Back to Journals » Patient Preference and Adherence » Volume 17
Health-Related Quality of Life for Jordanian-Recovered Individuals During Post-COVID-19 Era: A Cross-Sectional Study
Authors Abuhammad S , Khabour OF, Alzoubi KH, Hamaideh S, Khassawneh BY, Mehrass AAO, Alsmadi BF, Ababneh AM
Received 14 April 2023
Accepted for publication 13 May 2023
Published 22 May 2023 Volume 2023:17 Pages 1303—1310
DOI https://doi.org/10.2147/PPA.S415336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sawsan Abuhammad,1 Omar F Khabour,2 Karem H Alzoubi,3,4 Shaher Hamaideh,5 Basheer Y Khassawneh,6 Amat Al-Khaleq O Mehrass,7 Baha F Alsmadi,6 Abdelrahman M Ababneh6
1Department of Maternal and Child Health, Faculty of Nursing, Jordan University of Science and Technology, Irbid, 22110, Jordan; 2Department of Medical Laboratory Sciences, Jordan University of Science and Technology, Irbid, 22110, Jordan; 3Department of Pharmacy Practice and Pharmacotherapeutics, College of Pharmacy, University of Sharjah, Sharjah, United Arab Emirates; 4Department of Clinical Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 5Department of Community and Mental Health Nursing, Faculty of Nursing, The Hashemite University, Zarqa, 13133, Jordan; 6Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 7Department of Obstetric and Gynecology, Thamar University, Dhamar, Yemen
Correspondence: Amat Al-Khaleq O Mehrass, Email [email protected]
Aim: This study aims to determine health-related quality of life (HRQoL) that includes the physical and mental health of recovered patients of COVID-19 and examines the significant impact of variables such as period of infection, sample demographics characteristics, hospitalization past, and chronic disease past and the other variables on HRQoL of COVID-19-recovered patients.
Methods: An exploratory, community-based, cross-sectional research layout was adopted, using an electronic self-reporting survey disseminated online to recovered COVID-19 patients in Jordan. Targeted COVID-19 patients were individuals who were 18 years old or above. They had a documented background of COVID-19 illness, as stated in the following inclusion requirements: Those who had not been formally proven to have been afflicted by COVID-19 were excluded.
Results: The mean of the physical well-being of study participants during COVID-19 was M=68.00 (SD=6.95), representing medium physical well-being status. The mean of psychological well-being of study participants during COVID-19 was M=60.20 (SD=8.85), representing medium physical health. Multiple regression showed that female recovered patients who are not working, with a low level of income, married women, and who getting COVID-19 more than once are having lower health-related quality of life compared to other recovered patients.
Conclusion: The HRQoL of COVID-19 patients was significantly impacted, independent of the period since hospitalization or rehabilitation. Policymakers and health workers should research strong ways to enhance the HRQoL of COVID-19 patients as soon as possible. Elderly patients and those who have been infected more than one time and being hospitalized have a greater probability of decreased HRQoL after infection.
Keywords: mental health, physical health, COVID-19, recovered
Introduction
The COVID-19 pandemic affects the general population’s health-related quality of life (HRQoL) in numerous nations, notably in terms of physical, psychological, social, and spiritual health.1,2 The HRQoL defined as “how well a person functions in their life and his or her perceived well being in physical, mental, and social domains of health”.3 COVID-19 also impacted the health-related quality of life of many individuals.4,5 Numerous studies have shown that people infected with COVID-19 exhibit a wide range of symptoms during and after the illness.4,6–10 Every day, more information on the COVID-19 outbreak’s impact on physical and mental health is published.11,12 Furthermore, COVID-19 is a multiorgan illness; many individuals will need a comprehensive rehabilitation effort by a multidisciplinary team to allow recovery.13–15 COVID-19 is also anticipated to significantly influence the well-being and health-related quality of life of recovered patients, given the rising number of COVID-19 patients and the high percentage of persons who are admitted and need ICU treatment for infection control.16–19 However, given the brief period of the SARS-CoV-2 pandemic, only a limited amount of scientific information on the physical function and health-related quality of life implications of COVID-19 is known.20,21
Another essential consideration in COVID-19-recovered patients is that lengthy periods of motion limitation and the illness itself might compromise physical function due to decreased strength and endurance, range of motion, and breathing ability, among other things.22,23 As a result, there are deficits in completing everyday living tasks, limiting the patient’s freedom and autonomy, and lowering their quality of life.24,25 A greater understanding of the functional consequences of COVID-19 can aid in developing and implementing disability recovery methods and treatments that can enhance the health-related quality of life.26,27 COVID-19 patients who have been released HRQoL, particularly physical and psychological well-being, are subpar after a month. It has been found that their health-related quality of life (HRQoL) is still significantly lower than that of the general population after hospitalization.28,29 However, there were no studies in Jordan conducted for recovered patients who suffered from moderate-to-severe symptoms—significant influence in the area of mental health.
Pizarro-Pennarolli et al30 recently conducted a literature review to evaluate the influence of COVID-19 on adult patients’ activities of daily living performance and to explain the typical scales used to measure patients’ activities of daily living performance post-COVID-19. All nine studies in the review showed impaired performance in activities of daily living, demonstrating a critical deterioration of functional capacity in daily tasks, living productivity, and, as a result, loss of autonomy in COVID-19 patients following the acute phase of illness. Despite this, we are aware of no published study that examined the influence of COVID-19 on recovered physical function and health-related quality of life.
As a result, the authors conducted this study to evaluate the HRQoL of recovered COVID-19 patients in Jordan. This study aims to determine the physical and mental health of recovered patients of COVID-19 and examine the significant impact of variables such as the period of infection, sample demographics characteristics, hospitalization past, and chronic disease past and the other variables on HRQoL of COVID-19-recovered patients. In addition, all or some HRQoL components were predicted to be negatively impacted by sociodemographic and other variables, including immunization goals, time since infection, and perceptions of COVID-19’s influence on wellness and hospitalization.
Method
An exploratory, community-based, cross-sectional design was adopted in this study, using an electronic self-reporting survey disseminated online to recovered COVID-19 patients in Jordan.
Sample and Procedure
Targeted COVID-19 patients were individuals who were 18 years old or above and had a documented background of COVID-19 illness. Those who had not been formally proven infected by COVID-19 were excluded. With 95% statistical power and a 0.5 error margin, the computed size of the collection was predicted to achieve a total of 2000 responses. The final number of people who received the survey was 2100. From April to June 2022. Responses for the online survey that were distributed to eligible participants were gathered utilizing social media (eg, WhatsApp, Twitter, and text messaging) after the participants signed informed consent to participate in the study. It is worth mentioning that data collection of this study covered all cities in Jordan and advertised all over the social media to reach a greater number of people. The authors were provided their contact information for any question that related to the study from 8 am to 8 pm during data collection time.
Description of Instrument
A 36-item self-report survey that evaluates eight aspects of a person’s physical and psychological health was used to calculate a person’s Health-Related Quality of Life (HRQoL) on a range from 0 to 100. The eight components that comprise well-being are muscular strength (role-physical), bodily discomfort, overall health assessments, energy, cognitive relationships, mental wellbeing (role-emotional), and overall cognitive well-being. Physical health is represented by the first four factors, while the remaining eight capture the mental state.31 The study was considered valid and reliable with Cronbach's alpha being 0.84.32 The Cronbach's alpha for the HRQoL in this study was 0.87.
Ethical Consideration
The Institutional Review Board (IRB# 708-2021) at Jordan University of Science and Technology approved this study. Also, for the participants who can participate in the study, approval was taken before starting the data collection. The study complies with the Declaration of Helsinki.
Data Analysis
The study used SPSS (Statistical Package for the Social Sciences) for Windows (Standard Version 24, IBM Corp. Released 2016). IBM SPSS Statistics 24.0 for Windows was used to examine the data (Armonk, NY: IBM Corp.). The frequency of values that were missing in this set of data was less than 5% across all of the items. A multivariate diagnostic test to investigate the degree of unpredictability in the missing data identified. The research found that the missing pattern was entirely coincidental (p > 0.05). For the missing scores, the mean/median of the non-missing items was imputed, and all analyses were repeated with and without imputed data, showing no significant changes. First, we used numerical and percentage descriptions of our primary and secondary data sources. Then we used the one-sample Kolmogorov–Smirnov test to ensure that our data were normally distributed. Multiple regressions test was used to determine the predictors of HRQoL after checking for the collinearity. No variable was found with VIF with more than 10.
Results
Demographic of Participants
The response rate of the participants was 2055 (98%). The study included 873 (42.5%) males, and 1182 (57.5%) females. The study included people of all age levels. See Table 1
 |
Table 1 Demographic Characteristics of the Participants (N=2055) |
Description of Physical Health and Psychological Health of Recovered Patients
Physical well-being was measured among Jordanian women using the sf-36 V2.
The instrument was originally set to yield a score from (30–70). The mean of physical well-being of study participant during COVID-19 was M=68.00 (SD=6.95), which represented medium physical well-being status. The mean of psychological well-being of study participants during COVID-19 was M=60.20 (SD=8.85), which represented medium physical health. See Table 2 and Table 3.
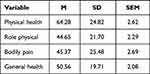 |
Table 2 Description of the Four Domains of Physical Health Scores Among Jordanian Participants (n=2055) |
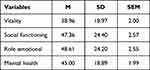 |
Table 3 Description of the Four Domains of Mental Health Scores Among Jordanian Participants (n=2055) |
Predictors of HRQoL of Life
The model was significant (F=13.54, P=0.01). This means many factors will predict the health-related quality of life of the patients. These factors were gender (B=0.085, P=0.002), working status (B=0.088, P=0.001), income level (B=0.084, P=0.000), marital status (B=0.067, P=0.013), and number of times having COVID (B=0.197, P=0.00). This means female recovered patients, those who are not working, with a low level of income, married women, and who are getting COVID-19 more than one are having lower health-related quality of life compared to other recovered patients. See Table 4
 |
Table 4 Predictors of Health-Related Quality of Life Among Recovered COVID-19 Patients (n=2055) |
Discussion
Unfortunately, our findings show that the effects of COVID-19 continue even after patients are hospitalized and recovered from COVID-19 infection. In this study, the authors could contact 2055 individuals after recovering from illness from COVID-19 infection. In line with this theory, numerous cohort studies31,33 twice to thrice higher were essentially twice to thrice higher than before COVID-19. However, our findings showed that many recovered patients can recover long after the acute phase has passed.
Our results showed decreases in physical activity, bodily pain, and general health if we compared it to people in other studies before the COVID-19 era. Regardless of the scale used, the data demonstrated a deterioration in everyday living ability following COVID-19 infection. According to Belli et al,34 COVID-19 results in a loss of autonomy and dignity for the recovered COVID-19 patients which can have a detrimental influence on their quality of life. According to Clemente-Suárez et al,35 COVID-19 has a deleterious impact on sensorimotor, levels of daily exercise, dietary habits, and mental wellbeing. Furthermore, immobility during acute sickness might result in a loss of body function, which can have an influence on everyday activities.29 These variables may be linked to physical and functional deterioration, as well as decreased performance in everyday tasks. As a result, further study is required to discover the variables related to impaired functioning and everyday activities, as well as the best rehabilitation methods.
Our results showed a decrease in mental health, vitality, social function, and role function compared to studies that were conducted before COVID-19 era. The study of Guo et al36 also showed a decrease in all domains of mental health. Dorri et al37 showed that all four components of mental health declined compared to other studies that were conducted before COVID-19.
Finally, our study found that female recovered patients, not working, with low levels of income, married women, and who getting COVID-19 more than once are having low health-related quality of life compared to other recovered patients. One study found that admission to the intensive care unit was a significant predictor of declining HRQoL. Similarly, a study provides conclusive evidence that COVID-19 negatively affects wellness, quality of life, and mental well-being. Previous studies that used objective methods to evaluate HRQoL in recovered COVID-19 patients indicated that those admitted to the critical care unit had worse health-related quality of life scores than those treated on the wards, notably in the pain/discomfort area.26,38 Our research confirms their conclusions but also adds to the literature on the topic.
The current study is one of the first to evaluate patients’ HRQoL and psychological health during the post-COVID-19 era. Many COVID-19 patients are elderly or have other chronic medical illnesses, so it is essential to know whether their decreased health-related quality of life after being discharged from the hospital directly results from their illness.38,39 Patient responses to the quality-of-life questionnaire were compared to those given before the beginning of COVID-19 symptoms, allowing researchers to show that all five domains were negatively impacted by the condition, with pain/discomfort and anxiety/depression being the most pronounced. Studies also showed that a greater fall in quality-of-life scores was linked to a poorer health condition before hospitalization after 3 months of follow-up.40,41
A recent study in Brazil focusing on people who had never had COVID-1942 showed that the changes in society and economy imposed by the COVID-19 epidemic may have been responsible for the decline in health-related quality of life and mental well-being. Non-diseased individuals in Chinese population research rated anxiety and depression the lowest on the quality-of-life scale.43,44 One study that looked at the effects of lockdown on psychological health in high-risk populations in France found a correlation between joblessness and increased levels of emotional distress.45
Our results further suggest the possibility that social characteristics may well have played a role since we found that the female sex was a strong and independent predictor of poor health-related life quality during the post-COVID-19 era. Global data show that the COVID-19 pandemic has disproportionately negatively affected women’s mental health,46 even if they have not been infected with COVID-19.10,47,48 Our study highlights the involvement of the disease itself, maybe in addition to numerous social and economic factors that exacerbate its burden, since there was a clear correlation between the intensity of the acute event of COVID-19 and HRQoL during the post-COVID-19 era.
Implications of the Study
The findings of this study also emphasized the importance of getting adequate mental health treatment during the post-COVID-19 era. Authorities and healthcare authorities must give the general public objective, up-to-date, precise, yet simple, adequate guidance about the disease’s progression, security precautions for themselves and others, and activities and steps good.49,50 These results offer information to health officials and policymakers that may be used to create strategic methods for dealing with future epidemics and reassure people that all is well.
Limitations
There are many limitations for this study. Firstly, sample flaws that may have an impact on the overall outcome while performing online surveys. A survey relies on a representative sample to help the author generalize the findings to a wider population. However, there are a number of sample difficulties that might undermine the efficacy of internet-based surveys and generalizability. Secondly, using cross-sectional study. In contrast to longitudinal studies, cross-sectional studies make it harder to identify cause-and-effect linkages.
Conclusion
The HRQoL of COVID-19 patients was significantly impacted, independent of the period since hospitalization or rehabilitation. Policymakers and health workers should research strong ways to enhance the HRQoL of COVID-19 patients as soon as possible. Older patients and those who were infected more than once and those who got hospitalized have a greater probability of decreased HRQoL after infection. Health practitioners should take extra measures to enhance their health-related quality of life following the illness. Females, especially, should be given special treatment upon recovery since they are more prone to experience poor HRQoL. Society healthcare programs, at least in virtual form, are advised to enhance the HRQoL of COVID-19 patients. The overall health of the population and predictors should be considered while designing the health program.
Funding
This study was supported by a grant (MPH/01/14/2021) from the Scientific Research Funds, Ministry of Higher Education and Scientific Research, Amman, Jordan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nandasena H, Pathirathna M, Atapattu A, Prasanga P. Quality of life of COVID 19 patients after discharge: systematic review. PLoS One. 2022;17(2):e0263941. doi:10.1371/journal.pone.0263941
2. Malik P, Patel K, Pinto C, et al. Post‐acute COVID‐19 syndrome (PCS) and health‐related quality of life (HRQoL)—a systematic review and meta‐analysis. J Med Virol. 2022;94(1):253–262. doi:10.1002/jmv.27309
3. Stenman U, Hakama M, Knekt P, et al. Measurement and modeling of health-related quality of life. Epidem Demog Public Health. 2010;195(1):130–135.
4. Abuhammad S, Khabour OF, Alomari MA, Alzoubi KH. Depression, stress, anxiety among Jordanian people during COVID-19 pandemic: a survey-based study. Inform Med Unlocked. 2022;30:100936. doi:10.1016/j.imu.2022.100936
5. AlAzzam M, Abuhammad S, Tawalbeh L, Dalky H. Prevalence and correlates of depression, anxiety, and suicidality among high school students: a national study. J Psychosoc Nurs Ment Health Serv. 2021;59(8):43–51. doi:10.3928/02793695-20210426-02
6. Abuhammad AK, Khabour OF, Hamaideh S, Khasawneh B, Khasawneh B. Sleep quality and sleep patterns among recovered individuals during post-COVID-19 among Jordanian: a cross-sectional national study. Medecine. 2023;102:e32737. doi:10.1097/MD.0000000000032737
7. Abuhammad S, Khabour O, Alzoubi K, et al. Mental health of COVID-19 recovered individuals: a national study from Jordan. Electron J Gen Med. 2023;20(2):em451. doi:10.29333/ejgm/12833
8. Abuhammad S. Violence against Jordanian women during COVID‐19 outbreak. Int J Clin Pract. 2021;75(3):e13824. doi:10.1111/ijcp.13824
9. Abuhammad S, Khabour OF, Alzoubi KH, El-Zubi F, Hamaieh SH. Respiratory infectious diseases and adherence to nonpharmacological interventions for overcoming COVID-19 pandemic: a self-reported study. Int J Clin Pract. 2022;2022:154.
10. AlAzzam M, Abuhammad S, Abdalrahim A, Hamdan-Mansour AM. Predictors of depression and anxiety among senior high school students during COVID-19 pandemic: the context of home quarantine and online education. J School Nurs. 2021;37(4):241–248. doi:10.1177/1059840520988548
11. El Sayed S, Gomaa S, Shokry D, Kabil A, Eissa A. Sleep in post-COVID-19 recovery period and its impact on different domains of quality of life. Egypt J Neurol Psychiatr Neurosurg. 2021;57:1–10. doi:10.1186/s41983-021-00429-7
12. Qamar MA, Martins RS, Dhillon RA, et al. Residual symptoms and the quality of life in individuals recovered from COVID-19 infection: a survey from Pakistan. Ann Med Surg. 2022;75:103361. doi:10.1016/j.amsu.2022.103361
13. Garrigues E, Janvier P, Kherabi Y, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81(6):e4–e6. doi:10.1016/j.jinf.2020.08.029
14. Jacobs LG, Gourna Paleoudis E, Lesky-di bari D, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15(12):e0243882. doi:10.1371/journal.pone.0243882
15. Figueiredo EAB, Silva WT, Tsopanoglou SP, et al. The health-related quality of life in patients with post-COVID-19 after hospitalization: a systematic review. Rev Soc Bras Med Trop. 2022;55. doi:10.1590/0037-8682-0741-2021
16. Vlake JH, Wesselius S, Van Genderen ME, van Bommel J, Boxma-de Klerk B, Wils E-J. Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: a single-center, observational study. PLoS One. 2021;16(8):e0255774. doi:10.1371/journal.pone.0255774
17. Santus P, Tursi F, Croce G, et al. Changes in quality of life and dyspnoea after hospitalization in COVID-19 patients discharged at home. Multidiscip Respir Med. 2020;15(1). doi:10.4081/mrm.2020.713
18. Meys R, Delbressine JM, Goërtz YM, et al. Generic and respiratory-specific quality of life in non-hospitalized patients with COVID-19. J Clin Med. 2020;9(12):3993. doi:10.3390/jcm9123993
19. Rosa RG, Robinson CC, Veiga VC, et al. Quality of life and long-term outcomes after hospitalization for COVID-19: protocol for a prospective cohort study (Coalition VII). Revista Brasileira de Terapia Intensiva. 2021;33:31–37. doi:10.5935/0103-507X.20210003
20. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):1–12. doi:10.1038/s41598-021-95565-8
21. McFann K, Baxter BA, LaVergne SM, et al. Quality of Life (QoL) is reduced in those with severe COVID-19 disease, post-acute sequelae of COVID-19, and hospitalization in United States adults from Northern Colorado. Int J Environ Res Public Health. 2021;18(21):11048. doi:10.3390/ijerph182111048
22. Sandmann FG, Tessier E, Lacy J, et al. Long-term health-related quality of life in non-hospitalized coronavirus disease 2019 (COVID-19) cases with confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in England: longitudinal analysis and cross-sectional comparison with controls. Clin Infect Dis. 2022;75(1):e962–e73. doi:10.1093/cid/ciac151
23. Chatys-Bogacka Z, Mazurkiewicz I, Slowik J, et al. Brain fog and quality of life at work in non-hospitalized patients after COVID-19. Int J Environ Res Public Health. 2022;19(19):12816. doi:10.3390/ijerph191912816
24. Capin JJ, Wilson MP, Hare K, et al. Prospective telehealth analysis of functional performance, frailty, quality of life, and mental health after COVID-19 hospitalization. BMC Geriatr. 2022;22(1):251. doi:10.1186/s12877-022-02854-6
25. Covino M, Russo A, Salini S, et al. Long-term effects of hospitalization for COVID-19 on frailty and quality of life in older adults≥ 80 years. J Clin Med. 2022;11(19):5787. doi:10.3390/jcm11195787
26. Taboada M, Moreno E, Cariñena A, et al. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. Br J Anaesth. 2021;126(3):e110–e3. doi:10.1016/j.bja.2020.12.007
27. Méndez R, Balanzá‐Martínez V, Luperdi SC, et al. Short‐term neuropsychiatric outcomes and quality of life in COVID‐19 survivors. J Intern Med. 2021;290(3):621–631. doi:10.1111/joim.13262
28. Prescott HC. Outcomes for patients following hospitalization for COVID-19. JAMA. 2021;325(15):1511–1512. doi:10.1001/jama.2021.3430
29. de Oliveira Almeida K, Nogueira Alves IG, de Queiroz RS, et al. A systematic review on physical function, activities of daily living and health-related quality of life in COVID-19 survivors. Chronic Illn. 2022;19:17423953221089309.
30. Pizarro-Pennarolli C, Sánchez-Rojas C, Torres-Castro R, et al. Assessment of activities of daily living in patients post COVID-19: a systematic review. PeerJ. 2021;9:e11026. doi:10.7717/peerj.11026
31. Sotoodeh Ghorbani S, Taherpour N, Bayat S, Ghajari H, Mohseni P, Hashemi Nazari SS. Epidemiologic characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID‐19: a systematic review and meta‐analysis. J Med Virol. 2022;94(1):44–53. doi:10.1002/jmv.27281
32. Maruish ME. Assessment of health status and health-related quality of life. In: Handbook of Psychological Assessment in Primary Care Settings. Routledge; 2017:529–564.
33. Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325(3):304–306. doi:10.1001/jama.2020.21465
34. Belli S, Balbi B, Prince I, et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived hospitalisation. Eur Respir J. 2020;56(4):2002096. doi:10.1183/13993003.02096-2020
35. Clemente-Suárez VJ, Beltrán-Velasco AI, Ramos-Campo DJ, et al. Physical activity and COVID-19. The basis for an efficient intervention in times of COVID-19 pandemic. Physiol Behav. 2022;244:113667. doi:10.1016/j.physbeh.2021.113667
36. Guo L, Lin J, Ying W, et al. Correlation study of short-term mental health in patients discharged after coronavirus disease 2019 (COVID-19) infection without comorbidities: a prospective study. In Neuropsychiatric Disease and Treatment. Taylor and Francis; 2020:2661–2667.
37. Dorri M, Bazargany MHM, Khodaparast Z, et al. Psychological problems and reduced health-related quality of life in the COVID-19 survivors. J Affect Disorders Rep. 2021;6:100248. doi:10.1016/j.jadr.2021.100248
38. Gamberini L, Mazzoli CA, Sintonen H, et al. Quality of life of COVID-19 critically ill survivors after ICU discharge: 90 days follow-up. Qual Life Res. 2021;30:2805–2817. doi:10.1007/s11136-021-02865-7
39. Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect. 2020;11(5):296. doi:10.24171/j.phrp.2020.11.5.05
40. Bryson WJ. Long-term health-related quality of life concerns related to the COVID-19 pandemic: a call to action. Qual Life Res. 2021;30(3):643–645. doi:10.1007/s11136-020-02677-1
41. Aljuaid M, Ilyas N, Altuwaijri E, et al. Quality of life among caregivers of patients diagnosed with major chronic disease during COVID-19 in Saudi Arabia. In: Healthcare. MDPI; 2022.
42. Vitorino LM, Júnior GHY, Gonzaga G, et al. Factors associated with mental health and quality of life during the COVID-19 pandemic in Brazil. BJ Psych Open. 2021;7(3):e103. doi:10.1192/bjo.2021.62
43. Ping W, Zheng J, Niu X, et al. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One. 2020;15(6):e0234850. doi:10.1371/journal.pone.0234850
44. Ferreira LN, Pereira LN, da Fé Brás M, Ilchuk K. Quality of life under the COVID-19 quarantine. Qual Life Res. 2021;30:1389–1405. doi:10.1007/s11136-020-02724-x
45. Valent A, Dudoignon E, Ressaire Q, Dépret F, Plaud B. Three-month quality of life in survivors of ARDS due to COVID-19: a preliminary report from a French academic centre. Anaesthes Crit Care Pain Med. 2020;39(6):740–741. doi:10.1016/j.accpm.2020.10.001
46. Abuhammad S, Alzoubi KH, Al-Azzam SI, Karasneh RA. Knowledge and practice of patients’ data sharing and confidentiality among nurses in Jordan. J Multidiscip Healthc. 2020;13:935. doi:10.2147/JMDH.S269511
47. Chen K-Y, Li T, Gong F-H, Zhang J-S, Li X-K. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psychiatry. 2020;11:668. doi:10.3389/fpsyt.2020.00668
48. Hung MSY, Lam SKK, Chan LCK, Liu SPS, Chow MCM. The psychological and quality of life impacts on women in Hong Kong during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(13):6734. doi:10.3390/ijerph18136734
49. Karasneh R, Al-Mistarehi A-H, Al-Azzam S, et al. Physicians’ knowledge, perceptions, and attitudes related to patient confidentiality and data sharing. Int J Gen Med. 2021;721–731. doi:10.2147/IJGM.S301800
50. Abuhammad S. Preparing for future pandemics: challenges for healthcare leadership. J Healthc Leadersh. 2022;14:131–136. doi:10.2147/JHL.S363650
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
