Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Gender Differences in Psychiatric Symptoms and the Social Functioning of 610 Patients with Schizophrenia in Urban China: A 10-Year Follow-Up Study
Authors Zhao J, Diao J, Li X, Yang Y, Yao Y , Shi S , Yuan X, Liu H, Zhang K
Received 9 May 2022
Accepted for publication 21 July 2022
Published 27 July 2022 Volume 2022:18 Pages 1545—1551
DOI https://doi.org/10.2147/NDT.S373923
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Jintao Zhao,1,2,* Jian Diao,1,2,* Xiaoyue Li,1,2,* Yating Yang,1,2 Yitan Yao,1,2 Shengya Shi,1,2 Xiaoping Yuan,1,2 Huanzhong Liu,1,2 Kai Zhang1,2
1Department of Psychiatry, Chaohu Hospital of Anhui Medical University, Hefei, People’s Republic of China; 2Anhui Psychiatric Center, Anhui Medical University, Hefei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kai Zhang; Huanzhong Liu, Department of Psychiatry, Chaohu Hospital of Anhui Medical University, No. 64 North Chaohu Road, Chaohu City, Hefei, 238000, People’s Republic of China, Email [email protected]; [email protected]
Purpose: To explore the different outcomes between male and female patients with schizophrenia after long-term follow-up.
Patients and Methods: Schizophrenia patients were participants in our study. First, two senior psychiatrists collected data on the demographic characteristics and clinical symptoms of patients from the Hospital Information System between February 2009 and January 2010. Second, two other senior psychiatrists called the patients and their guardians between February 2019 and January 2020 to get general information on the patients and assess their psychiatric symptoms and social functioning using the Positive and Negative Syndrome Scale (PANSS) and the Personal and Social Performance (PSP) scale.
Results: Of the 610 participants, the 306 female participants were younger (48.32 ± 12.99 vs 49.84 ± 12.60) and had received more education (8.08 ± 3.76 vs 7.94 ± 3 0.73). After 10 years, women were found to have more outpatient visits than men (20.86 ± 22.21 vs 16.11 ± 16.87, P < 0.05). However, there was no significant gender difference in number of hospitalizations (3.12 ± 5.34 vs 2.77 ± 5.84, P > 0.05). The PANSS scores were lower for both groups at the 10-year follow-up. Women had significantly lower scores than men after the 10-year period (P < 0.05). With regard to social functioning, there was a significant difference in social functioning between baseline scores and 10-year follow-up scores indicating an improvement in social functioning. PSP scores had significantly increased in women (P < 0.01) but not in men (P > 0.05).
Conclusion: Female patients had significantly lower levels of psychiatric symptoms and higher levels of social functioning at 10-year follow-up than male patients. They also reported more outpatient visits, which may have contributed to the gender differences in outcomes. Family members and doctors of patients should urge patients to make regular outpatient visits for better outcomes after hospitalization.
Keywords: mental illness, psychiatry, health outcomes, neuropsychiatric
Introduction
Schizophrenia is a common, serious, and chronic psychiatric disorder. The prevalence of schizophrenia is 0.7% in China, which means that more than 9.8 million Chinese people suffer from schizophrenia.1 Patients with schizophrenia generally have three types of symptoms: positive, negative, and cognitive. Compared with positive and negative symptoms, cognitive symptoms have been receiving increased research attention.2–4 Cognitive impairment in schizophrenia involves a broad array of social and nonsocial cognitive domains.5 Previous studies have shown that impairment of social cognitive capacity of patients with schizophrenia induces poor social skills resulting in impaired social functioning.6–9 Impairment in social functioning is commonly observed and is a major adverse outcome for patients and public health. Consequently, improving and preserving functioning is an important long-term treatment goal for better prognosis, recovery, and community adjustment.
In addition to social functioning, gender differences in people with schizophrenia are another important issue that has received research attention.10–12 Studies that focus on gender differences are important for understanding the biological, psychological, and sociological processes of schizophrenia, and provide clues for precise treatment of male and female patients.13,14 For example, gender differences in clinical presentation, psychosocial functioning, and course of illness have been widely observed in patients with schizophrenia.15–18
Some studies indicate that female patients have a more favorable prognosis than male patients, including fewer hospital readmissions, fewer negative symptoms, and less disability.19–21 In contrast, male patients with schizophrenia have been found to have significantly higher levels of positive symptoms and slightly lower levels of functioning.22 Beyond symptoms, personal and social functioning are important outcomes for patients with schizophrenia. Evidence from a 2-year follow-up study indicated that men displayed poorer working capacity and functional ability than women with the disease.23 Men experience more negative symptoms, which are particularly harmful to their role in society. However, long-term differences in outcomes, such as social functioning, positive symptoms, and negative symptoms, between male and female patients with schizophrenia living in urban areas are not clear. Therefore, this study included a large sample of patients with schizophrenia in an urban district of China to explore the different outcomes between male and female patients with schizophrenia after long-term follow-up.
Materials and Methods
Participants
Patients with schizophrenia who met the ICD-10 diagnostic criteria were participants in our study. All patients had been hospitalized during the period between February 2009 and January 2010 at Chaohu Hospital of Anhui Medical University in the Department of Psychiatry. Patients who met the following criteria were excluded from the study: (1) diagnosed with a serious physical illness, (2) a history of alcohol or drug addiction, (3) unable to understand and sign the informed consent form, and (4) discontinued psychiatric drug treatment at follow-up.
Figure 1 shows the procedure of our study. First, two senior psychiatrists collected data on the demographic characteristics and clinical symptoms of patients from the Hospital Information System of Chaohu Hospital who had been hospitalized between February 2009 and January 2010. Second, two other senior psychiatrists called the patients and their guardians between February 2019 and January 2020 to get general information on the patients and assess their psychiatric symptoms and social functioning.
 |
Figure 1 Flow chart of our study. |
This study was approved by the Human Research and Ethics Committee of Chaohu Hospital of Anhui Medical University (Approval No. 201902-kyxm-03), and all study procedures were performed in accordance with the Declaration of Helsinki. Participants in the study and their guardians were informed about the purpose of the study by telephone, and oral informed consent was obtained from them. The verbal informed consent from the participants was approved by the Human Research and Ethics Committee of Chaohu Hospital of Anhui Medical University.
Measurement
Two senior psychiatrists measured the psychiatric symptoms of patients using the Positive and Negative Syndrome Scale (PANSS) by phone.24,25 Repeated assessments of the PANSS total score showed that an inter-rater correlation coefficient greater than 0.8 was maintained. According to previous studies, we assessed the social functioning of patients with the Personal and Social Performance (PSP) scale.26–28 The PSP scale is a widely used clinician-reported measurement to assess personal and social functioning of patients with schizophrenia. The PSP scale provides quantitative measures of patient functioning that are separate from disease-specific symptoms. In a previous study, the Chinese version of the PSP scale demonstrated adequate reliability and validity for the measurement of social functioning.26
Statistical Analysis
Statistical analysis was conducted using SPSS 23.0. Demographic continuous variables such as age, level of education, and duration of disease were expressed as mean ± standard deviation. Normally distributed data were tested for differences with Student’s t-test, and categorical data were analyzed with Pearson’s chi square test. Non-normally distributed data, such as number of hospitalizations and outpatient visits, were tested for gender differences with the Mann–Whitney U-test. Psychiatric symptoms and social functioning of the male and female patients were analyzed using a two-way analysis of variance. The time points were 0 year and 10 years. All tests were two-tailed with a significance level at 0.05.
Results
Demographic Characteristics of the Participants
From February 2009 to January 2010, a total of 823 patients with schizophrenia were hospitalized at Chaohu Hospital of Anhui Medical University in the Department of Psychiatry.
Of the 823 patients at baseline in 2009–2010, 213 were not included in the study in 2019–2020 as they were not able to follow-up with the patient or for other reasons (see Figure 1). Therefore, the final sample included 610 patients (74.12%) who participated in the study. All enrolled patients had no suicide behavior in our study. Informants were available for all participants (100%).
Table 1 shows the demographic characteristics of the participants. Of the 610 participants, 304 were male and 306 were female. The female participants were younger (48.32 ± 12.99 vs 49.84 ± 12.60) and had received more education (8.08 ± 3.76 vs 7.94 ±3 0.73, P > 0.05) (Table 1). There were no significant differences in duration of disease, marital status, employment, monthly income of family, and mean chlorpromazine equivalent daily (all P values were >0.05) (Table 1).
 |
Table 1 General Demographic Characteristics of All Patients with Schizophrenia |
Hospitalizations and Outpatient Visits Over the 10-Year Period
After 10 years, women were found to have more outpatient visits (total number) than men (20.86 ± 22.21 vs 16.11 ± 16.87, P < 0.05) (Table 1). However, there was no significant gender difference in number of hospitalizations (3.12 ± 5.34 vs 2.77 ± 5.84, P > 0.05) (Table 2).
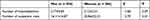 |
Table 2 Number of Hospitalizations and Outpatient Visits Between Male and Female Patients with Schizophrenia |
Psychiatric Symptoms and Social Functioning at Baseline and Follow-Up
Table 3 shows the results on the gender differences in psychiatric symptoms and social functioning at baseline and follow-up. There was a significant time effect for psychiatric symptoms based on the PANSS total scores for the two groups. The scores were lower for both groups at the 10-year follow-up. However, there was a significant time × gender interaction among the PANSS total scores. Women had significantly lower scores than men after the 10-year period (P < 0.05). With regard to social functioning, there was a significant difference in social functioning between baseline scores and 10-year follow-up scores indicating an improvement in social functioning. However, there was a significant time × gender interaction among the PSP total scores. PSP scores had significantly increased in women (P < 0.01) but not in men (P > 0.05).
 |
Table 3 Psychiatric Symptoms and Social Function of Male and Female Patients with Schizophrenics at Baseline and Follow-Up |
Discussion
In this study, we organized one large-size longitudinal study to detect the outcomes in psychiatric symptoms and social functioning of patients with schizophrenia in urban China after a 10-year period. We also investigated gender differences in these outcomes. We found that female patients with schizophrenia reported better social functioning and less psychiatric symptoms than male patients. In addition, women reported more outpatient visits than men, while men had more hospitalizations than women. The results of this study suggest that it is beneficial for patients’ rehabilitation and social functioning for their family members and doctors to urge patients to make regular outpatient visits.
Patients’ long-term outcomes are always an important issue for patients, relatives, and psychiatrists.29,30 Treatment guidelines recommend medication throughout the course of the disease to achieve good recovery.31 However, does long-term psychopharmacological treatment eliminate or reduce psychosis in patients with schizophrenia? Harrow et al found that more than 70% of patients who had been continuously prescribed antipsychotic medication experienced psychotic symptoms at follow-up assessments over a 20-year period.32 Furthermore, patients who had not been prescribed antipsychotic medication showed significantly less psychotic activity than those who had been prescribed antipsychotics. The findings of several other articles were consistent with this view.33,34 These results debate the current mainstream view that emphasizes long-term maintenance treatment with antipsychotic medication in patients with schizophrenia.35–37 In our study, long-term treatment with antipsychotic medication down-regulated psychotic symptoms; psychiatric symptoms improved in both male and female participants. We thought that drug maintenance treatment is better for patients to recovery from psychosis. Consistent with our results, Ran’s 14-year follow-up study showed that outcomes for the untreated group were worse.38 In addition, we found that psychiatric symptoms improved more so in women than in men, but the difference was not statistically significant. This result may be related to the higher number of outpatient visits in female patients. We will pay more attention to this issue in future studies.
Social functioning is another outcome of importance to patients’ recovery long-term. Does long-term psychopharmacological treatment contribute to social functioning in patients with schizophrenia? Harrow et al performed a 15-year follow-up study that focused on this issue.39 In their study, they found that a larger percentage of patients who were not taking antipsychotic medication showed periods of recovery and better global functioning. They suggested that not all patients with schizophrenia need to be treated with antipsychotic medication long-term. However, the social functioning of the participants in our study improved after 10 years of psychopharmacological treatment. There was a significant difference between baseline and 10-year follow-up. However, female patients showed better social functioning than male patients. We believe this difference may also be due to women with schizophrenia having more outpatient visits. Previous research can offer different perspectives. Galderisi et al examined gender differences in social functioning in a cross-sectional study and found there were no gender differences.40 Consistent with their study, our study also did not find significant gender differences at baseline. However, over time, gender differences in social functioning emerged. Consistent with our results, Ran’s another study showed that the long-term outcomes of male schizophrenia patients are worse than those of female patients in rural China.41 Other than psychopharmacological treatment, do we have any other type of treatment to improve impairment of social functioning in patients with schizophrenia? Research suggests that family interventions may be effective in this regard. Lenior et al showed that standard treatment (antipsychotic medication) plus family intervention significantly improved patients’ social functioning when compared with receiving standard treatment alone.40 Social skills training is another evidence-based treatment that can improve social functioning. Conversation and assertive skills training have been shown to significantly improve the social skills of patients with schizophrenia.42,43
There are limitations to our study that should be noted. First, there was only one follow-up assessment. With more follow-up assessments, there would be more comparative information about outcomes over time. In future research, we will design a study that includes more follow-up times. Second, we did not collect patients’ information on changes in antipsychotic medications during the 10-year period. Third, we did not know whether those who could not be reached at follow-up were doing badly or not. Fourth, we did not measure patients’ adverse effect during ten years.
Conclusions
In conclusion, gender differences were found among urban Chinese patients with schizophrenia. Female patients had significantly lower levels of psychiatric symptoms and higher levels of social functioning at 10-year follow-up than male patients. They also reported more outpatient visits, which may have contributed to the gender differences in outcomes. Family members and doctors of patients with schizophrenia should urge patients to make regular outpatient visits for better outcomes after hospitalization, such as a decrease in psychiatric symptoms and improved social functioning.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, Kai Zhang, upon reasonable request.
Acknowledgments
We thank all of participants who volunteered to participate in the study. Thanks to Chaohu Hospital of Anhui Medical University and corresponding authors for their support. This study was supported by the National Natural Science Foundation of China (81801341), the Anhui Provincial Key R&D Programme (202004j07020030), the China International Medical Exchange Foundation (Z-2018-35-2002). The funding body did not participate in the design, conduct, or writing of the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Huang Y, Wang YU, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi:10.1016/S2215-0366(18)30511-X
2. Tripathi A, Kar SK, Shukla R. Cognitive deficits in schizophrenia: understanding the biological correlates and remediation strategies. Clin Psychopharmacol Neurosci. 2018;16(1):7–17. doi:10.9758/cpn.2018.16.1.7
3. Strassnig M, Bowie C, Pinkham AE, et al. Which levels of cognitive impairments and negative symptoms are related to functional deficits in schizophrenia? J Psychiatr Res. 2018;104:124–129. doi:10.1016/j.jpsychires.2018.06.018
4. Carruthers SP, Van Rheenen TE, Gurvich C, et al. Characterising the structure of cognitive heterogeneity in schizophrenia spectrum disorders. A systematic review and narrative synthesis. Neurosci Biobehav Rev. 2019;107:252–278. doi:10.1016/j.neubiorev.2019.09.006
5. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. 2019;18(2):146–161. doi:10.1002/wps.20624
6. Adery LH, Ichinose M, Torregrossa LJ, et al. The acceptability and feasibility of a novel virtual reality based social skills training game for schizophrenia: preliminary findings. Psychiatry Res. 2018;270:496–502. doi:10.1016/j.psychres.2018.10.014
7. Inchausti F, García-Poveda NV, Ballesteros-Prados A, et al. The effects of metacognition-oriented social skills training on psychosocial outcome in schizophrenia-spectrum disorders: a randomized controlled trial. Schizophr Bull. 2018;44(6):1235–1244. doi:10.1093/schbul/sbx168
8. Turner DT, McGlanaghy E, Cuijpers P, et al. A meta-analysis of social skills training and related interventions for psychosis. Schizophr Bull. 2018;44(3):475–491. doi:10.1093/schbul/sbx146
9. Granholm E, Holden J, Worley M. Improvement in negative symptoms and functioning in cognitive-behavioral social skills training for schizophrenia: mediation by defeatist performance attitudes and asocial beliefs. Schizophr Bull. 2018;44(3):653–661. doi:10.1093/schbul/sbx099
10. Navarra-Ventura G, Fernandez-Gonzalo S, Turon M, et al. Gender differences in social cognition: a cross-sectional pilot study of recently diagnosed patients with schizophrenia and healthy subjects. Can J Psychiatry. 2018;63(8):538–546. doi:10.1177/0706743717746661
11. Šimunović Filipčić I, Ivezić E, Jakšić N, et al. Gender differences in early onset of chronic physical multimorbidities in schizophrenia spectrum disorder: do women suffer more? Early Interv Psychiatry. 2020;14(4):418–427.
12. Seeman MV. Does gender influence outcome in schizophrenia? Psychiatr Q. 2019;90(1):173–184. doi:10.1007/s11126-018-9619-y
13. Riecher-Rössler A, Butler S, Kulkarni J. Sex and gender differences in schizophrenic psychoses - a critical review. Arch Womens Ment Health. 2018;21(6):627–648. doi:10.1007/s00737-018-0847-9
14. Brand BA, de Boer JN, Dazzan P, et al. Towards better care for women with schizophrenia-spectrum disorders. Lancet Psychiatry. 2022;9(4):330–336. doi:10.1016/S2215-0366(21)00383-7
15. Seeman MV. Women who suffer from schizophrenia: critical issues. World J Psychiatry. 2018;8(5):125–136. doi:10.5498/wjp.v8.i5.125
16. Brand BA, Haveman YRA, De Beer F, et al. Antipsychotic medication for women with schizophrenia spectrum disorders. Psychol Med. 2021;52(4):1–15.
17. González-Rodríguez A, Guàrdia A, Álvarez Pedrero A, et al. Women with schizophrenia over the life span: health promotion, treatment and outcomes. Int J Environ Res Public Health. 2020;17(15):5594. doi:10.3390/ijerph17155594
18. Li AWY, Hui CLM, Lee EHM, et al. Gender differences in correlates of cognition in first-episode psychosis. Psychiatry Res. 2019;271:412–420. doi:10.1016/j.psychres.2018.12.011
19. Thorup A, Albert N, Bertelsen M, et al. Gender differences in first-episode psychosis at 5-year follow-up–two different courses of disease? Results from the OPUS study at 5-year follow-up. Eur Psychiatry. 2014;29(1):44–51. doi:10.1016/j.eurpsy.2012.11.005
20. Grossman LS, Harrow M, Rosen C, et al. Sex differences in outcome and recovery for schizophrenia and other psychotic and nonpsychotic disorders. Psychiatr Serv. 2006;57(6):844–850. doi:10.1176/ps.2006.57.6.844
21. Rotstein A, Shadmi E, Roe D, et al. Gender differences in quality of life and the course of schizophrenia: national study. BrJ Psych Open. 2022;8(2):e35. doi:10.1192/bjo.2022.3
22. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49(6):523–529. doi:10.1016/j.comppsych.2008.03.004
23. Usall J, Ochoa S, Araya S, et al. Gender differences and outcome in schizophrenia: a 2-year follow-up study in a large community sample. Eur Psychiatry. 2003;18(6):282–284. doi:10.1016/j.eurpsy.2003.06.001
24. Yang Y, Ning X, Wang X, et al. Triglyceride/glucose index is a reliable predictor of insulin resistance in schizophrenia. Schizophr Res. 2020;223:366–367. doi:10.1016/j.schres.2020.07.005
25. Yuan X, Wang S, Shi Y, et al. Pro-inflammatory cytokine levels are elevated in female patients with schizophrenia treated with clozapine. Psychopharmacology. 2022;239(3):765–771. doi:10.1007/s00213-022-06067-y
26. Chiu EC, Hung TM, Huang CM, et al. Responsiveness of the personal and social performance scale in patients with schizophrenia. Psychiatry Res. 2018;260:338–342. doi:10.1016/j.psychres.2017.11.053
27. Das S, Punnoose VP, Doval N, et al. Spirituality, religiousness and coping in patients with schizophrenia: a cross sectional study in a tertiary care hospital. Psychiatry Res. 2018;265:238–243. doi:10.1016/j.psychres.2018.04.030
28. Gonzalez-Blanco L, Garcia-Portilla MP, Dal Santo F, et al. Predicting real-world functioning in outpatients with schizophrenia: role of inflammation and psychopathology. Psychiatry Res. 2019;280:112509. doi:10.1016/j.psychres.2019.112509
29. Strauss GP, Harrow M, Grossman LS, et al. Periods of recovery in deficit syndrome schizophrenia: a 20-year multi-follow-up longitudinal study. Schizophr Bull. 2010;36(4):788–799. doi:10.1093/schbul/sbn167
30. Newman SC, Bland RC, Thompson AH. Long-term course and outcome in schizophrenia: a 34-year follow-up study in Alberta, Canada. Psychol Med. 2012;42(10):2137–2143. doi:10.1017/S0033291712000177
31. Shimomura Y, Kikuchi Y, Suzuki T, et al. Antipsychotic treatment in the maintenance phase of schizophrenia: an updated systematic review of the guidelines and algorithms. Schizophr Res. 2020;215:8–16. doi:10.1016/j.schres.2019.09.013
32. Harrow M, Jobe TH, Faull RN. Does treatment of schizophrenia with antipsychotic medications eliminate or reduce psychosis? A 20-year multi-follow-up study. Psychol Med. 2014;44(14):3007–3016. doi:10.1017/S0033291714000610
33. Harrow M, Jobe TH, Tong L. Twenty-year effects of antipsychotics in schizophrenia and affective psychotic disorders. Psychol Med. 2021;2021:1–11.
34. Harrow M, Jobe TH, Faull RN. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol Med. 2012;42(10):2145–2155. doi:10.1017/S0033291712000220
35. Goff DC, Falkai P, Fleischhacker WW, et al. The long-term effects of antipsychotic medication on clinical course in schizophrenia. Am J Psychiatry. 2017;174(9):840–849. doi:10.1176/appi.ajp.2017.16091016
36. Harrow M, Jobe TH, Tong L. Long-term effectiveness of antipsychotics. Psychol Med. 2021;2021:1–5.
37. Pierre JM, Zito MF, Yang YS, et al. Antipsychotic discontinuation and recovery: chicken or egg? Psychol Med;2021. 1–2. doi:10.1017/S0033291721001872
38. Ran MS, Weng X, Chan CLW, et al. Different outcomes of never-treated and treated patients with schizophrenia: 14-year follow-up study in rural China. Br J Psychiatry. 2015;207(6):495–500. doi:10.1192/bjp.bp.114.157685
39. Harrow M, Jobe TH. Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study. J Nerv Ment Dis. 2007;195(5):406–414. doi:10.1097/01.nmd.0000253783.32338.6e
40. Galderisi S, Bucci P, Üçok A, et al. No gender differences in social outcome in patients suffering from schizophrenia. Eur Psychiatry. 2012;27(6):406–408. doi:10.1016/j.eurpsy.2011.01.011
41. Ran MS, Mao WJ, Chan CLW, et al. Gender differences in outcomes in people with schizophrenia in rural China: 14-year follow-up study. Br J Psychiatry. 2015;206(4):283–288. doi:10.1192/bjp.bp.113.139733
42. Lenior ME, Dingemans PMAJ, Linszen DH, et al. Social functioning and the course of early-onset schizophrenia: five-year follow-up of a psychosocial intervention. Br J Psychiatry. 2001;179(1):53–58. doi:10.1192/bjp.179.1.53
43. Chien HC, Ku CH, Lu RB, et al. Effects of social skills training on improving social skills of patients with schizophrenia. Arch Psychiatr Nurs. 2003;17(5):228–236. doi:10.1016/S0883-9417(03)00095-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
