Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 14
Graphite Foreign Body Misdiagnosed as a Blue Naevus-Like Localised Argyria
Authors Sharma A
Received 26 May 2021
Accepted for publication 18 August 2021
Published 16 September 2021 Volume 2021:14 Pages 1253—1256
DOI https://doi.org/10.2147/CCID.S317867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Anushka Sharma
Institute of Clinical Sciences, Imperial College School of Medicine, London, UK
Correspondence: Anushka Sharma
Faculty of Medicine, Imperial College London, Exhibition Road, South Kensington, London, SW7 2BX, UK
Tel +447427404135
Email [email protected]
Abstract: Pencil-tip injuries, although usually insignificant, have the potential to provoke granulomatous reactions. Other undesirable consequences of such injuries include pigmentation and abscess formation. Despite the rarity of such outcomes, it is important that clinicians are aware of the varying presentations of pencil-tip injury, as this can cause diagnostic uncertainty. Here, we present a case of graphite foreign body granuloma, originally thought to be a blue naevus-like localised argyria. The diagnostic work-up was complicated by the absence of a history of injury with a pencil-tip.
Keywords: pencil-tip, granuloma, misdiagnosis, granulomatous reaction
Introduction
The lead pencil is composed of graphite, a crystalline form of elemental carbon, as well as aluminium silicate and waxes. Although usually insignificant, pencil-tip injuries have the potential to provoke granulomatous reactions,1,2 which may lead to undesirable consequences, namely pigmentation and abscess formation.3 While such outcomes are rare, it is important that clinicians are aware of them; a small number of cases have been described in which pencil core granulomas have presented to dermatologists as suspected soft tissue sarcomas, haemangiomas and melanomas.1 Here, we present a case of graphite foreign body granuloma, originally thought to be a blue naevus-like localised argyria. The diagnostic work-up was complicated by the absence of a history of injury with a pencil-tip.
Case Report
In order to share details of this case, institutional approval was obtained. A 74-year-old woman presented with a 10-year-history of an asymptomatic bluish lesion located on the left lateral breast. On inspection, a well-defined blue macule was observed, and a simultaneous hyperkeratotic process was suspected. On palpation, an underlying cyst could not be felt. Examination elsewhere revealed no other related lesions or pigmented areas.
An excision biopsy (17 × 17×5 mm) and staining with haematoxylin and eosin of the lesion revealed black and brown pigment deposits on dermal elastin and collagen fibres, and around sweat ducts (Figure 1). The features were initially thought to indicate a pigment deposition disorder, rather than a melanocytic lesion. This proposal was supported when immunostaining with S100, MelanA and HMB45 failed to show evidence of a melanocytic lesion. The pigment in the dermis also appeared negative for Masson Fontana and Perl’s.
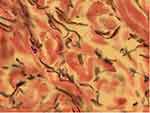 |
Figure 1 Microscopic appearance of the bluish macule after haematoxylin and eosin staining. |
A diagnosis of a single, blue naevus-like localised argyria was proposed. Nonetheless, the patient’s history lacked characteristic features that would normally be anticipated in this type of presentation; there was no report of contact with silver jewellery at the site of the lesion, trauma to the breast, or injections at the site. The patient had not taken any silver-containing medications. The patient revealed that she had mercury and silver dental fillings. It was postulated that mucosal absorption of silver from the fillings was a conceivable explanation; however, we thought it unlikely due to the isolated and localised nature of the lesion.
The histological samples were revisited. A large cluster of black material was observed, surrounded by finer pigmented deposits on dermal collagen (Figures 2 and 3). It was then proposed that this cluster represented an implanted foreign body, which had deposited pigment on surrounding dermal collagen. The histological findings were consistent with a diagnosis of graphite foreign body granuloma.
 |
Figure 2 Large, pigmented cluster on the haematoxylin and eosin-stained histological sample. |
 |
Figure 3 Magnified image of the large, pigmented cluster on the haematoxylin and eosin-stained histological sample. |
Discussion
Non-caseating granulomatous reactions may present as a delayed response to a graphite foreign body.4 The introduction of a graphite foreign body may result from a pencil-tip injury. The histological findings presented in this case are consistent with a reaction to graphite, although other components of pencil lead, namely aluminium silicate and wax, can induce a reactive inflammatory process.5 Whilst few graphite foreign body granulomas have been reported in the literature, all written cases describe a presentation some years after the initial pencil-tip injury, with patients presenting as late as 58 years after the injury.6 It is reasonable that the absence of a pencil-tip injury here may be explained by the patient’s inability to recall such an event that may have occurred several decades earlier.
In keeping with other reports, this case suggests that the response to a graphite foreign body is a delayed granulomatous reaction. Clinicians should consider the possibility of a pencil-tip injury when presented with a localised, pigmented lesion that shows dark, granular pigment on histological staining. Histological examination of the tissue was able to detect granulomatous changes, however it remains unclear whether sophisticated tests should be employed to detect the presence of graphite in tissues given that cases of pencil core granulomas are so rare.7
In this case, a misdiagnosis of a blue naevus-like localised argyria did not drastically alter the patient’s management. However, the case should prompt us to consider the potentially devastating complications that arise as a result of diagnostic uncertainty. The literature has described a clinical resemblance between pencil core granulomas and malignant melanoma.1 A misdiagnosis of a malignant melanoma could expose an otherwise well patient to harmful chemotherapeutic agents. Simultaneously, a misdiagnosis of a pencil-tip granuloma in the presence of melanoma could delay life-saving treatment.
Summary
In summary, the possibility of trauma to the site in question should be explored in detail, as the delay between sustaining a pencil-tip injury and presentation to dermatology can be decades. As a result, key features of the history may not be offered by the patient.
Consent Statement
Informed consent was received from patient to use details of the case in this report.
Funding
No external funding.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Fukunaga Y, Hashimoto I, Nakanishi H, et al. Pencil-core granuloma of the face: report of two rare cases. J Plast Reconstr Aesthet Surg. 2011;64(9):1235–1237. doi:10.1016/j.bjps.2011.01.017
2. Terasawa N, Kishimoto S, Kibe Y, Takenaka H, Yasuno H. Graphite foreign body granuloma. Br J Dermatol. 1999;141(4):774–776. doi:10.1046/j.1365-2133.1999.3144c.x
3. Jin Kim Y, Young Ahn J, Joon Kim B, et al. A case of graphite foreign body misdiagnosed as blue nevus. Ann Dermatol. 2007;19(4):166. doi:10.5021/ad.2007.19.4.166
4. Granick MS, Erickson ER, Solomon MP. Pencil-core granuloma. Plast Reconstr Surg. 1992;89(1):136–138. doi:10.1097/00006534-199289010-00030
5. Gormley RH, Kovach SJ, Zhang PJ. Role for trauma in inducing pencil ‘lead’ granuloma in the skin. J Am Acad Dermatol. 2010;62(6):1074–1075. doi:10.1016/j.jaad.2009.02.027
6. Taylor B, Frumkin A, Pitha JV. Delayed reaction to “lead” pencil simulating melanoma. Cutis. 1988;42(3):199–201.
7. Aswani VH, Kim SL. Fifty-three years after a pencil puncture wound. Care Rep Dermatol. 2015;7:303–305. doi:10.1159/000441248
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
