Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Gynecological emergency ultrasound in daytime and at night: differences that cannot be ignored
Authors Jin BB , Gong YZ, Ma Y, He ZH
Received 24 March 2018
Accepted for publication 20 April 2018
Published 20 June 2018 Volume 2018:14 Pages 1141—1147
DOI https://doi.org/10.2147/TCRM.S169165
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Bin-Bin Jin,1,* Yi-Zhen Gong,2,* Yan Ma,1 Zhong-Hui He3
1Department of Ultrasonography, 2Department of Evidence-Based Medicine, 3Department of Gynecology, The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, People’s Republic of China
*These authors contributed equally to this work
Background: Ultrasonography, the preferred adjunct examination method and the differential diagnostic tool for gynecologic emergency, can reflect the change pattern of gynecological diseases in daytime and at night. The purpose of this study was to analyze the diseases through gynecological emergency ultrasound in daytime and at night and to evaluate the day–night difference in the accuracy of ultrasound diagnosis.
Materials and methods: Retrospective analysis was performed on the 2016 clinical data of the patients who had undergone gynecological emergency ultrasound at The First Affiliated Hospital of Guangxi Medical University, and the results of the ultrasound diagnosis were compared with the clinical diagnosis.
Results: The following categories of gynecologic emergency diseases during the daytime and at night have significant statistical differences in the constituent ratio (P<0.001); ectopic pregnancy, intrauterine pregnancy, acute pelvic inflammatory disease, no organic lesion in uterine and adnexa; while the constituent ratio of abortion and trophoblastic diseases, ovarian tumor, uterine and endometrial lesions, was no statistical difference during the daytime and at night (P>0.05). The overall coincidence rate of ultrasound diagnosis was 96.3% (daytime, 97.9%; night, 86.4%). The coincidence rates of ectopic pregnancy ultrasonography diagnosis in daytime and at night were 96.4 and 75.4%, respectively; the difference was statistically significant (P<0.001).
Conclusion: Since the different constituent ratio of disease between daytime and night gynecological emergency ultrasound was significantly different, and the diagnostic accuracy of ultrasound at night was low; hence, the ultrasound doctor at night should pay attention to improve the accuracy of diagnosis and the ability of differential diagnosis of ectopic pregnancy, and it is suggested that some suspected cases during the night should be reexamined again in the daytime to eliminate the errors resulted from subjective factors.
Keywords: gynecology, emergency, ultrasound, daytime, night, difference
Introduction
The schedule of most public hospitals follows the rule that doctors working in the day clinic significantly outnumber those working at night, and experienced and senior doctors are mostly arranged in daytime, while the night shift are mainly covered by the younger and junior doctors. Therefore, in order to be treated by the experienced and senior doctors, patients are more likely to go to hospital during the day. But not all patients can choose time of visiting the doctor at will, for example, those who suffer from gynecologic acute abdomen.
Gynecologic acute abdomen, with complicated pathogenesis and condition could be life-threatening; hence, correct diagnosis at the time is the prerequisite for proper treatment. The ultrasonic examination which is noninvasive, simple, and convenient, plays an important role in the clinical diagnosis of gynecological diseases. Sometimes it is the only adjunct to the assessment of acute pelvic pain in women. It can effectively diagnose gynecological diseases caused by acute abdominal pain in women, while exclude other causes without surgical treatment.1 Therefore, it is the preferred adjunct examination method and differential diagnostic tool for gynecologic emergency.
The aims of this study are to investigate the difference of gynecological emergency ultrasound between the day and the night and to evaluate the quantity, quality, and disease constituent ratio, so as to promote doctors and clinicians to work together to reduce human error and improve the diagnostic accuracy.
Materials and methods
Clinical data
This retrospective study was carried out at The First Affiliated Hospital of Guangxi Medical University, which is the largest teaching hospital and tertiary referral center of Guangxi in southern China. Patients in the daily clinic and emergency department exceed 10,000 and cover an ethnically and socially diverse population. All clinicians have >2 years of clinical experience, and the emergency ultrasound doctors on duty have passed the standardized training. This study assessed all patients, who had been first diagnosed by an outpatient or emergency clinic and undergone an emergency gynecologic ultrasound examination, from January 1, 2016, to December 31, 2016. According to the hospital’s schedule, the patients were divided into the daytime group (8 am to 5.59 pm) and the night group (6 pm to 7.59 am next day) based on the ultrasonic examination time. Exclusion criteria were >13 weeks of gestation. All patients provided written informed consent for the use of ultrasound data in subsequent studies. The research was approved by The First Affiliated Hospital of Guangxi Medical University’s Ethical Review Committee.
Instruments and methods
GE E8 and Siemens AS ultrasonic diagnostic apparatus with the abdominal probe frequency of 2–6 MHz and the transvaginal probe frequency of 3–7 MHz was used. The patient who is undergoing abdominal ultrasonography took supine position after properly filling the bladder, and the one who is undergoing transvaginal sonography took lithotomy position after emptying the bladder. The emergency ultrasound doctors on duty who have passed the standardized training conducted transabdominal and/or transvaginal multisection ultrasound scanning to observe the shape, the size, and the internal echo of the uterus, abnormalities around the uterus, free effusion in pelvic cavity and abdominal cavity, and color blood flow signal.
According to the results of the clinical diagnosis combined with the characteristics of ultrasonic diagnosis, we used previous studies2–6 to develop a classification and divided the gynecologic emergency diseases into the following seven categories: 1) ectopic pregnancy, in which extrauterine mass can be found by ultrasound and was clinically diagnosed as tubal pregnancy, abdominal pregnancy, ovarian pregnancy, cervical pregnancy, scar pregnancy, and intramural pregnancy; 2) intrauterine pregnancy, in which developing gestational sac can be found in uterine cavity by ultrasound; 3) abortion and trophoblastic diseases, which include inevitable abortion, complete abortion, incomplete abortion, missed abortion, hydatidiform mole, invasive hydatidiform mole, and chorioepithelioma; 4) acute pelvic inflammatory disease; 5) Ovarian tumor: benign or malignant tumor; 6) uterine and endometrial lesions, which include uterine fibroids, adenomyosis, endometrial polyps, endometrial hyperplasia, malignant tumors of the uterus and so on; and 7) no organic lesion in uterine and adnexa, which includes no organic lesion in uterine and adnexa by ultrasonic diagnosis but clinically diagnosed as primary dysmenorrhea, functional uterine bleeding, residual or malposition of the intra uterine device, perineal trauma, or other nongynecological diseases such as appendicitis, cholecystitis, and urinary calculi.
Result tracking
The following are valid tracking: 1) for surgical patients, accessing reliable pathological diagnosis; 2) for hospitalized patients without surgery, consulting the medical records, determining symptoms, signs, and treatment process, observing the results of other auxiliary examinations such as blood biochemistry examination, radiological examination, and aspiration biopsy examination, or eventually accessing the reliable clinical diagnosis through repeated examination of ultrasound; 3) for nonoperated nor hospitalized patients, eventually confirming the clinical diagnosis by keeping follow-ups and checking the blood biochemical indexes and ultrasound regularly in the hospital.
The following are deemed as invalid tracking: 1) those who cannot be contacted by phone and address; 2) those who refuse to undergo another examination or treatment; and 3) the results of the current examination cannot be used to make clear diagnosis.
Statistical analyses
The SPSS Version 20.0 (IBM Corporation, Armonk, NY, USA) statistical software was used for data processing, and the clinically confirmed diagnosis results were used as control. The age comparison of doctors and patients in daytime and at night was conducted by independent samples t-test; the seniority of doctors, main symptom features of the patients, disease constituent ratio, and diagnostic coincidence rate of ultrasound were tested by Chi-square test. P-values <0.05 were considered statistically significant.
Results
Comparison of the characteristics of ultrasound doctors and the study population
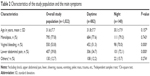
There were 10 doctors engaged in gynecological emergency ultrasound work in the Ultrasound Department of The First Affiliated Hospital of Guangxi Medical University; among whom, 3 worked only in daytime, 3 worked only at night, and other 4 worked both in daytime and at night according to the shift schedule. All of them are female. The youngest was 26 years, and the eldest was 54 years. As resident physicians in the People’s Republic of China need to pass the examination to be promoted to attending physicians when they are in-service for 5 years, therefore, those with ≥6 years in-service are senior physicians, while those with <6 years are junior physicians. The comparison of ultrasound doctors is shown in Table 1.
There were 1,107 patients accepting gynecological emergency ultrasound examination, of whom 85 patients were invalid follow-ups and 1,022 patients were validly tracked. Among the patients who were validly tracked, there were 882 cases in the daytime group and 140 cases in the night group, the youngest was 9 years old and the oldest was 72 years old, and the main symptoms included menolipsis, vaginal bleeding, and lower abdominal pain. Most patients had more than two symptoms at the same time. The patient’s age and symptom characteristics are given in Table 2.
Comparison of disease constituent ratio
Among 1,022 emergency ultrasound patients, 882 patients were in the daytime group and 140 patients were in the night group. Among clinically diagnosed diseases, ectopic pregnancy accounted for 18.7% (165/882) and 46.4% (65/140), intrauterine pregnancy accounted for 33.9% (299/882) and 11.4% (16/140), acute pelvic inflammatory disease accounted for 2.2% (19/882) and 9.3% (13/140), and no organic lesions in uterine and adnexa accounted for 11.3% (100/882) and 2.1% (3/140) in daytime and at night, respectively. All the above mentioned differences were statistically significant (P<0.001), whereas there were no significant differences on the constituent ratio of abortion and trophoblastic diseases, ovarian neoplasms, and uterine and endometrial lesions in daytime and at night (P>0.05), as shown in Figure 1 and Table 3.
  | Figure 1 Contrast chart of disease constituent ratio in daytime and at night. |
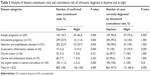  | Table 3 Analysis of disease constituent ratio and coincidence rate of ultrasonic diagnosis in daytime and at night |
Comparison of diagnosis coincidence rate
The overall coincidence rate between the ultrasonic diagnosis and the clinical diagnosis was 96.3% in 1,022 cases, while the coincidence rate of daytime diagnosis was 97.9%, and the coincidence rate of night diagnosis was 86.4%; the difference was statistically significant (P<0.001). Among all diseases, the coincidence rates of ectopic pregnancy ultrasonography diagnosis in daytime and at night were 96.4 and 75.4%, respectively; the difference was statistically significant (P<0.001). However, there was no statistically significant difference in the coincidence rate of other diseases of daytime and night ultrasound diagnoses (P>0.05), as given in Table 3.
Discussion
Differences among the visiting population
As shown in this study, there was no difference in age distribution between the daytime visiting population and the night one. Most of them were women of childbearing age, and 77.8% presented with menolipsis. There was no difference between daytime and night, which indicated that most cases of emergency gynecological ultrasound might be pregnancy-related diseases. However, patients with symptoms of lower abdominal pain in the night group (72.1%) were more than those during the daytime group (34.7%). Obviously, pain could lead to sleep disorders,7 while sleep disorders could urge patients to go to the hospital more quickly to relieve pain. These main symptoms reflected the clinician’s understanding of the emergency indications; patients with lower abdominal pain and vaginal bleeding might have intrauterine abortion or ectopic pregnancy and later might endanger life, so clinicians urgently needed to diagnose by ultrasonography.
Differences in disease constituent ratio
In this study, there were statistically significant differences (P<0.001) on the proportion of ectopic pregnancy, intrauterine pregnancy, acute pelvic inflammatory disease, and no organic lesion in uterine and adnexa in both daytime and night groups. The largest proportion of all diseases was intrauterine pregnancy (33.9%) in the daytime group while ectopic pregnancy (46.4%) in the night group. There were several reasons for disease differentiation: 1) most of the emergency patients had pregnancy-related diseases, the incidence of intrauterine pregnancy in women of child-bearing age was significantly higher than that of ectopic pregnancy, and the sample size of daytime gynecological emergency ultrasound was larger and might be closer to the disease distribution in the population; 2) the symptoms of intrauterine pregnancy patients were mild and the patients might choose their visiting time freely, in most of the patients who suffered from ectopic pregnancy, acute pelvic infection had acute and serious symptoms, and they had to visit the doctor immediately when these symptoms occurred at night; 3) during the day, there were many gynecological ultrasound doctors (≥6) on duty who could accept patients from all departments of the hospital, such as female patients with unexplained acute abdominal pain from gastrointestinal surgery department, to exclude gynecological diseases. However, there was only one ultrasound doctor on duty at night. In order to improve emergency efficiency, the First Affiliated Hospital of Guangxi Medical University suggested that nighttime patients should be consulted by a gynecologist before performing a gynecological emergency ultrasound examination. The gynecologist was professional and targeted, who applied for gynecological emergency ultrasound only if they considered the patient suffering from gynecological disease, such as ectopic pregnancy. Therefore, the disease constituent ratio obtained by gynecological emergency ultrasound statistics could not reflect day-night differences of actual incidence in the population.
In this group of data, there were no statistically significant differences in the ratio between daytime and night of abortion and trophoblastic diseases, ovarian tumor, uterine, and endometrial lesions, regarding the clinical symptoms of these diseases as mild or slow, and patients seeking emergency medical treatment were serious cases, such as ovarian tumor with rupture or torsion or infection, inevitable abortion combining acute hemorrhage of uterus, and cervical cancer with vaginal acute hemorrhage. So far, there has been no literature reporting that the incidence of these diseases during the day and night was significantly different.
Difference of coincidence rate of ultrasonic diagnosis
The overall coincidence rate between the ultrasonic diagnosis of gynecologic emergency and the clinically confirmed diagnosis results was 96.3%, which was similar to results of hospitals of the same rank in the People’s Republic of China.8 It was suggested that ultrasound should be an effective assistant method for gynecologic emergency examination.
There was a difference in the coincidence rate between the ultrasonic diagnosis of gynecologic emergency and the clinically confirmed diseases during the daytime and night, that is, the coincidence rate of night diagnosis in ectopic pregnancy was lower than that of daytime. Ectopic pregnancy accounted for most of the nocturnal diseases (46.4%), ectopic pregnancy was complicated in the pelvic cavity, sometimes the clinical symptoms were atypical, and sonographic changes lacked specificity. Kirk et al9 pointed out that suboptimal quality ultrasound equipment, operator inexperience, increased maternal body mass index, uterine fibroids, or ovarian pathology may also make the visualization of an ectopic pregnancy difficult.
In this study, there were 6 missed diagnoses during the day and 10 missed diagnoses during night and all were proved to be tubal pregnancy. The common features of the 16 patients were short duration of menolipsis (30–42 days), the lesion of <2 cm, mild abdominal pain, and so on, and the ultrasonic examination found no gestation sac in uterine cavity and no abnormal masses in adnexal region, but atypical indirect signs could be seen, such as uterine cavity effusion, endometrial thickening, ovarian corpus luteum cyst, and perirectal fossa free effusion. Of these 16 missed diagnoses, one case had sudden rupture of ectopic pregnancy at the 7th day without reexamination. Data from a specialist of early pregnancy unit show that ~73.9% of women with an ectopic pregnancy may be diagnosed on an initial transvaginal ultrasound examination.10 Therefore, patients who were suspected ectopic pregnancy should be recommended to have close observation and regular follow-ups, and doctors may consider the use of transabdominal sonography in combination with transvaginal sonography to complement information, improve detection rate, and reduce or avoid misdiagnosis and missed diagnosis, which provides a scientific basis for the formulation of clinical treatment scheme.11 In addition, 3 cases of scar pregnancy were misdiagnosed as inevitable abortion and cervical pregnancy at night; the reason was that there were similarities in the sonogram of these diseases, but their clinical management measures were quite different, so ultrasound doctors should pay attention to differential diagnosis. Riaz et al12 summarized the key points of ultrasonic diagnosis of scar pregnancy as 1) no gestational sac was found in the uterus cavity; 2) gestation sac attaching to anterior wall of uterus in the lower section, surrounded by abundant blood flow signals, which was the key point to identify inevitable abortion; and 3) the muscular wall between the gestational sac and the bladder was thin, which could be used to further differentiate cervical pregnancy.
Although our study showed no significant difference in the age and seniority of ultrasound doctors in the daytime group and the night group, the actual situation was that there were more doctors working in the hospital during the day, which means the junior doctors could ask the senior doctors to analyze and judge any problems found, while at night, in most cases, there was only one ultrasonic doctor on duty who had to complete the diagnosis independently and quickly. What is more, there were four of the seven doctors in the night shift whose entire period of actual operation was under 6 years, and these doctors might have the problems such as lack of experience and a low sensitivity to the sonographic changes, and it was difficult for them to make the correct diagnosis independently in a short time.
Another significant reason causing low diagnostic accuracy of ultrasonography at night was the psychological and physiological factors of the night shift doctors. Chronic fatigue caused the decline of the doctors’ physical and mental executions, thereby increasing the incidence of medical errors. A number of studies showed that all the cognitive abilities including working memory ability, information processing speed, spatial thinking ability, and cognitive flexibility of the medical staff who work on the night shift or after 24 hours decreased;13,14 the discrepancy between subjective feeling and objective cognitive impairments poses a risk for performing complex manual and cognitive tasks.15 However, the impact on the night shift ultrasound doctors should be further assessed.
Our findings essentially confirm that ultrasound is a core skill in gynecology but is highly operator dependent. As what is already known, ultrasound performance of trainees in obstetrics–gynecology depended on a combination of motor skills, visual skills, and cognitive skills.16 However, compared with the other clinical assessment tools, ultrasound is the most convenient and reliable imaging modality in the pregnant patient presenting to the emergency department with abdominal pain or vaginal bleeding.2
Limitations
As other similar study,3 we acknowledge that this study is limited by the fact that it was based on the clinician’s “intention to treat” and there was a certain diagnostic suspicion bias. However, sonography is not used in isolation. More information could be gained into an acute gynecology service. Some of the gynecological emergency ultrasound diseases collected in this research did not belong to life-threatening emergencies; since Chinese law states that public hospitals cannot reject any patient, the patients who think themselves are in emergency situation have been admitted to access medical treatment procedures through emergency channels, taking up emergency resources. Before emergency ultrasound examinations, it might be difficult to effectively distinguish the ordinary patients from those with acute diseases, which is the very limitation that this research cannot avoid. In spite of this, our research still has some significance and can provide reference for other research centers.
Conclusion
Due to the distribution of medical resources during the day and night and other reasons, there was significant difference in disease constituent ratio and coincidence rate of ultrasonic diagnosis of gynecological emergency ultrasound of daytime and night and the difference of the diagnostic coincidence rate was mainly manifested by the low coincidence rate of the diagnosis of ectopic pregnancy at night; ultrasound physicians should focus on the accumulation of diagnostic experience for such conditions. Especially for teaching hospitals, doctors should train the medical students to identify the differential diagnosis accordingly in teaching work. In addition, clinicians might suggest patients who performed an gynecologic emergency ultrasound at night with ambiguous diagnosis, to be reexamined during the day, and change a more experienced ultrasound doctor that can avoid missed diagnosis caused by operator-dependence.
Acknowledgment
This work was supported by Talents Highland of Emergency and Medical Rescue of Guangxi Province in the People’s Republic of China (GXJZ201516).
Disclosure
The authors report no conflicts of interest in this work.
References
Mazzei MA, Guerrini S, Cioffi Squitieri N, et al. The role of US examination in the management of acute abdomen. Crit Ultrasound J. 2013;5(suppl 1):S6. | ||
Lambert MJ, Villa M. Gynecologic ultrasound in emergency medicine. Emerg Med Clin North Am. 2004;22(3):683–696. | ||
Haider Z, Condous G, Khalid A, et al. Impact of the availability of sonography in the acute gynecology unit. Ultrasound Obstet Gynecol. 2006;28(2):207–213. | ||
Adhikari S, Blaivas M, Lyon M. Diagnosis and management of ectopic pregnancy using bedside transvaginal ultrasonography in the ED: a 2-year experience. Am J Emerg Med. 2007;25(6):591–596. | ||
Jurkovic D, Mavrelos D. Catch me if you scan: ultrasound diagnosis of ectopic pregnancy. Ultrasound Obstet Gynecol. 2007;30(1):1–7. | ||
Salomon LJ, Nassar M, Bernard JP, Ville Y, Fauconnier A; Société Française pour l’Amélioration des Pratiques Echographiques (SFAPE). A score-based method to improve the quality of emergency gynaecological ultrasound examination. Eur J Obstet Gynecol Reprod Biol. 2009;143(2):116–120. | ||
Ohayon MM. Relationship between chronic painful physical condition and insomnia. J Psychiatr Res. 2005;39(2):151–159. | ||
Cao L, Zhou Y-Q, Zhao W, Xie M. The comparison study of ultrasonography and pathologic results in 1036 gynecologic emergency. Chin J Pract Gynecol Obstet. 2008;24(3):198–200. | ||
Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update. 2014;20(2):250–261. | ||
Kirk E, Daemen A, Papageorghiou AT, et al. Why are some ectopic pregnancies characterized as pregnancies of unknown location at the initial transvaginal ultrasound examination? Acta Obstet Gynecol Scand. 2008;87(11):1150–1154. | ||
Li Y, Feng T, Sun J. Evaluation of clinical effect of transabdominal sonography and transvaginal sonography in early diagnosis of ectopic gestation. Pak J Med Sci. 2017;33(1):53–58. | ||
Riaz RM, Williams TR, Craig BM, Myers DT. Cesarean scar ectopic pregnancy: imaging features, current treatment options, and clinical outcomes. Abdom Imaging. 2015;40(7):2589–2599. | ||
Marquie JC, Tucker P, Folkard S, Gentil C, Ansiau D. Chronic effects of shift work on cognition: findings from the VISAT longitudinal study. Occup Environ Med. 2015;72(4):258–264. | ||
Maltese F, Adda M, Bablon A, et al. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med. 2016;42(3):393–400. | ||
Ernst F, Rauchenzauner M, Zoller H, et al. Effects of 24 h working on-call on psychoneuroendocrine and oculomotor function: a randomized cross-over trial. Psychoneuroendocrinology. 2014;47:221–231. | ||
Tolsgaard MG. Assessment and learning of ultrasound skills in obstetrics & gynecology. Dan Med J. 2018;65(2):B5445. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.