Germany; 5Universitätsklinikum Hamburg-Eppendorf (UKE), Hamburg, Germany
Correspondence: Nils Picker, Ingress-Health HWM GmbH, Alter Holzhafen 19, Wismar, 23966, Germany, Tel +49 3841 758 1013, Fax +49 3841 758 1011, Email [email protected]
Purpose: Achieving good glycemic control in type 2 diabetes (T2DM) may require individualized pharmacological approaches. We aimed to compare direct healthcare costs in patients treated with empagliflozin (EMPA) compared to dipeptidyl peptidase-4 inhibitors (DPP-4i) or glucagon-like peptide-1 receptor agonists (GLP-1-RA).
Patients and Methods: This German claims data study included continuously insured persons with at least two outpatient diagnoses and/or one inpatient diagnosis of T2DM if they started EMPA, DPP-4i, or GLP-1-RA in 2015– 2018. Healthcare costs were assessed from therapy initiation until the end of data availability, death, or therapy discontinuation and compared among propensity score-matched cohorts.
Results: Of 24,465 patients included, 3285 received EMPA, 19,443 DPP-4i, and 1747 GLP-1-RA. Matched cohorts were balanced on baseline characteristics (EMPA versus DPP-4i: n1/n2 = 3100/3100 and EMPA versus GLP-1-RA: n3/n4 = 1346/1346). Mean total costs after start of DPP-4i were € 7009 (95%-CI: 6573– 7444) versus € 4274 (3982– 4566) for EMPA. Costs associated with GLP-1-RA treatment were also significantly higher compared with EMPA (€ 6851 [6183– 7518] versus € 4895 [4345– 5445]).
Conclusion: Although the individual clinical patient profile and physician assessment are paramount in treatment decisions, substantial differences in the economic impact of different antidiabetic therapies should be considered.
Keywords: type 2 diabetes mellitus, sodium-glucose cotransporter-2 inhibitor, DPP-4 inhibitors, GLP-1 receptor agonists, healthcare costs
Introduction
In Germany, the current estimates of the prevalence of diabetes range between 7.2% (population aged 18 to 79 years) based on health examination surveys of the Robert Koch Institute and 9.9% (among all age groups) based on statutory health insurance data.1 Patients with type 2 diabetes mellitus (T2DM) make up the largest share, with an estimated prevalence of 6.9 million diagnosed cases in 2015 and a projected future number of diagnosed cases of between 10.7 million (+54%) and 12.3 million (+77%) by 2040.2
According to the German National Disease Management Guideline on the Treatment of Type 2 Diabetes, there are multiple stages.3 If a patient is unable to achieve their individual therapy target through changing their lifestyle (ie, education on dietary change and enhanced physical activity), physicians will add different pharmacological therapies. This will depend on the patient’s presence or estimated risk of diabetes-associated cardiovascular and/or renal events. Metformin is first recommended as a monotherapy if there is no high risk for such events. Metformin plus sodium-glucose cotransporter type 2 inhibitors (SGLT-2i) or glucagon-like peptide-1 receptor agonists (GLP-1-RA) are recommended if the patient is already suffering from clinically relevant cardiovascular disease (CVD). Suppose the initial therapy strategy does not achieve the patient-individual therapy target after three to six months. In that case, physicians can opt for additional or alternative medications (including insulin, dipeptidyl peptidase-4 inhibitor [DPP-4i], SGLT-2i, GLP-1-RA, and sulfonylurea), or intensify the existing therapy.
SGLT-2i have been available since 2012 and are one of the newer treatment options for T2DM. In addition to the glucose-lowering effects, they positively affect body weight, blood pressure, blood uric acid levels, and inflammation.3 When added to the standard care, SGLT-2i can reduce the incidence of major cardiovascular events (non-fatal myocardial infarction, non-fatal stroke, and cardiovascular mortality) and improve renal outcomes in patients with chronic kidney disease (CKD) despite a lesser antihyperglycemic effect.4 Based on this evidence, the indications for SGLT-2i expanded to include a reduction in the risk of major cardiovascular events, coronary heart disease (CHD), and heart failure, respectively.5,6 Superiority in cardiovascular outcomes was also demonstrated for some GLP-1-RA when compared to placebo, while DPP-4i was found to have a neutral effect on the risk of heart failure.7–10
CVDs are reported to contribute up to 50% of healthcare costs in the treatment of T2DM, with hospitalizations and surgical resources being the main drivers of direct costs.11 However, there is little known about the costs and healthcare resource utilization (HCRU) associated directly with the antidiabetic regimen of T2DM patients, particularly when comparing SGLT-2i, DPP-4i and GLP-1-RA. This study aims to close this research gap by comparing the healthcare costs and HCRU of German T2DM patients who initiated the SGLT-2i empagliflozin (EMPA) versus DPP-4i and GLP-1-RA in routine clinical practice. In this study, we describe the expenditures from the perspective of the statutory health insurance funds in Germany. In addition, cost drivers are identified by disaggregating costs by inpatient and outpatient care and pharmacy sales. Finally, this study examines the causes for differences in economic impact by comparing the most common reasons for hospitalization between the comparison cohorts.
Materials and Methods
Data Source, Study Population, and Observational Period
This study retrospectively analyzed an anonymized claims dataset from GWQ ServicePlus AG covering over 4 million persons insured by different statutory health insurance companies across Germany. Generally, claims data of German sickness funds contain patient-level information on patients’ demographics and reimbursement-related data on outpatient care, inpatient care, and outpatient medication.
The analysis sample included all adult persons continuously insured between 01/01/2014 until 31/12/2018 or death who received at least one outpatient prescription with EMPA (ATC codes: A10BK03 [formerly A10BX12] and A10BD20), DPP-4i (ATC codes: A10BH*, A10BD07, A10BD08, and A10BD10), or GLP-1-RA (ATC codes: A10BJ* [formerly A10BX04, A10BX07, A10BX10, or A10BX14] and A10AE56) between 01/01/2015 and 31/12/2018, excluding all patients already receiving one of the respective agents in 2014 (12-month treatment-free period ensuring the identification of therapy starters). All patients included in the analysis were identified as having T2DM by observing at least one inpatient diagnosis (International Statistical Classification Of Diseases And Related Health Problems, 10th revision, German Modification [ICD-10-GM] code: E11) or at least two outpatient diagnoses in two different quarters within one year before the treatment initiation (index date). Finally, patients were excluded if another form of diabetes (type 1, gestational, or secondary diabetes), neoplasms (identified by diagnosis or prescriptions of cancer-related drugs), or one of the top three most cost-intensive diseases as defined by the German Federal Insurance Office (sepsis, human immunodeficiency virus [HIV], or opportunistic infections) have been diagnosed in the 12 months before the start of treatment.
Patients were observed starting from the first day of treatment initiation until the date of death, the end of data availability (31/12/2018), or the date of therapy discontinuation. Discontinuation of therapy was assumed if there was a gap in drug availability of at least 90 days, approximating the drug supply based on the quantity and the daily defined dose (DDD) of prescribed medication. If there was a gap in drug availability was observed, the end of the respective gap was considered the end of the treatment.
Study Variables
HCRU and costs were calculated from the perspective of the statutory health insurance (including outpatient and inpatient care as well as drug prescriptions). All costs and HCRU items were assessed in the available patient-individual follow-up period, investigating total all-cause costs. All costs are reported in Euros. No discounting was applied because the median follow-up time of the patients in this analysis was less than one year.
Costs for outpatient care were assessed according to the Uniform Valuation Scheme (EBM). In Germany, outpatient services are valued based on pre-defined weighted points that were multiplied by the EBM. The values used in this study ranged from €0.101300 per point in 2014 to €0.106543 per point in 2018.
Inpatient treatment costs were assessed per hospitalization according to the German “diagnosed-related-group” (G-DRG) reimbursement framework. Hospital financing for operating costs in Germany is based on a grouping algorithm, which considers major diagnosis, procedures, secondary diagnoses, length of stay, type of admission (emergency, referral from general practitioner or transfer from other hospitals), as well as patient characteristics (age and sex) to determine the G-DRG for each inpatient stay. The hospital payment for a patient treated is determined by multiplying the base case value by a fixed cost weight of the patient’s G-DRG, calculated by the Institute for the Hospital Remuneration System (InEK) on average costs as documented by a subsample of hospitals. The G-DRGs are collected from all German hospitals and transmitted to the sickness funds for payment to the hospitals. Hospital outpatient services are not included in this system.
Medication costs were calculated as costs for prescribed drugs according to the pharmacy sales price at the prescription date. Patient co-payments, reimbursement for medical aids/remedies, rehabilitation, and daily sickness allowance were not considered in this analysis. Due to medical progress and evolution of health policy legislation, costs for outpatient care, inpatient treatment costs, and medication costs are subject to future change. The utilization of healthcare resources was assessed in terms of the numbers of outpatient visits, the number of all-cause inpatient visits, and the number of prescribed DDDs of antidiabetic drugs.
For each patient, the following available baseline characteristics were measured within a 12-months baseline period: age (at index date), sex, binary indicators for the level of care at index date (degree of need for care according to statutory long-term care insurance; level I–V), the Charlson Comorbidity Index (CCI based on documented diagnoses excluding age factor; Supplementary Table 1), binary indicators for the use of prespecified antidiabetic and cardiovascular therapies (insulin, metformin, sulfonylurea, other antidiabetics, antithrombotic agents, beta-blocking agents [BB], calcium channel blockers, renin-angiotensin-aldosterone system [RAAS] inhibitors, lipid-lowering therapies [LLT]), binary indicators for prevalent CVD (ischemic stroke, myocardial infarction, CHD, or heart failure), documented alcohol abuse, documented nicotine dependence, the top ten most frequently diagnosed comorbidities (any outpatient or inpatient diagnosis) as well as T2DM-associated and non-T2DM-associated costs for outpatient physician visits, inpatient stays, and drug prescriptions.
Statistical Analysis
The comparability issue due to systematic differences in patient characteristics between treatment groups must be addressed when comparing non-randomized study cohorts. To compare HCRU and related costs of patients starting an EMPA treatment with patients who initiated therapy with DPP-4i or GLP-1-RA, respectively, a propensity score matching (PSM) approach was used to adjust for potential differences in patient characteristics and prior disease and treatment history among these cohorts. Patients starting EMPA versus either DPP-4i or GLP-1-RA were matched 1:1 based on a propensity score using a nearest-neighbor matching algorithm without replacement and a maximum caliper of 0.001. The propensity scores were derived by logistic regression models estimating the probability of a patient belonging to the different treatment groups (two estimations: EMPA versus DPP-4i and EMPA versus GLP-1-RA). In addition, four prespecified subgroup analyses were performed to determine differences between patients who had started treatment with any of the above agents as i) monotherapy, ii) add-on therapy with insulin, iii) therapy without insulin, or iv) dual therapy with metformin. A separate comparison was performed in a further prespecified sensitivity analysis between EMPA and the individual GLP-1-RAs dulaglutide (DULA) and liraglutide (LIRA). An overview of all the variables included in the logistic regression models estimating the propensity scores for each comparison is provided in Supplementary Table 2.
Descriptive statistics for baseline characteristics were summarized for all patients in the unmatched and matched cohorts for each index therapy. The differences in baseline characteristics between the groups (EMPA versus DPP-4i/GLP-1-RA) before and after the matching were tested for statistical significance using t-tests. The group differences in the costs incurred after treatment initiation were evaluated based on an incremental cost approach using the Bang and Tsiatis estimator with possibly censored data, as previously described by Chen et al 2015.12,13 The group differences in the utilization of healthcare resources investigated in the follow-up period were assessed by the ratio of total items utilized per observable person-years (PY). In addition, differences in the hospitalization rates were assessed by reporting the event rate ratios separately for different admission reasons (most frequently observed main diagnoses).
All analyses were performed using STATA (Version 14.1), Microsoft Excel (version 2105), and MySQL (Version 17.9.1).
Results
Patient Characteristics
The stepwise procedure selecting eligible patients is presented in Figure 1. Overall, 24,465 T2DM patients newly treated with EMPA, DPP-4i, or GLP-1-RA were observed. The mean age at index date was 60.0/63.3 years in the unmatched groups for EMPA versus DPP-4i (p<0.001; Table 1), and 60.0/55.0 for EMPA versus GLP-1-RA (p<0.001; Table 2). Fewer women were represented in the EMPA cohort (33.8%) compared with DPP-4i (39.6%) and GLP-1-RA (43.2%). The mean Charlson Comorbidities Index (CCI), measured within the 12-month baseline period before the first prescription date, was 7.4 in EMPA treated patients, 7.2 in DPP-4i treated patients, and 7.5 in GLP-1-RA treated patients. Within the group of unmatched EMPA patients, 39.5% had experienced a major cardiovascular event (non-fatal ischemic stroke or myocardial infarction) or were diagnosed with CHD or heart failure. In contrast, these comorbidities were present in 26.3% (p<0.001) of patients with DPP-4i and 32.3% (p<0.001) of patients with GLP-1-RA. There were no substantial differences in the frequency of other comorbidities observed among the three cohorts in this study (see Tables 1 and 2).
 |
Table 1 Patient Characteristics – EMPA versus DPP-4i |
 |
Table 2 Patient Characteristics – EMPA versus GLP-1-RA |
 |
Figure 1 Attrition chart. |
In the DPP-4i cohort, the vast majority of patients (94.6%) were treated with sitagliptin. Other active ingredients of this group included saxagliptin (5.4%) and vildagliptin (>0.1%). Among the patients using GLP-1-RA, DULA (60.3%) and LIRA (35.0%) accounted for the largest proportions. Exenatide was received by 4.7% of patients. With respect to previous antidiabetic medication, 31.2% of EMPA patients with prior exposure to insulin were observed. In comparison, the proportion of insulin-experienced patients was substantially smaller in users of DPP-4i (15.7%; p<0.001), while the GLP-1-RA cohort included significantly more patients with prior insulin use than the EMPA cohort (54.3%; p<0.001). Metformin was the most commonly used antidiabetic drug at baseline in all three groups (EMPA: 78.1%, DPP-4i: 74.8%, GLP-1-RA: 70.9%). Furthermore, EMPA patients were significantly more likely to receive cardiovascular medications (antithrombotic therapy: 31.7%, LLT: 52.6%, RAAS inhibition: 71.9%) than patients starting treatment with DPP-4i/GLP1-RA (antithrombotic therapy: 27.5%/23.2%, LLT: 44.0%/40.3%, RAAS inhibition: 68.4%/70.3%; p<0.001 for each comparison).
In the PSM comparison versus patients on DPP-4i, 94.7% of whom had received sitagliptin, all differences described above could be adjusted for (sample size per matched cohort 3100; overall mean/median bias for observable covariates after matching: 1.2/0.9%). The same applied to the comparison between starters of EMPA and GLP-1-RA (sample size per matched cohort 1346; overall mean/median bias for observable covariates after matching: 2.6/2.2%). Within the GLP-1-RA cohort post-matching, 59.3% of patients were treated with dulaglutide, 35.8% with liraglutide, and 4.9% of patients were treated with exenatide.
Comparison of Healthcare Costs After Matching
Figure 2 summarizes the observed total direct costs for healthcare among matched cohorts of EMPA patients compared with starters of DPP-4i and GLP-1-RA. The median follow-up time in the EMPA group was 242 days when matched to DPP-4i (versus 458 days) and 259 days when matched to GLP-1-RA (versus 302 days). After adjustment for differences in length of follow-up, there were significantly higher expenses for healthcare observed among patients initiating DPP-4i (mean: € 7009 versus € 4274) and GLP-1-RA (mean: € 6851 versus € 4895) in comparison with EMPA. The highest differences between EMPA and DPP-4i were observed for inpatient care (€ 1455 versus € 3040; p<0.001) and pharmacy sales of prescribed drugs (€ 1966 versus € 2689; p<0.001), whereas incremental cost differences versus GLP-1-RA were mainly driven by medication costs alone (€ 2433 versus € 3575; p<0.001). These results were consistent across all pre-defined therapeutic subgroups (monotherapy, insulin-naïve, add-on to insulin, and dual therapy with metformin); (Supplementary Figure 1). A further comparison of EMPA versus DULA and EMPA versus LIRA, did not show any agent-specific cost effects compared to EMPA versus total GLP-1-RA (Supplementary Figure 2).
 |
Figure 2 Total direct cost of any cause by initiated therapy (matched cohorts). |
Comparison of Healthcare Resource Use After Matching
In line with the observed cost difference, the rate of hospitalizations per year over the entire observation period was substantially lower in the EMPA cohort compared to patients starting treatment with DPP-4i (35 versus 46 hospital admission per 100 PYs). The same proved true for the comparison between EMPA and GLP-1-RA (32 versus 40 per 100 PYs). Still, higher costs per hospitalization were observed in the EMPA cohort (€ 4930 versus € 4496), resulting in similar inpatient expenditures when comparing both cohorts. Table 3 reports the top ten reasons for hospitalization across the PS-matched cohorts for new users of EMPA, DPP-4i, and GLP-1-RA. Eight of the ten most common diagnoses for hospital admission were related to CVD, indicating the paramount importance of reducing cardiovascular risk in this patient population. Overall, patients starting EMPA had fewer hospitalizations per observed year than their respective comparison groups. Fewer hospitalizations are associated with reduced heart failure events, which is the greatest advantage of EMPA over DPP-4i and GLP-1-RA (−1.23 events per 100 PYs versus DPP-4i; −0.84 events per 100 PYs versus GLP-1-RA). These results are consistent with the results of cardiovascular outcome studies for DPP-4i, GLP-1-RA, and EMPA published during the last years.
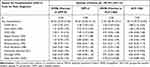 |
Table 3 Top 10 Reasons for Hospitalization in PS-Matched Cohorts |
Quarterly invoiced outpatient visits were more frequently observed in patients initiating EMPA (3.36 visits per PY) when compared to DPP-4i (3.01 visits per PY), while patients who received GLP-1-RA had the highest outpatient-visit rate (3.79 visits per PY versus 3.36 per PY with EMPA). No substantial differences were found between the study cohorts in terms of average cost per outpatient visit.
With respect to prescriptions of antidiabetic drugs, the highest resource use in terms of received DDDs was observed in patients starting GLP-1-RA (415 DDDs per PY), whereas comparable drug consumption as measured by the prescribed DDDs was observed for patients receiving DPP-4i (333 DDDs per PY) or EMPA (334–336 DDDs per PY).
Discussion
This retrospective analysis of a nationwide German claims dataset, covering the years 2015–2018, compared direct medical costs and HCRU among a sample of prevalent T2DM patients starting an antidiabetic treatment with EMPA versus DPP-4i or GLP-1-RA. An evaluation of propensity-score matched cohorts identified substantially higher costs for inpatient care in patients starting DPP-4i compared with EMPA. The differences in cost between EMPA and GLP-1-RA were mainly attributed to the higher drug price and the intensified dosing of the latter, resulting in higher medication costs.
While previous claims data studies from the US already highlighted that SGLT-2i are associated with longer treatment persistence and reduced healthcare utilization and cost savings relative to DPP-4i and GLP-1,14,15 this paper reinforces previous findings with novel data for the German statutory health insurance (SHI) context.
For the cross-class comparison with DPP-4i, reimbursement for CVD-related inpatient care was found to contribute significantly to the higher incremental costs than EMPA. This is in line with previous findings from the cardiovascular outcome trials EMPA‐REG OUTCOME, TECOS, and SAVOR-TIMI 53, suggesting a significantly reduced risk for CVD-related hospitalizations for EMPA compared to DPP-4i, such as sitagliptin or saxagliptin.16,17 Among the known diabetes-related complications, CVD is the most prevalent cause of morbidity and mortality in patients with T2DM,18 which yields considerable cost benefits for EMPA. Furthermore, nearly half of all deaths in patients with T2DM are due to increased CV risk of myocardial infarction and stroke.19 Although hospitalizations due to renal complications were rarely observed, the number of documented cases was more than three times higher in DPP-4i patients (0.66 per 100 PYs) than in EMPA patients (0.21 per 100 PYs). In contrast, event rates were similar between GLP-1-RA and EMPA. These figures are consistent with recent studies finding positive renal effects of SGLT-2i and, to some extent, GLP-1-RA.4,20,21 However, due to the low hospitalization rate caused by renal failure, no relevant economic impact was shown in this study.
We found no significant cost differences in hospital expenditures between GLP-1-RA and EMPA. While some individual GLP-1 agonists, such as liraglutide and dulaglutide, have shown CV benefit in patients with established CVD in placebo-controlled trials,7,10 the lack of difference versus EMPA is consistent with other real-world studies comparing GLP-1-RA and SGLT-2i, where both were associated with a similar risk for hospitalization due to major CV events, severe hypoglycemia, and fractures.22,23 In addition, a recent US claims data analysis showed that switching from DPP-4i to GLP-1-RA or SGLT-2i was associated with fewer hospitalizations; however, higher pharmacy costs, particularly for GLP-1-RAs, outweighed the savings from reduced hospitalizations.24
Nevertheless, our study demonstrated a significant cost advantage of EMPA over GLP-1-RA when comparing direct healthcare expenditure after therapy initiation. This was also confirmed in a direct comparison with the individual agents dulaglutide and liraglutide. The cost difference was most evident when analyzing the reimbursement for drug prescriptions between both drug classes, which accounts for nearly 60% of EMPA’s cost benefit. While drug prices in Germany are substantially higher per average daily dose for GLP-1 RA compared to EMPA: (3.62–4.24 Euro/DDD versus 2.36 Euro/DDD; gross price according to Lauer-Taxe as of December 11, 2018), a quantity effect in favor of EMPA was additionally observed, indicating more frequent treatment intensification with GLP-1-RA. Accordingly, the prescribed number of daily doses for GLP-RA-1 exceeded the expected recommended daily dose on average by more than 13%. In patients who started EMPA, the dose consumption per PY was even slightly below the recommended amount (−8%). Similar utilization patterns for GLP-1-RA were described in a retrospective cohort study in Italian patients with T2DM.25
Limitations
Unlike other observational studies, this study was based on a large nationwide database that is free from selection bias. Nevertheless, several other limitations exist. Since patients receiving various classes of antidiabetic agents (ie, SGLT-2i, DPP-4i, and GLP-1-RA) differ widely in terms of sociodemographic characteristics, certain comorbidities, and medication history, PSM was applied. While this improved comparability across cohorts by balancing prespecified observable covariates, residual unobservable factors may present bias in the comparative analysis of matched cohorts. When new therapies become reimbursable, there is often an increase in prescribing these drugs in individuals who have not responded to previous therapies and are at higher risk for complications and associated higher healthcare costs. Since empagliflozin and dulaglutide recently came to the market in 2014, we cannot exclude the possibility that these agents were prescribed more frequently to patients who had not responded to other oral antidiabetic agents (eg, sulfonylureas) or insulin. Consequently, these patients are more likely to be associated with higher healthcare costs. Another limitation of this study was the degree of glycemic control at baseline (commonly quantified in terms of HbA1c values), which could not be captured in this analysis and was therefore not controlled within the matching procedure. In addition, several risk factors of major importance for cardiovascular outcomes, such as body weight, blood pressure, LDL-cholesterol level, or smoking status were assessed only in severe cases, for example, when a diagnosis of obesity, hypertension, hypercholesterolemia, or history of nicotine dependence was documented based on the ICD-10 classification. However, given that the included observable characteristics are proxies for unobservable clinical parameters, the selection bias in this large database study is expected to be minor. Nevertheless, the matching quality for the comparison between EMPA and GLP-1-RA was somewhat limited due to the smaller sample size, as GLP-1-RAs were prescribed less frequently in the source population. This resulted in a non-significant minor bias in major cardiovascular diseases (heart failure, CHD, myocardial infarction, or ischemic stroke) present at baseline.
Furthermore, because DPP-4i and GLP-1-RA (first approved in 2006) have received approval for the treatment of patients with T2DM for a significantly longer period of time than EMPA (approved in 2014), there is a substantial difference in observable length of follow-up between the compared study cohorts (median duration for DPP-4i matched to EMPA: 8.1 months versus 15.3 months), since more patients initiating treatment with EMPA were identified towards the end of the study period, while the opposite was true for patients starting DPP-4i and GLP-1-RA. These differences were evident in terms of distribution by index year (year of treatment initiation), particularly in the proportion of patients who received their first prescription in 2015. Of the matched EMPA patients, only 8.2% had started their treatment in 2015, whereas 29.6% had received DPP-4i. This difference was also significant when comparing EMPA (10.2%) and GLP-1-RA (25.6%). Therefore, there is a possibility of bias due to informative censoring, as long-term effects could be observed less frequently in patients on EMPA than on DPP-4i or GLP-1-RA. However, a sensitivity analysis limiting the observation period to the first year of treatment showed similar cost benefits for EMPA compared with DPP-4i and GLP-1-RA, respectively (Supplementary Figure 3).
There were no substantial differences between the matched cohorts with respect to discontinuation rates. Of those patients who had started EMPA, 60.8% had discontinued or switched therapy compared with those who had started DPP-4i (56.9%). Discontinuation rates were slightly higher in patients starting EMPA (62.9%) compared with GLP-RA-1 (55.4%). With respect to the defined follow-up periods, it should be noted that drug persistence for the evaluated antidiabetic therapies was only approximated based on prescription data and obtained pack sizes. However, the grace period, which determines the follow-up period for drug exposure and censoring in case of treatment discontinuation (medication refill gap > coverage of the last prescription according to DDD observed + 90 days), represents a relatively broad definition but is still consistent with applied ranges in the previous literature.26–28 In addition, potential delayed treatment effects after discontinuation of therapy should be considered, especially in the context of treatment of chronic diseases such as T2DM and CVD.
Conclusions
Our analysis demonstrated that T2DM patients who initiated EMPA therapy had lower healthcare expenses in the proceeding course of treatment than those starting DPP-4i and GLP-1-RA. In particular, patients newly treated with EMPA had lower inpatient costs than DPP-4i users, mainly due to lower rates of CVD-related hospitalizations, such as heart failure. The results of this study indicate that treatment with DDP-4i, which is widely prescribed in Germany, is not a cost-effective option despite the lower drug price compared to EMPA. Healthcare providers should therefore reconsider their current treatment patterns. The cost advantage for EMPA over GLP-RA-1 was mainly due to the difference in direct medication costs. Further studies are recommended to confirm these results, particularly concerning the real-world efficacy of SLGT-2 inhibition in heart failure.
Data Sharing Statement
The dataset analyzed during the current study are not publicly available due to German data protection law for social insurance data (SGB X).
Ethics Approval and Informed Consent
This work was a non-interventional retrospective study based on anonymized data provided by GWQ ServicePlus AG under formal agreement. In accordance with German laws (§ 75 SGB X), the use of such data is not subject to ethics committee approval no informed consent was required. The study was coordinated and led by a Scientific Steering Committee (SSC). All authors were part of the SSC.
This study fulfilled the criteria of European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP; EU PAS Register Number: 31950) and followed the “ENCePP Code of Conduct”.29
Funding
The study was funded by Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany.
Disclosure
Thomas Wilke and Axel Dittmar participated in this study as staff members of IPAM. Nils Picker and Sabrina Müller participated in this study as staff members of Ingress-health; the work of IPAM and Ingress-health in this study was financed by Boehringer Ingelheim Pharma GmbH & Co. KG. Anna Stürmlinger and Maximilian Gabler are employees of Boehringer Ingelheim Pharma GmbH & Co. KG. Jens Aberle participated as external clinical advisor in the scientific steering committee of this study and received honoraria from Boehringer Ingelheim Pharma GmbH & Co. KG. The authors report no other conflicts of interest in this work.
References
1. Heidemann C, Scheidt-Nave C. Prevalence, incidence and mortality of diabetes mellitus in adults in Germany – a review in the framework of the diabetes surveillance. J Heal Monit. 2017;2(3):98–121.
2. Tönnies T, Röckl S, Hoyer A. Projected number of people with diagnosed type 2 diabetes in Germany in 2040. Diabet Med. 2019;36(10):1217–1225. doi:10.1111/DME.13902
3. Kassenärztliche Bundesvereinigung, Bundesärztekammer. Nationale Versorgungsleitlinie Typ-2-Diabetes: Teilpublikation der Langfassung, 2. Auflage, [National care guideline for type 2 diabetes: partial publication of the long version, 2nd edition], Version 1. 2021. Available from: www.leitlinien.de.
4. Nespoux J, Vallon V. Renal effects of SGLT2 inhibitors: an update. Curr Opin Nephrol Hypertens. 2020;29(2):190. doi:10.1097/MNH.0000000000000584
5. Committee for Medicinal Products for Human Use (CHMP). Jardiance summary of opinion (post authorisation). Available from: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-jardiance-ii-55_en.pdf.
6. Committee for Medicinal Products for Human Use (CHMP). Forxiga summary of opinion (post authorisation). Available from: https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-forxiga-ws-1737_en.pdf.
7. Schuster MA, Reisner SL, Onorato SE. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):101. doi:10.1056/NEJMOA1603827
8. Hernandez AF, Green JB, Janmohamed S. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (harmony outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392(10157):1519–1529. doi:10.1016/S0140-6736(18)32261-X
9. Cardiovascular AJS. Effects of new oral glucose-lowering agents: DPP-4 and SGLT-2 Inhibitors. Circ Res. 2018;122(10):1439–1459. doi:10.1161/CIRCRESAHA.117.311588
10. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–130. doi:10.1016/S0140-6736(19)31149-3
11. Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value Health. 2018;21(7):881–890. doi:10.1016/J.JVAL.2017.12.019
12. Bang H, Tsiatis A. Estimating medical costs with censored data. Biometrika. 2000;87(2):329–343. doi:10.1093/BIOMET/87.2.329
13. Chen S, Rolfes J, Zhao H. Estimation of mean health care costs and incremental cost-effectiveness ratios with possibly censored data. Stata J. 2015;15(3):698–711. doi:10.1177/1536867X1501500305
14. Poonawalla IB, Bowe AT, Tindal MC, Meah YA, Schwab P. A real-world comparison of cardiovascular, medical and costs outcomes in new users of SGLT2 inhibitors versus GLP-1 agonists. Diabetes Res Clin Pract. 2021;175:108800. doi:10.1016/J.DIABRES.2021.108800
15. Reifsnider O, Kansal A, Pimple P, Aponte‐Ribero V, Brand S, Shetty S. Cost‐effectiveness analysis of empagliflozin versus sitagliptin as second‐line therapy for treatment in patients with type 2 diabetes in the United States. Diabetes Obes Metab. 2021;23(3):791. doi:10.1111/DOM.14268
16. Ramos M, Foos V, Ustyugova A, Hau N, Gandhi P, Lamotte M. Cost-effectiveness analysis of empagliflozin in comparison to sitagliptin and saxagliptin based on cardiovascular outcome trials in patients with type 2 diabetes and established cardiovascular disease. Diabetes Ther. 2019;10(6):2153. doi:10.1007/S13300-019-00701-3
17. Kansal A, Reifsnider OS, Proskorovsky I, et al. Cost‐effectiveness analysis of empagliflozin treatment in people with Type 2 diabetes and established cardiovascular disease in the EMPA‐REG outcome trial. Diabet Med. 2019;36(11):1494. doi:10.1111/DME.14076
18. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83. doi:10.1186/S12933-018-0728-6
19. Leon BM. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6(13):1246. doi:10.4239/WJD.V6.I13.1246
20. Prischl FC, Wanner C. Renal outcomes of antidiabetic treatment options for type 2 diabetes—a proposed mare definition. Kidney Int Rep. 2018;3(5):1030–1038. doi:10.1016/J.EKIR.2018.04.008
21. Mosterd CM, Bjornstad P, van Raalte DH. Nephroprotective effects of GLP-1 receptor agonists: where do we stand? J Nephrol. 2020;33(5):965–975. doi:10.1007/S40620-020-00738-9/FIGURES/1
22. Patorno E, DH Kim, Pawar A, et al. 156-OR: risk-benefit of SGLT2 inhibitors (SGLT2i) vs. GLP-1 receptor agonists (GLP-1RA) in routine care of older adults. Diabetes. 2019;68(Supplement1). doi:10.2337/DB19-156-OR
23. Pineda ED, Liao I-C, Godley PJ, Michel JB, Rascati KL. Cardiovascular outcomes among patients with type 2 diabetes newly initiated on sodium-glucose Cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, and other antidiabetic medications. J Manag Care Spec Pharm. 2020;26(5):610–618B. doi:10.18553/JMCP.2020.26.5.610
24. Newman TV, Munshi KD, Neilson LM. Health care utilization and costs associated with switching from DPP-4i to GLP-1RA or SGLT2i: an observational cohort study. J Manag Care Spec Pharm. 2021;27(4):435–443.
25. Federici MO, McQuillan J, Biricolti G, et al. Utilization patterns of glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus in Italy: a retrospective cohort study. Diabetes Ther. 2018;9(2):789. doi:10.1007/S13300-018-0396-2
26. Weisman A, King LK, Mamdani M. Reporting and variability of constructing medication treatment episodes in pharmacoepidemiology studies: a methodologic systematic review using the case study of DPP −4 inhibitors and cardiovascular outcomes. Pharmacoepidemiol Drug Saf. 2020;29(8):939–950. doi:10.1002/PDS.5071
27. Parker MM, Moffet HH, Adams A, Karter AJ. An algorithm to identify medication nonpersistence using electronic pharmacy databases. J Am Med Inform Assoc. 2015;22(5):957–961. doi:10.1093/JAMIA/OCV054
28. Alfian SD, Denig P, Coelho A, Hak E. Pharmacy-based predictors of non-adherence, non-persistence and reinitiation of antihypertensive drugs among patients on oral diabetes drugs in the Netherlands. PLoS One. 2019;14(11). doi:10.1371/JOURNAL.PONE.0225390
29. ENCePP code of conduct; 2018. Available from: https://www.encepp.eu/code_of_conduct/index.shtml.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
