Back to Journals » Transplant Research and Risk Management » Volume 9
Hand transplantation: current challenges and future prospects
Authors Alolabi N, Augustine H, Thoma A
Received 12 July 2016
Accepted for publication 27 September 2016
Published 21 February 2017 Volume 2017:9 Pages 23—29
DOI https://doi.org/10.2147/TRRM.S94298
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qing Yi
Noor Alolabi,1 Haley Augustine,1 Achilles Thoma1–3
1Division of Plastic Surgery, Department of Surgery, 2Surgical Outcomes Research Centre, 3Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, ON, Canada
Abstract: Over the last two decades, 113 vascularized composite allotransplantation (VCA) of the hand have been performed in 76 patients globally. The procedure that was once regarded as experimental has certainly emerged as a clinical reality with multiple centers worldwide now performing it. The psychological and physical impact of losing an upper extremity is profound. Amputees face significant challenges contributing to disability and dependence even with activities of daily living. Hand transplantation offers functions with restoring sensation, voluntary motor control, and proprioception, as well as a sense of feeling “whole” again. Along with these benefits, however, transplantation carries a significant risk profile attributed to the complications of life-long immunosuppression and possible rejection. Moreover, the procedure carries a significant financial burden to the health care system. As hand VCA is becoming more widely accepted and performed worldwide, there are still many challenges that will face its rapid growth. This review highlights some of the challenges facing hand VCA including patient selection, effect on quality of life, financial burden, functional outcomes, and complications of immunosuppression.
Keywords: hand transplantation, vascularized composite allotransplantation
A Letter to the Editor has been received and published for this article.
Introduction
The first attempted hand transplantation was performed in Ecuador in 1964. The transplant survived 2 weeks but was lost to acute rejection.1 Over the next three decades, surgical advancements in replantation microsurgery as well as medical advancements in transplant immunology and immunosuppressive therapy allowed for the success of such a procedure.2 In 1998, the second hand transplant was performed in Lyon, France. The patient ultimately lost the transplant after 2 years because of rejection secondary to medication noncompliance.3,4 Following this, the first successful hand transplant with long-term survivability was performed in Louisville, Kentucky, in 1999.5 The patient remains the longest surviving hand transplant recipient, 17 years since transplantation.
Subsequent to this success, hand transplantation has evolved from what used to be regarded as experimental and potentially unethical to a procedure that is accepted and recognized, with 113 transplants performed on 76 patients worldwide.6–17 Though it offers sensation, function, cosmetic, and psychological benefits, there are significant risks associated with the lifelong immunosuppressive medication required with transplantation.4,5,7,12,18–34 This article aims to outline the challenges of hand transplantation by discussing patient selection, effect on quality of life, financial burden, functional outcomes, and risks of immunosuppression.
Incidence, etiology, and alternative treatment
Upper extremity amputation in young patients is typically the result of trauma, infection, or is secondary to congenital anomalies. For older patients, amputation is more likely a result of medications or peripheral vascular diseases. The incidence of upper extremity loss is variable in the literature, though it is estimated to be 11.6 in 100,000 adults.35
The psychological and physical impact of losing an upper extremity is profound. Such a loss results in significant disability, with severe impact on quality of life. The mainstay of treatment for hand amputation has been prosthesis. Various forms of prostheses are available and range from a nonfunctional cosmetic prosthetic, to a hook, to a more advanced myoelectric prosthetic. Though a prosthetic may provide an assisting hand, it is limited by the burden of weight, discomfort, limited usefulness, and lack of functional feedback. Additionally, bilateral amputees face unique challenges with basic grooming, self-care, and activities of daily living contributing to significant disability and dependence.36
As a form of vascularized composite allotransplantation (VCA), hand transplantation can functionally offer a far superior option than prostheses. It provides superior dexterity with restoring sensibility, intrinsic muscle function, and proprioception. Moreover, it can potentially provide a match in color, size, and overall appearance. However, these benefits could be outweighed by the complications secondary to the life-long immunosuppression required.6–7
Patient selection
Eligibility and indication for hand transplantation remain to be a challenge and topic of debate. Generally speaking, indications for transplant are based on both the expected preoperative success of transplant and the impact on function for the patient. Indications may include amputation of the dominant hand, bilateral amputations, distal amputations (less nerve regeneration required), and abrupt amputations with clean end points of distal stump.37,38 Table 1 outlines the inclusion and exclusion criteria used by several USA hand transplant centers.39
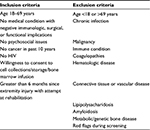  | Table 1 Inclusion and exclusion criteria for hand transplant recipients used by several USA hand transplant centers Note: Reproduced from MacKay BJ, Nacke E, Posner M. Hand transplantation: a review. Bull Hosp Jt Dis. 2014;72(1):76–88. With permission.39 |
An assessment of the whole person is required to determine eligibility. This involves a multidisciplinary team to properly evaluate the possible medical, psychological, and social impacts of one’s amputation as well as to determine their potential for success and improved outcomes with transplant. Centers that contemplate performing hand VCA must have the capacity for a multidisciplinary team such as the one listed in Table 2.
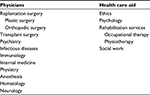  | Table 2 Sample multidisciplinary team required for a hand transplant center |
Predictors of non-adherence to immunosuppressive medication regimens include inadequate social support, higher education, and less conscientiousness.40 Patient selection and education are crucial as intensive daily hand therapy and significant morbidity are associated with immunosuppression.27,41 Once selection is determined, it is paramount to explore patients’ expectations as well as educate them on the nature of the intense recovery.
Effectiveness of hand VCA
Performing high-quality studies such as a randomized controlled trial to investigate the difference in outcomes between hand VCA and, for example, prosthesis application is not possible because of feasibility issues, ethical issues, costs, and patient recruitment. This poses a significant challenge when attempting to widely implement a new intervention since little outcome data are available. However, when clinical trials cannot be performed, well-done observational studies and decision analyses are regarded as an acceptable method to help decide among different treatment options.42,43
Four decision analysis studies have been published,44–47 evaluating the effectiveness of hand transplantation. The studies used differing methodology, populations, and assumptions in their decision analyses. Overall, bilateral hand transplantation showed improvement in health utility or at least showed an increased risk acceptance profile, whereas unilateral hand transplantation was not justified. These studies highlighted the significant impact that immunosuppressive side effects play on the overall utility of the procedure.
Financial burden
Another challenge with implementing such a resource-heavy treatment option is the financial burden on the health care system. The direct and indirect costs associated with hand transplantation include surgical costs, days in hospital, immunosuppression treatment and complications, rehabilitation, and the opportunity cost of days off work.
Chung et al46 performed an economic cost-utility analysis of hand transplantation in the United States using 100 medical students and showed that the mean surgical costs were $13,796 for single and $14,608 for bilateral hand transplants. This included preoperative assessments, hospitalization, and physician fees. Estimates for immunosuppressive therapy were $433,282 for 40 years of treatment. Overall, a lifetime cost for hand VCA was $528,000–$530,000 (single or bilateral) versus single and bilateral prosthesis at $20,000 and $41,000, respectively. The cost of productivity loss for hand transplantation was $42,265 and prosthetic adaptation was $9,753.
Moreover, the estimated rehabilitation cost for a single hand transplant in one study was calculated to be $53,336 for 226 hours of therapy and $63,360 for 260 hours of therapy for a bilateral transplant.39 Based on the limited evidence available, hand transplantation has shown to be significantly more costly than prosthesis and exceeds the predetermined threshold in cost-effectiveness analysis and therefore it is not cost-effective for a single hand transplant.39,46 So far, the cost for most hand transplants has been covered by insurance companies, government grants, the ministry of defense, or individual hospitals. If this procedure was to become the standard of care for the treatment of a hand amputation, the economic impact would be very significant.
Outcomes
Shores et el48 published on the outcomes of hand and upper extremity transplantation in the worldwide experience in 2016. This report included 72 patients with 107 total unilateral or bilateral upper limb transplants. With regard to mortality, 4 patients have died; 2 patients had combined hand and leg transplants; and 1 had combined hand and face transplants. The patient survival rate for unilateral or bilateral hand transplantation in isolation is 98.5%. A total of 24 limbs have been lost because of patient death (4 patients, 8 limbs), acute loss (3 patients, 5 limbs), and chronic limb loss (11 patients, 11 limbs). Transplants performed in China, however, have had issues with noncompliance or lack of access to immunosuppression resulting in 58% graft loss in their experience. When disregarding the Chinese group and the multisite heterogeneous transplants group, hand transplantation in Western Europe/Australia/US experience have had successful results with a mortality rate of 0% in 50 patients and a graft survival rate of 90.5% (7 of 74 limbs lost). Table 3 provides a summary of known hand and upper extremity transplants before 2016 as published by Shores et al.48 Since then, six transplants have been performed, two at the University of Pennsylvania, one at the University of Louisville, two in India, and one in Canada. Certainly, this list may not be fully complete as there may be other unknown or unpublished hand transplantation data.
  | Table 3 Summary of the known hand and upper extremity transplantations worldwide48 Note: *Simultaneous hand and other body region transplantation (face or leg). Reproduced from Shores JT, Brandacher G, Lee WP. Hand and upper extremity transplantation: an update of outcomes in the worldwide experience. Plast Reconstr Surg. 2015;135(2):351e–360e. http://journals.lww.com/plasreconsurg/pages/articleviewer.aspx?year=2015&issue=02000&article=00035&type=abstract.48 |
The patient population in hand transplantation is extremely heterogeneous with respect to anatomy, function, rehabilitation, and goals. For these reasons, evaluating and predicting outcomes for patients have proven to be a difficult task. In an attempt to address this issue, the International Registry on Hand and Composite Tissue Transplantation (IRHCTT) was developed as a means of collecting and synthesizing data on outcomes in a centralized and accessible manner. The registry has collected prospective data on transplant patients since 2002.7 The last report,6 published in 2011, includes 39 patients who underwent 57 hand transplants. With regard to immunosuppressive complications, a majority (90%) of patients had metabolic complications (hyperglycemia, end-stage renal disease, Cushing syndrome, hyperparathyroidism), and 77% of patients suffered from opportunistic infections at some point during follow-up. Other less common complications included hypertension, serum sickness, avascular necrosis of the hip, and skin cancer.
Evaluation of functional outcomes demonstrated that all patients developed protective sensation. Tactile sensibility was present in 90% of patients, and discriminative sensibility was present in 82%. Patients recovered sufficient motor function to perform most activities of daily living, including eating, driving, grooming, and writing. DASH scores averaged 38 at 1 year and 16 at 10 years post transplant (0 being the best possible score). Greater than 75% of patients had improved quality of life and the majority had returned to some manner of occupation.7,48,49
Immunosuppression
Perhaps the biggest challenge and impediment to hand transplantation growth is justifying the negative effects of life-long immunosuppression for a non-life-threatening condition. The compilation of foreign skin, muscle, nerve, tendon, and bone in VCA makes it exceedingly more challenging to avoid rejection than in solid organ transplantation. Specifically, skin has the tendency to be extremely antigenic requiring more aggressive immunosuppression.50 Chronic immunosuppression has profound short- and long-term side effects predisposing patients to opportunistic infections, cancer, endocrinopathies such as diabetes and dyslipidemia, as well as end-organ damage, including nephrotoxicity and neurotoxicity.51 These profound effects along with the expensive price of medications contribute significantly to the poor compliance of patients to their medication regimes.
Typically, a patient preparing for transplant will undergo several cycles of induction therapy to diminish the initial acute immune response, followed by a triple-drug therapy protocol once transplantation has taken place for long-term immunosuppression.52–56
Induction agents work to deplete the T- and B-cell stores or interfere with the adaptive immune response at the time of alloantigen presentation with transplantation. Induction consists of a polyclonal or monoclonal antibody against thymocytes such as thymoglobulin and alemtuzumab.52–56 This approach has reduced the need for long-term steroid use and the associated cardiovascular risk factors.57
Once transplantation has taken place, maintenance therapy begins with triple-drug therapy. Triple-drug regimens include a calcineurin inhibitor to prevent early activation of T cells (e.g., tacrolimus), an antimetabolite agent to prevent synthesis of nucleotides required in lymphocyte proliferation (e.g., mycophenolate mofetil), and a steroid (e.g., prednisone). Triple-drug therapy is guided by protocols developed for solid organ transplantation.57,58 Doses and treatment regimens in VCA most resemble those used in renal transplant.58 A balance is achieved by preventing graft rejection while avoiding some immunity to prevent sepsis, end-organ damage, and neoplasia.
Newer regimens to decrease the risks of immunosuppression are currently being researched heavily. Specifically, protocols are now attempting to avoid the use of steroids and replacing tacrolimus with sirolimus. Steroids have significant cardiovascular side effects, resulting in nearly half transplant loss related to cardiovascular and infectious complications. Long-term use of tacrolimus results in nephrotoxicity, diabetes, hypertension, infection, and neoplasia.58 However, it also has been shown to facilitate nerve regeneration and therefore has some benefit in VCA of the hand. This effect is applied to nerve transection with primary repair as well as grafts.59–61 In an attempt to decrease systemic immunosuppression and focus on the antigenic nature of skin, topical steroids and tacrolimus have also been trialed.7
Moreover, novel approaches have been applied to adapt the immune system to tolerate the coexistence of donor and recipient immune cells through chimerism.62,63 Donor bone marrow cells are infused into the recipient during induction therapy to develop tolerance of donor antigens.64–68 Tolerance may be sufficiently achieved by only a few (1%) circulating donor lymphocytes. This area of research has been developed at the University of Pittsburgh, and early results suggest decreased immunosuppressive requirements with successful graft take.69
Data from the IRHCTT show that 85% of hand transplant recipients experience one or more episodes of acute rejection.6 The clinical presentation includes erythematous maculopapular rash, hair loss, and desquamation. Close monitoring of skin changes is important to ensure there are no early signs of rejection. Similar to solid organ transplantation, acute rejection that is biopsied may show lymphocytic infiltrate. Chronic rejection is not well visualized histologically, but it is thought to cause intimal hyperplasia.7
Ideal hand VCA unit
Successful hand VCA relies on the collaboration, financial support, and commitment by health care workers and the patient. The ideal hand VCA center would be established in an academic center where a solid organ transplant unit already exists. This is important since many of the ethical implications hopefully would have been addressed with the assistance of an ethicist and the details in transplant planning are already established. Supportive administration facilitates the coordination and open communication of all services involved. The necessary lifelong immunosuppressive drugs are extraordinarily expensive for patients. Therefore, a commitment to drug coverage by the institution needs to be established to minimize this barrier and the catastrophic complication of rejection. Moreover, multiple disciplines are required for the success of such a procedure, and collaboration between all teams is crucial. The surgical team for the transplant should include both orthopedic and plastic surgeons. Other perioperative disciplines involved include immunology, psychiatry, infectious diseases, internal medicine, physiatry, dermatology, neurology, hematology, and anesthesia. Successful VCA hand transplant is dependent on the postoperative rehabilitation. Therefore, an on-site occupational therapist and physiotherapist are important to streamline this essential therapy. Lastly, the center should have adequate psychological and social support for patients as this surgery carries great psychosocial impact.
Summary
Hand transplantation is an emerging field in plastic, orthopedic, and transplant surgery that has become increasingly more popular and common in the last decade. The improvement in function and quality of life it offers is heavily recognized. The once considered “experimental” procedure is no longer the case. However, a newer debate of whether this procedure should be the standard of care for hand amputees is becoming popularized. This review highlights some of the challenges that hand transplantation faces including patient selection, effect on quality of life, financial burden, functional outcomes, and immunosuppressive complications. Before hand VCA becomes as widely accepted as solid organ transplantation has, these factors all need to be carefully studied and analyzed heavily. Hand transplantation in the appropriate candidate and settings may be a very suitable treatment option. Nevertheless, the sparse long-term data available, especially with respect to the immunosuppressive complications, still pose a significant barrier.
Disclosure
The authors report no conflicts of interest in this work.
References
Gilbert R. Transplant is successful with a cadaver forearm. Med Trib Med News. 1964;5:20–23. | ||
Errico M, Metcalfe NH, Platt A. History and ethics of hand transplants. JRSM Short Rep. 2012;3(10):74. | ||
Dubernard JM, Owen E, Lefranois N, et al. First human hand transplantation. Case report. Transpl Int. 2000;13:S521–S524. | ||
Dubernard JM, Owen E, Herzberg G, et al. Human hand allograft: report on first 6 months. Lancet. 1999;353:1315–1320. | ||
Jones JW, Gruber SA, Barker JH, Breidenbach WC. Successful hand transplantation. One year follow-up. Louisville hand transplant team. N Engl J Med. 2000;343:468–473. | ||
Petruzzo P, Dubernard JM. The International Registry on Hand and Composite Tissue allotransplantation. Clin Transpl. 2011:247–253. | ||
Petruzzo P, Lanzetta M, Dubernard JM, et al. The International Registry on Hand and Composite Tissue Transplantation. Transplantation. 2010;90:1590–1594. | ||
Cavadas PC, Landin L, Thione A, et al. The Spanish experience with hand, forearm, and arm transplantation. Hand Clin. 2011;27:443–453, viii. | ||
Hautz T, Engelhardt TO, Weissenbacher A, et al. World experience after more than a decade of clinical hand transplantation: update on the Innsbruck program. Hand Clin. 2011;27:423–431, viii. | ||
Jabłecki J. World experience after more than a decade of clinical hand transplantation: update on the Polish program. Hand Clin. 2011;27:433–442, viii. | ||
Kaufman CL, Breidenbach W. World experience after more than a decade of clinical hand transplantation: update from the Louisville hand transplant program. Hand Clin. 2011;27:417–421, vii–viii. | ||
Lanzetta M, Petruzzo P, Dubernard JM, et al. Second report (1998–2006) of the International Registry of Hand and Composite Tissue Transplantation. Transpl Immunol. 2007;18:1–6. | ||
Ninkovic M, Weissenbacher A, Gabl M, et al. Functional outcome after hand and forearm transplantation: what can be achieved? Hand Clin. 2011;27:455–465, viii–ix. | ||
Pei G, Xiang D, Gu L, et al. A report of 15 hand allotransplantations in 12 patients and their outcomes in China. Transplantation. 2012;94:1052–1059. | ||
Petruzzo P, Dubernard JM. World experience after more than a decade of clinical hand transplantation: update on the French program. Hand Clin. 2011;27:411–416, vii. | ||
Petruzzo P, Kanitakis J, Badet L, et al. Long-term follow-up in composite tissue allotransplantation: in-depth study of five (hand and face) recipients. Am J Transplant. 2011;11:808–816. | ||
Breidenbach WC, Meister EA, Turker T, et al. A methodology for determining standard of care status for a new surgical procedure: hand transplantation. Plast Reconstr Surg. 2016;137(1):367–373. | ||
Breidenbach WC, Gonzales NR, Kaufman CL, KlaphekeM, Tobin GR, Gorantla VS. Outcomes of the first 2 American hand transplants at 8 and 6 years posttransplant. J Hand Surg Am. 2008;33(7):1039–1047. | ||
Dubernard JM, Petruzzo P, Lanzetta M, et al. Functional results of the first human double-hand transplantation. Ann Surg. 2003;238(1):128–136. | ||
Francois CG, Breidenbach WC, Maldonado C, et al. Hand transplantation: comparisons and observations of the first four clinical cases. Microsurgery. 2000;20(8):360–371. | ||
Lanzetta M, Nolli R, Borgonovo A, et al. Hand transplantation: ethics, immunosuppression and indications. J Hand Surg Br. 2001;26(6):511–516. | ||
Lanzetta M, Petruzzo P, Margreiter R, et al. The International Registry on Hand and Composite Tissue Transplantation. Transplantation. 2005;79(9):1210–1214. | ||
Margreiter R, Brandacher G, Ninkovic M, Steurer W, Kreczy A, Schneeberger S. A double hand transplant can be worth the effort! Transplantation. 2002;74(1):85–90. | ||
Petruzzo P, Lanzetta M, Dubernard JM, et al. The International Registry on Hand and Composite Tissue Transplantation. Transplantation. 2008;86(4):487–492. | ||
Petruzzo P, Revillard JP, Kanitakis J, et al. First human double hand transplantation: efficacy of a conventional immunosuppressive protocol. Clin Transplant. 2003;17(5):455–460. | ||
Piza-Katzer H, Ninkovic M, Pechlaner S, Gabl M, Ninkovic M, Hussl H. Double hand transplantation: functional outcome after 18 months. J Hand Surg Br. 2002;27:385–390. | ||
Ravindra KV, Buell JF, Kaufman CL, et al. Hand transplantation in the United States: experience with 3 patients. Surgery. 2008;144(4):638–643. | ||
Klapheke MM. Transplantation of the human hand: psychiatric implications. Bull Menninger Clin. 1999;63:159–173. | ||
Cooney WP, Hentz VR. American Society for Surgery of the Hand. Hand transplantation – primum non nocere. J Hand Surg Am. 2002;27:165–168. | ||
Foucher G. Prospects for hand transplantation. Lancet. 1999;353(1961):1286–1287. | ||
Gorantla V, Maldonado C, Frank J, Barker JH. Composite tissue allotransplantation (CTA): current status and future insights. Eur J Trauma. 2001;27:267–274. | ||
Hettiaratchy S, Butler PE, Lee WP. Lessons from hand transplantations. Lancet. 2001;357(9255):494–495. | ||
Jones NF. Concerns about human hand transplantation in the 21st century. J Hand Surg Am. 2002;27(5):771–787. | ||
Lee WP. Composite tissue transplantation: more science and patience needed. Plast Reconstr Surg. 2001;107(4):1066–1070. | ||
Østlie K, Skjeldal OH, Garfelt B, Magnus P. Adult acquired major upper limb amputation in Norway: prevalence, demographic features and amputation specific features. A population-based survey. Disabil Rehabil. 2011;33(17–18):1636–1649. | ||
Grob M, Papadopulos NA, Zimmerman A, et al. The psychological impact of severe hand injury. J Hand Surg Eur. 2008;33:358–362. | ||
Boulas HJ. Amputations of the fingers and hand: indications for replantation. J Am Acad Orthop Surg. 1998;6(2):100–105. | ||
Hartzell TL, Benhaim P, Imbriglia JE, et al. Surgical and technical aspects of hand transplantation: is it just another replant? Hand Clin. 2011;27(4):521–530, x. | ||
Mackay BJ, Nacke E, Posner M. Hand transplantation – a review. Bull Hosp Jt Dis (2013). 2014;72(1):76–88. | ||
Dobbels F, Vanhaecke J, Dupont L, et al. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87(10):1497–1504. | ||
Shores JT. Recipient screening and selection: who is the right candidate for hand transplantation. Hand Clin. 2011;27(4):539–543, x. | ||
Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. 2nd edition. Oxford: Oxford Medical Publications; 1997. | ||
Mastracci TM, Cina CS, Thoma A, Farrokhyar F, Tandan VR; Evidence-Based Surgery Working Group. User’s guide to the surgical literature: how to use a decision analysis. Can J Surg. 2007;50(5):403–409. | ||
McCabe S, Rodocker G, Julliard K, et al. Using decision analysis to aid in the introduction of upper extremity transplantation. Transplant Proc. 1998;30(6):2783–2786. | ||
Majzoub RK, Cunningham M, Grossi F, Maldonado C, Banis JC, Barker JH. Investigation of risk acceptance in hand transplantation. J Hand Surg Am. 2006;31(2):295–302. | ||
Chung KC, Oda T, Saddawi-Konefka D, Shauver MJ. An economic analysis of hand transplantation in the United States. Plast Reconstr Surg. 2010;125(2):589–598. | ||
Alolabi N, Chuback J, Grad S, Thoma A. The utility of hand transplantation in hand amputee patients. J Hand Surg Am. 2015;40:8–14. | ||
Shores JT, Brandacher G, Lee WP. Hand and upper extremity transplantation: an update of outcomes in the worldwide experience. Plast Reconstr Surg. 2015;135(2):351e–360e. | ||
Jensen SE, Butt Z, Bill A, et al. Quality of life considerations in upper limb transplantation: review and future directions. J Hand Surg Am. 2012;37:2126–2135. | ||
Murray JE. Organ transplantation (skin, kidney, heart) and the plastic surgeon. Plast Reconstr Surg. 1971;47:425–431. | ||
Ojo AO, Held PJ, Port FK, et al. Chronic renal failure after transplantation of a nonrenal organ. N Engl J Med. 2003;349:931–940. | ||
Patlola V, Zhong X, Reed GW, Mandelbrot DA. Efficacy of anti-IL-2 receptor antibodies compared to no induction and to antilymphocyte antibodies in renal transplantation. Am J Transplant. 2007;7:1832–1842. | ||
Jindal RM, Das NP, Neff RT, et al. Outcomes in African-Americans vs. Caucasians using thymoglobulin or interleukin-2 receptor inhibitor induction: analysis of USRDS database. Am J Nephrol. 2009;29:501–508. | ||
Willoughby LM, Schnitzler MA, Brennan DC, et al. Early outcomes of thymoglobulin and basiliximab induction in kidney transplantation: application of statistical approaches to reduce bias in observational comparisons. Transplantation. 2009;87:1520–1529. | ||
Shapiro R, Basu A, Tan H, et al. Kidney transplantation under minimal immunosuppression after pre-transplant lymphoid depletion with thymoglobulin or campath. J Am Coll Surg. 2005;200:505–515. | ||
Kaufman DB, Leventhal JR, Axelrod D, Gallon LG, Parker MA, Stuart FP. Alemtuzumab induction and prednisone-free maintenance immunotherapy in kidney transplantation: comparison with basiliximab induction–long-term results. Am J Transplant. 2005;5:2539–2548. | ||
Ravindra KV, Ildstad ST. Immunosuppressive protocols and immunological challenges related to hand transplantation. Hand Clin. 2011;27(4):467–479, ix. | ||
Brandacher G, Gorantla VS, Lee WP. Hand allotransplantation. Semin Plast Surg. 2010;24:11–17. | ||
Yan Y, Sun HH, Hunter DA, Mackinnon SE, Johnson PJ. Efficacy of short-term FK506 administration on accelerating nerve regeneration. Neurorehabil Neural Repair. 2012;26:570–580. | ||
Moore AM, Ray WZ, Chenard KE, et al. Nerve allotransplantation as it pertains to composite tissue transplantation. Hand. 2009;4:239–244. | ||
Mackinnon SE, Doolabh VB, Novak CB, Trulock EP. Clinical outcome following nerve allograft transplantation. Plast Reconstr Surg. 2001;107:1419–1429. | ||
Wu S, Xu H, Ravindra K, Ildstad ST. Composite tissue allotransplantation: past, present and future-the history and expanding applications of CTA as a new frontier in transplantation. Transplant Proc. 2009;41(2):463–465. | ||
Szajerka T, Klimczak A, Jablecki J. Chimerism in hand transplantation. Ann Transplant. 2011;16(1):83–89. | ||
Schneeberger S, Gorantla VS, Brandacher G, et al. Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Ann Surg. 2013;257:345–351. | ||
Starzl TE, Zinkernagel RM. Antigen localization and migration in immunity and tolerance. N Engl J Med. 1998;339:1905–1913. | ||
Starzl TE, Murase N, Abu-Elmagd, et al. Tolerogenic immunosuppression for organ transplantation. Lancet. 2003;361:1502–1510. | ||
Fontes P, Rao S, Demetris AJ, et al. Bone marrow augmentation of donor-cell chimerism in kidney, liver, heart, and pancreas islet transplantation. Lancet. 1994;344:151–155. | ||
Ciancio G, Miller J, Garcia-Morales RO, et al. Six-year clinical effect of donor bone marrow infusions in renal transplant patients. Transplantation. 2001;71:827–835. | ||
Gorantla VS, Brandacher G, Schneeberger S, et al. Favoring the risk-benefit balance for upper extremity transplantation – the Pittsburgh Protocol. Hand Clin. 2011;27(4):511–520, ix–x. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
