Back to Journals » Clinical Interventions in Aging » Volume 13
Good function and high patient satisfaction at mean 2.8 years after dual mobility THA following femoral neck fracture: a cross-sectional study of 124 patients
Authors Tabori-Jensen S , Hansen TB , Bøvling S, Aalund P , Homilius M , Stilling M
Received 21 November 2017
Accepted for publication 2 March 2018
Published 9 April 2018 Volume 2018:13 Pages 615—621
DOI https://doi.org/10.2147/CIA.S157671
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Steffan Tabori-Jensen,1,2 Torben B Hansen,1,2 Søren Bøvling,1 Peter Aalund,1 Morten Homilius,1 Maiken Stilling1,2
1University Clinic for Hand, Hip and Knee Surgery, Regional Hospital West, Holstebro, Denmark; 2Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Aims: Our aim was to investigate function, health status and satisfaction in patients treated with primary dual mobility (DM) total hip arthroplasty (THA) after displaced femoral neck fracture (FNF).
Patients and methods: From 2005–2011, 414 consecutive FNF patients received Saturne DM THA. At a minimum of 1-year follow-up, 124 (95 women) were evaluated with Oxford Hip Score (OHS), Harris Hip Score (HHS), health-related quality of life (HRQoL) measure (EQ-5D) and two functional tests: Timed Up and Go (TUG) and Sit to Stand 10 times (STS). The FNF patients were matched 1:2 by age, sex and surgery date with patients receiving THA due to osteoarthrosis (OA group) and 1-year OHS and EQ5D were compared. FNF patients were matched by age and sex with the general population index (GPI) for EQ-5D comparison.
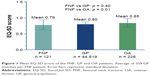
Results: Patient age at surgery after FNF was mean 74.8 (range 30–92) years. At mean follow-up of 2.8 (range 1.0–7.7) years, mean EQ-5D score was 0.79 (SD 0.15) in the FNF group, which was similar to the matched GPI (p = 0.4), but lower (p = 0.014) compared to the OA group. Mean OHS was 36.4 (SD 9.5) in the FNF group and 38.4 (SD 7.2) in the OA group (p = 0.18). HHS in the FNF group was 78.7 (SD 15.5). Mean TUG time was 13.5 (SD 4.9) secs, and mean STS was 37.9 (SD 15.3) secs. Eighty nine percent (n = 111) of FNF patients were satisfied with the operation result.
Conclusion: DM THA following displaced FNF provides a good functional result and quality of life in addition to high patient satisfaction.
Keywords: dual mobility cup, femoral neck fracture, hip arthroplasty, EQ-5D, Oxford Hip Score, patient reported outcome measures
Plain language summary
The proportion of older people in the world is increasing. Total hip arthroplasty (THA) is a common and well-established procedure for displaced femoral neck fractures (FNFs) due to the risk of femoral head necrosis after osteosynthesis with approximately 600 surgeries performed annually in Denmark. The demand for well-functioning implants that not only have low implant complications profile but also maintain the patients function and mobility after surgery is essential. In this cross-sectional study, we investigated the function, mobility and satisfaction in patients receiving a dual-mobility (DM) THA. A total of 414 patients were operated on between January 2005 and December 2011. In 2012, we evaluated 124 patients with two questionnaires (Oxford Hip Score [OHS] and Harris Hip Score [HHS]) regarding their postoperative function, health-related quality of life (HRQoL) and we did two functional capacity tests, Timed Up and Go (TUG) and Sit to Stand 10 times (STS). The patients were matched 1:2 to a patient group receiving a THA due to osteoarthritis (OA group). For the HRQoL, results were matched to the general population index (GPI). The mean follow-up time was 2.8 years and the mean age was 74.8 years. Of the 124 FNF patients investigated, 89% were satisfied with the operation. We found slightly lower HRQoL results in the FNF patients compared to the matched OA group, but HRQoL was similar to the large matched GPI group. OHS results for the FNF patients were comparable to the OA group. The functional capacity tests translate into good function. We concluded that using DM THA in the treatment of FNF patients provides good functional results and quality of life in addition to high patient satisfaction.
Introduction
Hip fracture is one of the biggest health care challenges in the 21st century. The reason is the reversing aging pyramid and longer life expectancy, which increases morbidity, mortality and socioeconomic costs related to hip fractures.1 Displaced femoral neck fracture (FNF) is a common injury in the elderly, and treatment with total hip arthroplasty (THA) has low complication and revision rates compared to internal fixation and hemiarthroplasty.2,3 The dual-mobility (DM) hip articulation has a mobile femoral head captured in the polyethylene (PE) liner so that the large diameter PE essentially functions as a large femoral head similar to that of the anatomical/native femoral head. This design, theoretically increases range to impingement and improves stability compared to conventional hip implants.4 The DM articulation has proven effective in reducing the THA dislocation risk in fragile FNF patients, demented and patients with a high risk of falling.5
Traditionally, the outcome after surgery has been measured in relatively tangible data such as mortality, reoperation, surgical implant success and radiographic results. Less is known about the patient-centered and functional outcome after ended rehabilitation in fragile FNF patients.6,7 There is increasing focus on patient-related outcome measures (PROMs) but little consensus among professionals on which measures to use, and which outcomes patients see as important. There are five major categories in assessing outcome measurements; general health-related quality of life (HRQoL), activities of daily living (ADLs), mobility and physical performance scales, disease-specific scales and joint-specific scales.7 It is advised to use scales from more than one category to assess outcome.
In Denmark, 568 THA out of 9,674 annual THA (all diagnoses, 2015) are performed due to FNF. There is no national follow-up on patient-reported outcomes after THA for treatment of FNF in Denmark.8
The aim of the present study was to investigate the function, health status and satisfaction in patients treated with primary DM THA after displaced FNF in comparison with 1) an age- and gender-matched group of patients treated with THA due to hip osteoarthritis (OA) and 2) the background population. We hypothesized that FNF patients treated with DM THA gain good function and high satisfaction at the level of hip OA patients treated with primary THA.
Patients and methods
Patients
The study design was a cross-sectional clinical cohort follow-up study with prospective evaluation of the function, health status and satisfaction in patients treated with primary THA after displaced FNF compared to 1) a matched group of patients treated with THA inserted due to OA, and 2) the age-matched background population.
In 2005 the Saturne® DM Acetabular System (Amplitude, Valence, France) became the standard treatment in our department for Garden type III and IV displaced FNF9 in combination with a cemented Exeter stem or a cementless Corail stem. Cemented or cementless fixation according to bone quality and the surgeon’s preference. Regardless of mental status, patients were given the same treatment.
Between January 2005 and December 2011, 414 consecutive FNF patients received a Saturne DM THA at the time of follow-up 155 were dead. The etiology of the FNF was low velocity mechanical fall in all cases. At a minimum of 1-year follow-up, 124 patients (95 women) with a mean age of 77.6 age (range 37.2–94.3) responded to an invitation and were evaluated in our outpatient clinic. Of the 124 patients, 56 cups and 83 stems were cemented.
All patients surgeries were through a posterolateral approach and they received the same postoperative rehabilitation program as OA patients. To prevent infection 1 g Diclocil® (dicloxacilline) was administrated preoperatively as well as three times during the first 24 postoperative hours. From the first postoperative day, the mobility goal was for the patient to be out of bed 4 hours including training with the physiotherapist and occupational therapist, and 8 hours per day for the rest of the hospitalization period.
At the cross-sectional follow-up, and after informed consent, all FNF patients reported their quality of life EQ-5D, Oxford Hip Score (OHS), New Mobility Score (NMS) and satisfaction with the DM THA treatment.10–14 A nurse assisted the patient in recalling the preoperative NMS. Harris Hip Score (HHS) including a hip examination was completed.15 Functional capacity was tested with Timed Up and Go (TUG) time as well as Sit to Stand 10 times (STS).16
Patients had their cognitive function tested at follow-up with a Danish version of the abbreviated 0–9 mental status test, where a test score between 0 and 5 is considered low cognitive function.17 For those participants with cognitive impairment (n = 10), the journal and questionnaire was reassessed and in total five patients were excluded because we felt their cognitive function was too impaired for the answered questionnaires to be valid and useful.
All the patients were offered a standard package of postoperative clinical controls from our standard clinical pathway, and by attending the controls the patients gave their consent to participate and no written consent was needed.
FNF patients were matched 1:2 by age, sex and surgery date with patients receiving THA due to hip osteoarthrosis (OA) where all had been followed to 1 year with OHS and EQ-5D. The FNF patients were further matched to the general population index (GPI) for comparison of EQ-5D scores.
Matching
We performed matching with two different control groups for comparison of PROM data with our FNF case group.
- 2:1 matching on EQ-5D and OHS to the hip OA group receiving THA at the Hospital Unit West between the years 2008 and 2013 (n = 1,250). The FNF patients were matched on three parameters (gender, age in 5-year age intervals and surgery year). A control patient was only used for a single match. We obtained a full match on all three parameters for 76 patients, and a partial match (gender and age, but not on operation year) for 42 patients, where we further attempted to minimize the difference in operation year. Six FNF patients could not be matched at all. Double match was possible in 88% of full matches and in 97% of partial matches. All full and partial matches were used for comparison of EQ-5D and OHS (n = 226).
- EQ-5D scores of the FNF patients was matched to the general population norms based on the study of 15,700 respondents in the Danish general population.18 FNF cases were divided into 5-year intervals and thereafter matched on gender- and age-related (5-year intervals) population norm. On average, there were 359 matches in the general population group per FNF case, but all possible matches were used for the comparison of life quality (n = 44,519).
The Central Danish Regional Committees on Biomechanical Research Ethics reviewed the study and judged it as a quality control, and therefore according to Danish law no approval was necessary (inquiry 149/2012 of October 1, 2012).
Statistical analysis
Non-parametric (Mann–Whitney) statistics was used for continuous data, where data were not normally distributed according to a Shapiro–Wilks test, and parametric (Student’s t-test) statistics where data was normal distributed.
Linear regression was used to compare the FNF group to the matched OA group for scores in EQ-5D, and likewise linear regression was used to compare OHS between FNF patients and the matched OA group. Correlations were evaluated by Spearman’s correlation test.
For comparability with the literature, and for interpretability reasons, we present the mean values for data without a Gaussian distribution (TUG, STS, EQ-5D, HHS and OHS).
Statistical significance was set at the 5% level and all statistical computations were undertaken with Intercooled Stata version 13.1 (StataCorp LP, College Station, TX, USA).
Results
The demographics for the FNF group are summarized in Table 1.
Comparison with matched OA THA group
FNF patients had a mean EQ-5D of 0.79 (range 0.37–1.0, SD 0.15). The adjusted (gender, age and operation year) estimate of the mean difference of EQ-5D from FNF patients to OA patients was 0.06 (95% CI 0.1, 0.01, p = 0.014).
The statistical difference between the FNF patients and the OA patients was found to be in question 1 concerning mobility (p = 0.002) and question 4 concerning pain/discomfort (p = 0.0043).
The adjusted estimate of the mean OHS difference between FNF patients and OA THA patients was 1.66 (95% CI −4.10, 0.78, p = 0.18). There was no difference in OHS score between genders in the FNF group (p = 0.74).
Comparison with matched GPI
There was no difference in EQ-5D between FNF patients and the gender- and age-matched general population norm (p = 0.40). EQ-5D results for FNF, GP and OA patients are shown in Figure 1.
The age matched (age > 75 years) HHS for the general population has been reported to be 93.7 (SD 7.1),19 and the HHS of the FNF patients in our study was lower than the reported population level (p < 0.0001), but 20% of the FNF patients had a score at or above the general population level at follow-up. In the FNF group, there were similar HHS between genders (p = 0.98).
There was a good correlation between HHS and EQ-5D (rho = 0.60, p < 0.0001) and between HHS and OHS in the FNF patients (rho = 0.65, p < 0.0001).
At follow-up, 89.5% (n = 111) scored their overall satisfaction with the operation outcome as either very good (n = 71) or good (n = 40). Satisfaction had a moderate correlation to EQ-5D (rho = −0.42), OHS (rho = −0.52) and HHS (rho = −0.48), all significant (p = <0.0001).
Complications
Of the FNF patients, four underwent revision surgery during follow-up. One patient had stem-revision because of a fall-related stem fracture 58 days after primary surgery. One patient in immunosuppressive therapy was successfully revised to debridement, washout and arthrotomy because of a Staphylococcus epidermidis acute deep infection, and no components were replaced. Two patients underwent revision surgery because of aseptic loosening, one with cup loosening and one with femoral stem loosening. One hemiplegic patient sustained a fall 17 days after surgery and had a hip dislocation, which was treated with closed reduction.
The patients who experienced complications all had below average scores in the follow-up PROMS and functional tests compared to the other FNF patients.
Discussion
To the best of our knowledge, this is the first study of mobility, physical performance, PROMs and treatment satisfaction exclusively in hip fracture patients treated with DM THA.
It is recommended to use scales from more than one of the five overall categories when measuring outcome after FNF, as there is no single unifying scale for assessing outcome after FNF.6,7 In this cross-sectional study, we focused on three out of the five categories, namely, general quality of life (EQ-5D), mobility and physical performance (TUG, STS) and hip-specific scores (OHS, HHS).
EQ-5D
The FNF patients in this study had a mean EQ-5D score of 0.79 (range 0.37–1.0) with follow-up between 12 and 90 months, which was better than reported in other studies of FNF patients treated with THA, with EQ-5D scores ranging from 0.61 to 0.71 with follow-up length between 12 and 48 months.20–23 We found a slightly lower EQ-5D score compared with the matched OA THA group, but the clinical relevance is questionable. In general, OA patients have fewer comorbidities than FNF patients and the follow-up time was mean 1.8 years longer for the FNF patients than for the matched OA THA patients, which may also have contributed to the difference, as function and health status decline with the passage of time especially in comorbid FNF patients.21 Positively, the EQ-5D for the FNF patients in our study were comparable or slightly better than EQ-5D values 6 months after surgery in British patients receiving THA for OA, which is reported to be 0.76 in the age range 70–80 in 2010/2011.24
We found no difference to the age- and gender-matched large general population group in EQ-5D.18
OHS
We expect both FNF and OA patients to have reached peak hip function 1 year after surgery, but possibly function may also decline again after 1 year due to aging and fragility.20,22 In spite of the longer follow-up in FNF patients, we found no difference in OHS score between the FNF patients and the age- and gender-matched OA THA group, and the mean OHS score of 36.4 translates to a good result in the FNF patients.
A combined normal population OHS reference in the age range 70–79 from Australia and Canada was 42.5.25 This score was based on a quite low total number of 70 persons from the two countries, which bears a risk of selection bias, and further cross-nation norm data might also be different.
HHS
HHS of 78.7 in the FNF patients of this study translates to a fair result which is lower than other studies of FNF patients.22,23,26,27 We found a lower HHS compared to the age (>75)-matched general population level by Lieberman et al, and to the reported HHS values of 93.1 for the age range 70–79 years in McLean et al.19,25 Both studies were based on a low number of respondents, 44 and 70, respectively, and Lieberman et al used telephone administrated questionnaire and no clinical assessments. Furthermore, both studies might have cultural composition differences that may not be comparable to that of our study group.
Time Up and Go test and Sit to Stand test
The TUG score of 13.5 secs (range 4.5–30.1) in the FNF patients is below the predictive cutoff fall values for community-dwelling older adults of 14 secs and that of 24 secs within the first 6 months after discharge after hip fracture operation.28,29 TUG score <20 secs translates to good mobility in terms of “can go out alone, mobile without gait aid,” and this was found in 90.5% of the FNF patients in our study.16
STS
STS 10 times repeated time measure has not been reported for FNF or OA patients before. The more widely used STS test is either 5 times STS or 30 secs STS.30 We found that a correlation between TUG and STS in the FNF patients was moderate to strong correlation (rho = 0.58), and we cautiously interpret this as a fairly good performance although we do not have directly comparative studies.
NMS
Of the FNF patients, 84.5% (n = 70) had a NMS higher than 6 at follow-up which translates into a high score with good mobility and functional level.29 Patients scored their recalled preoperative NMS higher than their postoperative score. This difference could potentially be recall bias, as the preoperative NMS evaluation was collected at a postoperative cross-sectional follow-up interview in the outpatient clinic at a mean follow-up of 2.8 years. The difference could also be attributed the general functional decline elderly experience over time.
Limitations
Elderly sustaining a FNF is a heterogeneous patient group ranging from healthy independent subjects, to patients demanding a high level of functional assistance, to even institutionalized and bedridden subjects. As a result, there is a natural high loss to follow-up to consider in any hip fracture study, which also was the case in this study.
The current study has several limitations that should be considered. Patient selection is one of the primary limitations of this study, as 37% (n = 155) patients were dead at follow-up, and of the remaining patients only 47% (n = 124) were sufficiently fit and willing to participate in the clinical examination. Thus, we probably evaluated only the best of the FNF patients. Longer follow-up would most likely have resulted in greater loss of patients available for evaluation, as the mortality rates and comorbidities of FNF patients are high.
The cross-sectional study design did not option data collection of preoperative mobility and physical performance data (TUG and STS) and PROM data (EQ-5D, OHS and HHS), and the absence of repeated measurements to detect change before and after intervention might not generate a true outcome.31 It is questionable that the PROMs developed for the evaluation of specific joints and HRQoL are suitable for evaluation after a proximal femoral fracture. The reason for this is that most of these scales were developed to evaluate patients after operation due to OA. Furthermore, older and fragile FNF patients may tend to view their limitation causality to aging, making it challenging to evaluate the FNF impact from the comorbidities patients may experience.6 The existence of four suitable validated scores for hip-related outcome scales for the use in patients with proximal femoral fractures calls for a shift in the widely used scales when evaluating the complex patient group that proximal femoral fracture patients represent.7 The need for implementing more robust and rigorous scoring systems is evident for clearer recommendations for future investigations.
Conclusion
At short-term follow-up, patients with DM THA following displaced FNF had a good functional and satisfaction result. Some 89% (n = 111) of the patients were satisfied with the surgical outcome. EQ-5D was similar to the age/gender-matched population index, but lower compared with OA THA patients. We found good functional and mobility outcomes on TUG test, STS and NMS for FNF patients. Hip-specific questionnaires revealed good results for FNF patients, and for OHS, the results were at the same level as the age, gender and surgery time-matched OA THA patients.
Acknowledgments
The abstract for this article was presented as a poster presentation at the annual PhD day at Aarhus University, January 2017. The authors are grateful to Professor Jan Soerensen, University of Southern Denmark, for collaboration and willingness to assist with the EQ-5D matching to the general population data.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Hansen L, Mathiesen AS, Vestergaard P, Ehlers LH, Petersen KD. A health economic analysis of osteoporotic fractures: who carries the burden? Arch Osteoporos. 2013;8:126. | ||
Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010;340:c2332. | ||
Johansson T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: a minimum fifteen-year follow-up study of a previously reported randomized trial. J Bone Joint Surg Am. 2014;96(6):e46. | ||
Cross MB, Nam D, Mayman DJ. Ideal femoral head size in total hip arthroplasty balances stability and volumetric wear. HSS J. 2012;8(3):270–274. | ||
Adam P, Philippe R, Ehlinger M, et al. Dual mobility cups hip arthroplasty as a treatment for displaced fracture of the femoral neck in the elderly. A prospective, systematic, multicenter study with specific focus on postoperative dislocation. Orthop Traumatol Surg Res. 2012;98(3):296–300. | ||
Haywood KL, Brett J, Tutton E, Staniszewska S. Patient-reported outcome measures in older people with hip fracture: a systematic review of quality and acceptability. Qual Life Res. 2017;4:799–812. | ||
Hutchings L, Fox R, Chesser T. Proximal femoral fractures in the elderly: how are we measuring outcome? Injury. 2011;42(11):1205–1213. | ||
Danish Hip Replacement Registry. National annual report 2016. 2016. Available from: https://www.sundhed.dk/content/cms/98/4698_dhr-årsrapport-2016.pdf. Accessed March 27, 2018. | ||
Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43B(4):647–663. | ||
Murray DW, Fitzpatrick R, Rogers K, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89(8):1010–1014. | ||
Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–190. | ||
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. | ||
Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75(5):797–798. | ||
Danish Hip Replacement Registry—Satisfaction score THA. 1996; page 11. Available from: http://www.rkkp.dk/siteassets/om-rkkp/de-kliniske-kvalitetsdatabaser/hoftealloplastik/data-definition-for-dansk-hoftealloplastik-register.pdf. Accessed March 27, 2018. | ||
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. | ||
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. | ||
Qureshi KN, Hodkinson HM. Evaluation of a ten-question mental test in the institutionalized elderly. Age Ageing. 1974;3(3):152–157. | ||
Sørensen J, Davidsen M, Gudex C, Pedersen KM, Brønnum-Hansen H. Danish EQ-5D population norms. Scand J Public Health. 2009;37(5):467–474. | ||
Lieberman JR, Hawker G, Wright JG. Hip function in patients >55 years old: population reference values. J Arthroplasty. 2001;16(7):901–904. | ||
Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003;85(3):380–388. | ||
Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005;87(8):1680–1688. | ||
Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89(2):160–165. | ||
Hedbeck CJ, Enocson A, Lapidus G, et al. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011;93(5):445–450. | ||
Clarke A, Pulikottil-Jacob R, Grove A, et al. Total hip replacement and surface replacement for the treatment of pain and disability resulting from end-stage arthritis of the hip (review of technology appraisal guidance 2 and 44): systematic review and economic evaluation. Health Technol Assess. 2015;19(10):1–668, vii–viii. | ||
McLean JM, Cappelletto J, Clarnette J, et al. Normal population reference values for the Oxford and Harris Hip Scores—electronic data collection and its implications for clinical practice. Hip Int. 2017;27(4):389–396. | ||
Mouzopoulos G, Stamatakos M, Arabatzi H, et al. The four-year functional result after a displaced subcapital hip fracture treated with three different surgical options. Int Orthop. 2008;32(3):367–373. | ||
Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S200–S207. | ||
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. | ||
Kristensen MT, Foss NB, Kehlet H. Timed “up & go” test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther. 2007;87(1):24–30. | ||
Mikkelsen LR, Mechlenburg I, Søballe K, et al. Effect of early supervised progressive resistance training compared to unsupervised home-based exercise after fast-track total hip replacement applied to patients with preoperative functional limitations. A single-blinded randomised controlled trial. Osteoarthritis Cartilage. 2014;22(12):2051–2058. | ||
Rolfson O, Bohm E, Franklin P, et al. Patient-reported outcome measures in arthroplasty registries. Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. 2016;87:9–23. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.