Back to Journals » Clinical Ophthalmology » Volume 17
Glycated Hemoglobin Improvement After Medical and Surgical Eye Care in American Veterans Involves Multidisciplinary Care
Authors Santilli CM , Johnson S, Thunstrom CR, Armbrust KR
Received 12 March 2023
Accepted for publication 12 May 2023
Published 10 June 2023 Volume 2023:17 Pages 1675—1682
DOI https://doi.org/10.2147/OPTH.S412187
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Christopher M Santilli,1 Shaun Johnson,2 Coltt R Thunstrom,3 Karen R Armbrust1,4
1Department of Ophthalmology and Visual Neurosciences, University of Minnesota, Minneapolis, MN, USA; 2School of Medicine, Case Western Reserve University, Cleveland, OH, USA; 3Department of Statistics, University of Minnesota, Minneapolis, MN, USA; 4Department of Ophthalmology, Minneapolis Veterans Affairs Health Care System, Minneapolis, MN, USA
Correspondence: Karen R Armbrust, Minneapolis VA Health Care System, Mail Code 112N, One Veterans Drive, Minneapolis, MN, 55417, USA, Tel +1 612-467-3857, Fax +1 612-727-5972, Email [email protected]
Purpose: The effects of diabetes mellitus (DM) on visual function have been extensively studied. Fewer studies evaluate the effect of visual function on DM, and previous small studies have shown mixed results concerning the relationship between glycated hemoglobin (HbA1c) and cataract surgery. We performed a retrospective, observational, single-site study at a Veterans hospital to evaluate this relationship and the relationship between HbA1c and non-surgical eye care.
Patients and Methods: We compared pre- and post-operative/examination HbA1c in 431 surgical and 431 matched, non-surgical subjects who underwent eye examination at the same institution. Subgroup analysis was performed by age, elevated (≥ 8) pre-operative/examination HbA1c, and change in diabetic management. We also assessed for a relationship between changes in best-corrected visual acuity (BCVA) and HbA1c. The Minneapolis Veterans Affairs Health Care System Research Administration determined this study to be Institutional Review Board exempt from the requirements of 38 CFR 16 under Category 4 (iii).
Results: Pairwise comparison of pre- versus post-operative HbA1c trended towards reduction at 3– 6 months in all surgical subjects, with a statistically significant reduction in older subjects, and those with higher pre-operative HbA1c. Eye examination subjects experienced a significant HbA1c reduction 3– 6 months after eye examination. Reduction in post-operative/examination HbA1c was associated with concurrent change in diabetic management.
Conclusion: We found an overall reduction in HbA1c in diabetic Veterans who interacted with an ophthalmologist, whether for cataract surgery or eye examination. HbA1c reduction was greatest when ophthalmic care was delivered as part of a multidisciplinary care team. Our findings add new evidence to further support the importance of ophthalmic care in patients with DM and suggest improved visual function may facilitate improved glycemic control.
Keywords: cataract, cataract surgery, diabetes mellitus, glycated hemoglobin
Introduction
The prevalence of diabetes mellitus (DM) disproportionately affects United States Veterans with nearly double the prevalence of DM in the Veteran (25%) versus national (10%) population.1 This situation can be expected to worsen as the prevalence of DM nationwide has been increasing and is predicted to continue to increase.2,3 Additionally, population-based measures show recent worsening of glycemic control. National Health and Nutrition Examination Survey data analysis shows that the percentage of DM patients with a glycated hemoglobin (HbA1c) <7.0% decreased nearly 7% from 2007–2010 to 2015–2018.4 The effects of poor glycemic control on worsening visual function, such as accelerated cataract formation and diabetic retinopathy, have been well studied.3 The converse also may be true, with impaired visual function leading to suboptimal glycemic control in DM through several potential mechanisms: limiting physical activity, impeding medication administration, and/or affecting other lifestyle factors.5 While it is standard of care to include ophthalmology as part of the multidisciplinary management of DM to prevent systemic disease from affecting visual function, it is not known whether improving visual function benefits systemic disease control.
One way to evaluate the potential effect of visual impairment on glycemic control is to compare HbA1c levels before and after cataract surgery, a procedure which typically improves visual function quickly and dramatically.6 Prior small studies examining changes in HbA1c levels after cataract surgery in patients with DM have shown mixed results. One study of 28 subjects showed a significant reduction in HbA1c by 0.45% at 4 months post-operatively with greater reduction in younger patients and those with higher pre-operative HbA1c levels,7 but a second study with 24 subjects showed no significant change in HbA1c at 7 months.8 To address the controversy raised by these dissimilar findings in small studies, we performed a retrospective, observational study using a much larger cohort to evaluate changes in HbA1c after cataract surgery at a single Veterans Affairs hospital.
Additionally, we hypothesized that nonsurgical eye care may be associated with changes in HbA1c. To test this hypothesis and compare changes in HbA1c with surgical versus non-surgical eye care we developed an age, sex, and baseline HbA1c-matched cohort with eye examination at the same Veterans Affairs hospital. The aim of our study is to assess whether receiving cataract surgery or non-surgical eye care is associated with changes in glycemic control as measured by HbA1c. We also investigated whether concurrent changes in diabetes management occurred in our study cohorts.
Materials and Methods
Data Acquisition
We performed a retrospective chart review utilizing the Veterans Affairs Informatics and Computing Infrastructure to query data from the Veterans Health Administration’s Corporate Data Warehouse.9,10 The Minneapolis Veterans Affairs Health Care System Research Administration determined this study to be Institutional Review Board exempt from the requirements of 38 CFR 16 under Category 4 (iii). This research adhered to the tenets of the Declaration of Helsinki.
Cataract Surgery Cohort
We evaluated all patients who underwent first eye cataract surgery from January 1, 2015 to December 31, 2019 at the Minneapolis Veterans Affairs Health Care System (MVAHCS) with HbA1c drawn both 0–90 days (0–3 months) prior to and 90–180 days (3–6 months) after cataract surgery. We classified patients as having a pre-operative diabetes mellitus diagnosis if they had International Classification of Disease (ICD)-9 (250.x) or ICD-10 (E10.x – E14.x) diabetes mellitus diagnosis codes associated with at least 1 hospitalization based on discharge diagnoses or at least 2 outpatient visits prior to cataract surgery.11 If available, we also recorded HbA1c 690–780 days (2 years) after cataract surgery. The primary outcome measure was the difference in HbA1c before and 3–6 months after cataract surgery for all surgical subjects. Since Bar-Oz et al found greater reductions in HbA1c for younger subjects and those with pre-operative HbA1c ≥8.0%,7 we performed prespecified subgroup analyses by the mean age (71 years) of subjects in our study population and in those with a pre-operative HbA1c > 8.0%. The subgroups of pre-operative HbA1c ≥8.0% and division by mean age were selected prior to analysis of data.
Visual Acuity Measurement
Pre-operative and 1–2-month post-operative best corrected visual acuity (BCVA) was recorded for the cataract surgery cohort. Clinically significant improvement in BCVA was defined as an improvement of >0.2 units on the logarithm of the Minimum Angle of Resolution (logMAR) scale.12 BCVA improvement of >0.2 logMar units corresponds to at least 2 Snellen lines. BCVA reported as “counting fingers” and “hand motion” was converted to 20/1500 and 20/4000, respectively.13
Eye Examination Cohort
Non-surgical subjects were matched by age, sex, and pre-examination HbA1c. These subjects also presented to the eye clinic at the MVAHCS from January 1, 2015 to December 31, 2019 and had HbA1c measured 0–3 months prior to and 3–6 months after their eye clinic visit, but were phakic bilaterally at presentation and did not undergo cataract extraction prior to the date of their 3–6 month post-examination HbA1c. A variance of ± 0.02% was accepted for matching of the pre-examination HbA1c, and a variance of ±1 year of age was accepted for age matching.
Determination of Change in Diabetic Management
To account for other variables that may influence changes in HbA1c the subjects from the cataract surgery and eye examination cohorts were subdivided depending upon whether they underwent any change in diabetic management from 3 months prior to surgery or eye examination to 3 months prior to the post-operative/examination HbA1c date. Any of the following constituted a change in diabetic management: addition of a new glycemic medication, increased dose of a current glycemic medication, changing the class of glycemic medication, or participating in an initial consultation with a dietician, diabetes case manager, or physician related to DM care. These non-pharmaceutical interventions have been found to have comparable impacts on lowering HbA1c to diabetic medications.14–17 Subjects were excluded from the change in diabetic management analysis if their diabetic management was not available in the electronic medical record.
Statistical Analysis
HbA1c before and after cataract surgery or eye examination was compared using a paired, two-tailed Student’s t-test. Statistical significance was set at α = 0.05, with the Holm-Bonferroni method used to adjust for multiple comparisons. BCVA was converted from Snellen visual acuity to the logMAR scale for statistical analysis. Correlations between the pre- and post-operative changes in BCVA and HbA1c were analyzed with Pearson’s coefficient. All statistical analyses were performed in SPSS v.25.
Results
Cataract Surgery Cohort
Of the 4058 patients undergoing cataract surgery during the study period at the MVAHCS, 1645 patients (41%) had a pre-operative diagnosis of diabetes mellitus based on ICD coding, and 431 subjects met our study inclusion criteria for pre-operative and post-operative HbA1c timing. The mean (median) age of the cataract surgery cohort with pre-operative and 3–6 month post-operative HbA1c measurements was 71.8 (71) years, and 419 (97%) were male. Pairwise comparison of pre- and post-operative HbA1c showed a trend toward HbA1c reduction at 3–6 months (7.68% to 7.56%, P = 0.063), with a significant HbA1c reduction in older subjects (7.62% to 7.39%, P = 0.004) and those with pre-operative HbA1c ≥8.0% (9.24% to 8.59%, P < 0.001) (Table 1 and Figure 1).
 |
Table 1 Change in HbA1c† 3–6 Months After Cataract Surgery |
 |
Figure 1 Mean pre- (dark grey) vs post- (light grey) operative/examination glycated hemoglobin (HbA1c). |
To test whether cataract surgery had a prolonged effect on glycemic control, we evaluated the 155 subjects (36%) in the cataract surgery cohort with HbA1c recorded 2 years after cataract surgery (Table 2 and Figure 1). We found a reduction in the 2-year post-operative HbA1c (7.96% to 7.69%, P = 0.047) that did not reach significance after Holm-Bonferroni correction in this group, with a significant reduction in those with pre-operative HbA1c ≥8.0% (9.45% to 8.35%, P < 0.001).
 |
Table 2 Change in HbA1c† 2 Years After Cataract Surgery |
Change in Visual Acuity
As anticipated, the cataract surgery cohort had post-operative improvement in BCVA: the mean post-operative change in BCVA was −0.328 logMAR with a standard deviation of 0.40. We evaluated whether 3–6 month post-surgical HbA1c reduction was associated with visual acuity improvement by comparing the HbA1c change in cataract surgery subjects with and without post-operative BCVA improvement of ≥ 0.2 logMAR, or at least 2 lines of improvement on Snellen visual acuity. Contrary to our hypothesis that visual improvement would be associated with improved glycemic control, there was minimal reduction in mean HbA1c (−0.02%) in the 271 subjects with post-operative BCVA improvement ≥ 0.2 logMAR, and the 155 subjects without this amount of post-operative BCVA improvement had a larger reduction in mean HbA1c (−0.29%). Additionally, we found no linear correlation between the change in BCVA and the change in HbA1c (Pearson’s r = 0.001).
Eye Examination Cohort
To evaluate whether the 3–6 month post-surgical HbA1c reduction is specific to cataract surgery or is found more broadly in patients receiving ophthalmic care, we established an age, sex, and baseline HbA1c-matched eye examination cohort consisting of patients with HbA1c measurements recorded 0–3 months prior to and 3–6 months after eye examination at the same institution. In this matched cohort, we found a significant reduction in HbA1c of 0.20% (7.70% to 7.50%, P < 0.001) 3–6 months after eye examination (Table 3 and Figure 1). Like the cataract surgery cohort, the eye examination cohort with baseline HbA1c ≥8.0% had a larger reduction in HbA1c (9.23% to 8.45%, P < 0.001). However, HbA1c change by age differed between the surgical and eye-examination cohorts. In the eye examination cohort, patients <71 years of age had a significant reduction in HbA1c 3–6 months after eye examination (7.84% to 7.49%, P < 0.001) but there was no significant HbA1c change in older patients.
 |
Table 3 Change in HbA1c† 3–6 Months After Eye Examination |
Determination of Change in Diabetic Management
Lastly, we reviewed the medical records of the cataract surgery and eye examination subjects to assess for changes in DM management. In the cataract surgery cohort, 311 subjects (72%) received DM care at the MVAHCS, and 104 of these subjects (33%) had a documented change in diabetic management. In the eye examination cohort, 310 subjects (72%) received DM care at the MVAHCS, and 122 of these subjects (39%) had a documented change in diabetic management. In both cohorts, significant mean HbA1c reduction occurred in subjects with diabetic management change(s) (Table 4). Patients with no change in DM management had lower mean baseline HbA1c, and in these patients we found a small increase in HbA1c at 3–6 months in the surgery group (7.13% to 7.35%, P = 0.006) that did not reach significance after Holm-Bonferroni correction and no significant change in HbA1c in the eye examination group (7.08% to 7.10%, P = 0.58).
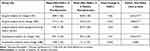 |
Table 4 Change in HbA1c† 3–6 Months After Cataract Surgery or Eye Examination in Subjects with and without Changes in Diabetic Management |
Discussion
Our study found improved HbA1c after cataract surgery, with significant HbA1c reductions 3–6 months after surgery in older subjects and those with higher pre-operative HbA1c values. Additionally, we found significant HbA1c reduction 2 years after cataract surgery in those with higher pre-operative HbA1c values. No subgroup in our study had significantly increased HbA1c, suggesting that cataract surgery will not thwart previously well-controlled DM. While it is critical to appropriately manage certain ophthalmic sequelae of DM such as iris/angle neovascularization, macular edema, or retinopathy prior to cataract surgery and to discuss the slightly higher operative complication rates in patients with DM,18 elevated HbA1c alone is not a contraindication to pursuing cataract surgery, and in fact, our findings support the idea that cataract surgery may be associated with improved glycemic control.
However, while surgical subjects experienced an overall improvement in both BCVA and HbA1c, we did not find a correlation between the two variables. This finding suggests that either vision improvement is not directly related to improved HbA1c or our BCVA analysis incompletely assesses visual function.19 A prior study found that cataract surgery is associated with improved quality of life,20 and other studies have shown that improved quality of life is associated with better glycemic control.21–24 These associations may explain the relationship between improved visual function and improved glycemic control; however, additional studies that more completely assess pre- and post-operative visual function beyond BCVA and determine the potential relationship between visual function and HbA1c after cataract surgery would be needed to support or refute this hypothesis.
In contrast to the two previously published studies evaluating HbA1c after cataract surgery,7,8 our study also examined a non-surgical, eye examination group. The non-surgical group also experienced reduction in HbA1c 3–6 months after ophthalmic care. Our 2015–2019 study period overlaps the 2015–2018 time frame when national trends showed population-based increases in HbA1c,4 so the HbA1c reduction in both surgical and eye examination groups in our study contrasts with national HbA1c trends.
One possible explanation for our data conflicting with national trends is that patients with DM who are seeing an ophthalmologist with a recently drawn HbA1c are more likely to be managed by a multidisciplinary care team. Our study’s finding of the greatest HbA1c reduction in patients who participated in an initial consultation with a dietician, diabetes case manager, or physician related to DM care, with equivalent HbA1c reductions in surgical and non-surgical groups, supports the importance of such a multidisciplinary approach. Perhaps, differences in multidisciplinary care account for our study showing postoperative HbA1c improvement, a finding consistent with the study conducted by Bar-Oz et al7 and discordant with the study performed by Ayaki et al.8
Another possible explanation for overall improvement in HbA1c in our surgical and eye examination cohorts is that patients may be motivated to better control other aspects of their health after taking action to improve their sight. Future prospective studies exploring whether improved connection with a multidisciplinary care team, improved quality of life, and/or improved visual function after interacting with ophthalmologists leads to HbA1c improvement may be instructive.
Study limitations include the male predominance and integrated health-care system utilization of our study population, which may limit generalizability of our study results. However, these features are consistent with the United States Veteran population undergoing cataract surgery.25 Additionally, a limitation inherent in the retrospective study design is that only subjects with HbA1c measurements at designated times were included in the study: we did not assess HbA1c in diabetic patients undergoing cataract surgery who did not have both pre-operative and 3–6 month post-operative HbA1c measurements, and our 2-year post-operative assessment was limited by attrition. However, one advantage of our retrospective study is that it provides real-world assessment of HbA1c change in the setting of cataract surgery, with less potential for Hawthorne effect-related bias.26
Conclusion
In conclusion, our study found the largest reductions in HbA1c when subjects received surgical and non-surgical ophthalmic care as part of a multidisciplinary care team. These findings add new evidence supporting the value of ophthalmology in DM care: in addition to preventing systemic disease from affecting sight, timely surgical and non-surgical ophthalmic care, incorporated with multidisciplinary diabetic care, may also facilitate better systemic disease control.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This work was supported using resources and facilities at the Minneapolis Veterans Affairs Health Care System and the VA Informatics and Computing Infrastructure (VINCI), VA HSR RES 13-457. Neither the Minneapolis Veterans Affairs Health Care System nor VINCI had any role in the design or conduct of this research. The contents of this manuscript do not represent the views of the US Department of Veterans Affairs or the United States Government.
This work was presented in part at the Association for Research in Vision and Ophthalmology Annual Meeting, May 1–7, 2021, as a virtual poster presentation. The poster’s abstract was published in ‘Poster Abstracts’ in Investigative Ophthalmology & Visual Science. Christopher Santilli, Jared Murray, Karen R Armbrust; Change in Hemoglobin A1c Levels After Cataract Surgery. Invest. Ophthalmol. Vis. Sci. 2021;62(8):1123. [https://iovs.arvojournals.org/article.aspx?articleid=2773282]
Disclosure
The authors report no conflicts of interest in this work.
References
1. Federal Practitioner. Federal health care data trends 2017. Diabetes Mellitus; 2017. Available from: https://www.fedprac-digital.com/federalpractitioner/data_trends_2017?pg=20#pg20.
2. Kiziltoprak H, Tekin K, Inanc M, Goker YS. Cataract in diabetes mellitus. World J Diabetes. 2019;10(3):140–153. doi:10.4239/wjd.v10.i3.140
3. Kelkar A, Kelkar J, Mehta H, Amoaku W. Cataract surgery in diabetes mellitus: a systematic review. Indian J Ophthalmol. 2018;66(10):1401–1410. PMID: 30249823; PMCID: PMC6173035. doi:10.4103/ijo.IJO_1158_17
4. Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999–2018. NEJM. 2021;384(23):2219–2228. doi:10.1056/NEJMsa2032271
5. Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment, and eye disease. Eye. 2018;32:1296–1303. doi:10.1038/s41433-018-0081-8
6. Gray CS, Karimova G, Hildreth AJ, Crabtree L, Allen D, O’connell JE. Recovery of visual and functional disability following cataract surgery in older people: Sunderland cataract study. J Cataract Refract Surg. 2006;32(1):60–66. PMID: 16516780. doi:10.1016/j.jcrs.2005.07.040
7. Bar-Oz D, Hecht I, Achiron A, et al. Glycemic control and quality of life following cataract surgery in patients with type 2 diabetes and without maculopathy. Curr Eye Res. 2018;43(1):96–101. doi:10.1080/02713683.2017.1383443
8. Ayaki M, Negishi K, Tsubota K. Rejuvenation effects of cataract surgery with ultraviolet blocking intra-ocular lens on circadian rhythm and gait speed. Rejuvenation Res. 2014;17(4):359–365. doi:10.1089/rej.2014.1550
9. U.S. Department of Veterans Affairs. VA Informatics and Computing Infrastructure (VINCI), VA HSR RES 13-457, U.S. Department of Veterans Affairs. U.S. Department of Veterans Affairs; 2008. Available from: https://vaww.VINCI.med.va.gov.
10. US Department of Veterans Affairs. 172VA10P2: VHA corporate data warehouse – VA. 79 FR 4377; 2021.
11. Chen G, Khan N, Walker R, Quan H. Validating ICD coding algorithms for diabetes mellitus from administrative data. Diabetes Res Clin Pract. 2010;89(2):189–195. doi:10.1016/j.diabres.2010.03.007
12. Dexamethasone Ozurdex, Allergan Inc. Clinical review report: indication: for the treatment of adult patients with diabetic macular edema who are pseudophakic. Appendix 5, Validity of Outcome Measures. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539248/.
13. Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006;47(3):1236–1240. doi:10.1167/iovs.05-0981
14. Klobucar T, Hibbs R, Jans P, Adams M. Evaluating the effectiveness of an aggressive case management and home telehealth monitoring program for long-term control of A1C. Prof Case Manag. 2012;17(2):51–58. doi:10.1097/NCM.0b013e31823ba3cb
15. Franz M, Macleod J, Evert A, et al. Academy of nutrition and dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet. 2017;117(10):1659–1679. doi:10.1016/j.jand.2017.03.022
16. Alli C, Daguio M, Kosciuk M, Middelhoff C, Wyrick K, Kerns W. Does case management improve diabetes outcomes? J Fam Pract. 2008;57(11):747–748.
17. American Diabetes Association. Standards of medical care in diabetes-2008. Diabet Care. 2008;31(suppi1):S12–S54. doi:10.2337/dc08-S012
18. Grzybowski A, Kanclerz P, Huerva V, Ascaso FJ, Tuuminen R. Diabetes and phacoemulsification cataract surgery: difficulties, risks and potential complications. J Clin Med. 2019;8(5):716. doi:10.3390/jcm8050716
19. Laitinen A, Koskinen S, Härkänen T, Reunanen A, Laatikainen L, Aromaa A. A nationwide population-based survey on visual acuity, near vision, and self-reported visual function in the adult population in Finland. Ophthalmology. 2005;112(12):2227–2237. doi:10.1016/j.ophtha.2005.09.010
20. Oleś M, Oleś P. Quality of life before and after cataract surgery: research in a sample of polish patients. Appl Res Qual Life. 2012;7:93–108. doi:10.1007/s11482-011-9139-5
21. Jolly M, Sequeira W, Block J. Health and quality of life outcomes. Health Qual Life Outcomes. 2014;12:173. doi:10.1186/s12955-014-0173-5
22. Engstrom M, Leksell J, Johansson U, et al. Health-related quality of life and glycaemic control among adults with type 1 and type 2 diabetes – a nationwide cross-sectional study. Health Qual Life Outcomes. 2019;17:141. doi:10.1186/s12955-019-1212-z
23. Shim Y, Lee J, Toh M, Tang W, Ko Y. Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in Singapore. Diabet Med. 2012;29(8):e241–8. doi:10.1111/j.1464-5491.2012.03689.x
24. Lau C, Qureshi K, Scott S. Association between glycaemic control and quality of life in diabetes mellitus. J Postgrad Med. 2004;50(3):189–193.
25. Wu AM, Wu CM, Tseng VL, et al. Characteristics associated with receiving cataract surgery in the US Medicare and Veterans Health Administration populations. JAMA Ophthalmol. 2018;136(7):738–745. PMID: 29800973; PMCID: PMC6136038. doi:10.1001/jamaophthalmol.2018.1361
26. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi:10.1016/j.jclinepi.2013.08.015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
