Back to Journals » Research and Reports in Tropical Medicine » Volume 14
From Neglected to Public Health Burden: Factors Associated with Podoconiosis in Resource Limited Setting in Case of Southwest Ethiopia: A Community Based Cross Sectional Study
Authors Debele GR , Shifera E, Dessie YL, Jaleta DD , Borena MU , Kanfe SG , Nigussie K , Ayana GM , Raru TB
Received 29 March 2023
Accepted for publication 8 July 2023
Published 12 July 2023 Volume 2023:14 Pages 49—60
DOI https://doi.org/10.2147/RRTM.S412624
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mario Rodriguez-Perez
Gebiso Roba Debele,1 Eyasu Shifera,1 Yohannes Lulu Dessie,2 Debela Dereje Jaleta,2 Megersso Urgessa Borena,3 Shuma Gosha Kanfe,4 Kabtamu Nigussie,5 Galana Mamo Ayana,5 Temam Beshir Raru5
1Department of Public Health, College of Health Sciences, Mattu University, Mattu, Ethiopia; 2Department of Nursing, College of Health Sciences, Mattu University, Mattu, Ethiopia; 3Department of Public Health, School of Health Sciences, Shashemene Campus, Madda University, Shashemene, Ethiopia; 4Department of Health Informatics, College of Health Sciences, Mattu University, Mattu, Ethiopia; 5College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Gebiso Roba Debele, Email [email protected]
Background: Even though podoconiosis can cause physical, financial, and social impairments, it is commonly overlooked by organizations, and one-fourth of the predicted worldwide burden will fall on Ethiopia. In spite of this, there are only a few attempts for prevention and control in certain areas in Ethiopia. Updated statistics on prevalence and contributing factors could make local efforts at prevention, control, and rehabilitation more effective. Thus, this study was aimed to assess the prevalence of podoconiosis and its associated factors among Ilu Aba Bor zone residents, South West Ethiopia.
Methods: A community-based cross-sectional study was conducted on 491 participants from March 25 to April 25, 2022. Data were entered into Epi-Data version 4.6.0, then exported to SPSS version 25 for final analysis. In the bi-variable regression, variables with P-values less than 0.25 were included in the multivariable model. Finally, multivariable logistic regression was performed to identify factors associated with podoconiosis at a 5% level of significance.
Results: In this study area, podoconiosis prevalence was found to be 5.7% [3.6– 7.2]. In multivariable regression model, lower tertile wealth status [AOR=2.09; (95% CI (1.384, 5.343)], no formal education [AOR=2.23; (95% CI; 1.179– 3.820)] and average distance to reach water source to home [AOR=2.061; (95% CI: 1.78– 7.35)] were significantly associated podoconiosis.
Conclusion and Recommendation: According to this study, one in every seventeen individuals had podoconiosis, which is a significant prevalence when compared to earlier studies. Podoconiosis was observed to be associated with factors like wealth status, educational attainment, and distance from water source. To address this public health issue, strong preventive and therapeutic treatments should be used.
Keywords: prevalence, factors, podoconiosis, Ilu Aba Bor zone
Introduction
Podoconiosis is a non-infectious, chronic, progressive, debilitating, and disfiguring disease that only affects the lower limbs.1 While the exact causes are unknown, current data points to prolonged exposure to red clay soil with volcanic origin as the disease’s primary cause.2 Podoconiosis typically appears with bilateral and asymmetric swelling on the lower limbs with rare groin involvement, in contrast to the chronic edema, which presents differently to podoconiosis in the early stages.3
Evidence showed that one-sixth of the world’s population, mostly in developing countries, is infected with one or more of the NTD.4 Podoconiosis is thought to affect 4 million people worldwide, mostly in tropical regions of southeast Asia, Central and South America, and Africa.5 It is known or suspected to be endemic in 32 countries, including Ethiopia.6 According to estimates, 1 million Ethiopians have podoconiosis, which results in annual economic losses of more than US$ 200 million.7 Despite having a significant negative impact on the economy and causing chronic morbidity and disability,8–10 podoconiosis appears to be neglected and not seen as a public health problem in Ethiopia.
Podoconiosis is one of the diseases with the highest prevalence in Ethiopia and it is thought that 500,000 to 1 million people have the disease and 15 million people are at risk due to red-clay soil exposure.11 In Ethiopia, the percentage of cases was 4%; Oromia had the greatest incidence (4%) following the Southern Nations Nationality and People Region, which had an 8.1% prevalence.12 According to estimates, there are 1.56 million cases of podoconiosis across the country, and the condition was more common than 1% in 345 districts.13
The Mossy Foot Treatment and prevention Association (MFTPA) initiative, which includes preventive, treatment, and rehabilitation activities, has been in Wolaita zone of Ethiopia since 1998.14 This initiative was adopted and later launched by Debre Markos and East Gojam Zone, in June 2010.15 Moreover, Ethiopia developed a guideline for controlling and preventing NTD morbidity as well as preventing disability.16 Under the second Strategic Plan, morbidity management and disability prevention services of podoconiosis were offered in 150 of the 345 targeted woredas (44% performance). Its performance was deemed insufficient for achieving the 2020 goal of ensuring 70% regular shoe wear and proper foot hygiene practice in all endemic areas.17
Podoconiosis has a wide range of effects, including a significant financial and social burden; it is also linked to significant stigma at school, work, or the market; and it can prevent people from participating in social bonds like marriage.8,18 According to estimates, those who have podoconiosis lose an average of one month’s worth of Disability-adjusted life years (DALYs) per year as a result of sickness.19 In Ethiopia, there were 1.5 million cases in 2017, which translates to172073DALYs. The estimated yearly economic cost of podoconiosis in Ethiopia is US$213.2 million, with productivity costs accounting for 91.1% of the total cost. Each case carried an average financial burden of US$136.9.18
Other than the economic and societal effects, complications are the most common side effects of podoconiosis. They include inflammation that occurs at least once a year and may be made worse by a superinfection of bacteria, viruses, or fungi.20 As well, it was discovered that individuals with podoconiosis had significantly worse quality of life ratings in all domains.21 Additionally, it puts patients under social and psychological strain and threatens their ability to pursue education and work possibilities because it causes frequent acute attacks and stigmatization fears in them.22
Despite this catastrophic impact, it is mostly neglected by most of governmental and nongovernmental organizations, and Ethiopia’s efforts at prevention and control fall short when compared to areas where the disease is endemic.23 A better understanding of the prevalence and underlying factors might make local efforts at prevention, control, and rehabilitation more successful. However, there are currently little studies on the prevalence and factors of podoconiosis in Ethiopia. Thus, the current study assessed the prevalence and associated factors in a resource-limited setting in the case of Ilu Aba Bor Zone, Southwest Ethiopia.
Methods and Materials
Study Setting and Design
Community-based cross-sectional study was conducted from March 1 to April 28, 2022 in Ilu Aba Bor zone, which is found in Oromia Regional State, Southwest Ethiopia. Ilu Aba Bor zone is one of the administrative zones in South Western Ethiopia. The administrative centre of the zone is Mattu town. Total population of Ilu Aba Bor zone as to 2007 census was, 1,271,609, among which 50.1% (636,986) were males.24
Population and Eligibility Criteria
The source population for this study consisted of all residents of the Ilu Aba Bor zone who were 15 years of age or older. The study population for this investigation consisted of every person in the randomly chosen districts who met the inclusion requirements. The study included people who had lived in the study area for at least six months. Those who were ill throughout the study time and were unable to respond, speak, hear, or who had severe mental illness were excluded from the study.
Sample Size Determination and Sampling Procedure
First Objective
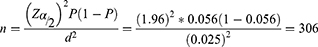
Sample size was determined using a single population proportion formula considering: 5.6% prevalence of Podoconiosis in Bedele Zuria woreda, Oromia regional state,25 at 95% confidence interval (CI), with 2.5% margin of error (d) and design effect of 1.5.
Where; n = Minimum sample size, Z = 1.96, Normal deviant at the portion of 95% confidence interval of two tailed test, P = 5.6% the prevalence of podoconiosis, d = margin of error acceptable is taken as 2.5%= 0.025. By adding 10% for non-response rate the final working sample was 505.
Second Objective
Using Epi-Data version 4.6.0, the sample size was calculated by selecting factors that have a significant association with Podoconiosis in prior studies,26–28 taking into account the assumption power of 80%, the marginal error of 5%, and the 95% CI. The sample size is displayed below after being multiplied by a 10% non-response rate (Table 1).
 |
Table 1 Sample Size Determination for Factors Associated with Podoconiosis from Previous Studies |
Where: P1: is the proportion of exposed with the outcome, P2: is the proportion of non-exposed with the outcome, Z α/2: is taking CI 95%, Zβ: 80% power and, the ratio of exposed to non-exposed is 1:1. Therefore, maximum sample size sample size was considered for the study which is 505 individuals from a randomly selected households based on the above parameters.
Sampling Techniques and Procedures
Three districts were randomly chosen by lottery out of the fourteen administrative districts that can be found in Ilu Aba Bor zone. Couples of kebeles per district were chosen by lottery after receiving the list of kebeles (smallest administrative units) from each selected district. Finally, a computer-generated software was used to choose the study participants from a sampling frame that contained a list of houses from the chosen kebeles. If a household had more than one eligible member, we used the lottery approach to select one person at random from the households. Non-eligible individuals in household were skipped to the following households. Figure 1 illustrates the schematic sampling procedure.
 |
Figure 1 Schematic presentation of sampling procedure to study factors associated with Podoconiosis in Ilu Aba Bor residents, South West Ethiopia, 2022. |
Study Variables and Operational Definition
The prevalence of podoconiosis served as the study’s dependent variable. Age, sex, family size, wealth index, ethnicity, occupation, religion, Years lived in the study area and educational status were employed as independent variables from socioeconomic and demographic factors. Shoe-wearing and personal hygiene characteristics, including how often people wear shoes, how often they use soap to wash their feet, how many pairs of shoes they own, and whether they have a history of leg swelling in the family, were also independent variables in our analysis.
Data collectors received hands-on instruction in the clinical diagnosis of podoconiosis based on endemic areas’ clinical algorithms,29 the disease staging system,30 and the technique for measuring leg circumference.31 Accordingly, someone affected by podoconiosis was characterized as a person who had a history of burning in the feet when the swelling first appeared; visible swelling that began at the feet and moved upwards; and no known clinical signs or symptoms of lymphatic filariasis or leprosy. The clinical indicators were an assessment of Aden lymphangitis (ALA), a reddish-hot, swollen leg with groin pain,11 the leg circumference between the level of the ankle and the knee measured with a tape,30 and mossy lesions, which are papillomatous horny lesions that give the skin a rough look.32 Fixed household assets were used to calculate the wealth index, and the factor score was obtained using Principal Component Analysis (PCA). The composite score was then divided into three tertiles.
Data Collection Procedures and Quality Control
The data were collected using an interviewer-administered structured questionnaire and an observational check list that was created from relevant literature with local context modifications. The sociodemographic factors, foot wear and personal hygiene characteristics, and knowledge of podoconiosis causes and prevention were all included in the questionnaire’s theme sub-sections.
Five BSc nurses with knowledge of the disease’s diagnosis and treatment were chosen for data collection, and one health officers were chosen for supervision and given a three-day training course.
Training was given on the nature, etiology, management, and prevention of podoconiosis, as well as the clinical characteristics that set it apart from other illnesses including leprosy and chronic edema. It also included the assessment of ALA and the presence of open wounds and mossy lesions. Before beginning the actual data collection, a pre-test on 5% of the sample at Buno Bedele Zone was conducted to ensure the accuracy of the data. During the house-to-house visits, the interviewers were led by the village chairpersons and health extension workers. During the diagnosis of the presence of podoconiosis and measurement of leg circumference, every attempt was made to reduce inter-observer bias. To account for intra-rater variance, the leg circumference was measured three times by each data collector. The average of the three measurements was then computed. Supervisors went through each questionnaire at the end of each data collection day.
Data Processing and Analysis
All data was checked visually, coded, entered into Epi-info version 4.6.0, and then exported into SPSS version 25 software for analysis. For continuous, normally distributed data, descriptive statistics were run and the mean (SD) was displayed. For categorical predictors, frequency and percentage were computed. To produce a wealth index, a PCA was used.
Select potential variables for multivariable regression analysis, a simple binary logistic regression analysis was carried out. The cut-off value used to determine which variables were suitable for the multivariable regression was a p-value of 0.25. In order to test for multi-collinearity amongst independent variables, pseudo variance inflation factor was used. The Hosmer–Lemeshow goodness-of-fit test was used to determine whether the multivariable logistic regression model was adequately fitted to predict the outcome variables. Finally, multivariable binary logistic regression was used to identify factors associated with podoconiosis at 5% level of significance.
Ethical Considerations
The Mattu University Ethical Review Committee provided a letter of ethical approval for the study. The zonal health department for Ilu Aba Bor and the zonal government were then addressed in an official letter. The letter was delivered to the management of each district health office that was chosen. After clearly explaining the study’s goal to each participant, verbal informed consent was obtained. Participants over the age of 18 signed a written informed consent form; participants under 18 had their consent signed on their behalf by their parents or legal guardians. Parents and legal guardians of study participants and participants were informed that they had the complete right to withdraw from the study without losing any of their rights. Moreover, consent was obtained from under the age of 18. The confidentiality of the data was ensured by omitting participant names from the questionnaire. This study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-Demographic and Economic Characteristics
Out of the 505 participants in this survey, 491 houses were interviewed, yielding a response rate of 97.2%. Of 491 participants, 41% were men and 59% were women. The participant’s mean (SD) age was 44.23 ± 13.40 SD. The respondents had, on average, lived in the research area for 29.19 ± 21.94 years. More than one-thirds of the respondents (n = 194, 39.9%) had no formal education. Around a quarter of the participants (n = 129, 26.2%) came from lower tertile wealth index (Table 2).
 |
Table 2 Socio-Demographic Characteristics of the Study Participants, 2022 |
Foot Wearing and Personal Hygiene Related Characteristics
When they put on their first pair of shoes, participants had an average age (SD) of 9.63 ± 6.62 years. Approximately 15.1% of the participants had no shoes at all, and 20.1% of the respondents said they usually go barefoot at home. The majority of study subjects (92.3%) wash their feet every day, and 62.2% never go barefoot. The majority of respondents—nearly two-thirds—lived in homes with earth floors (Table 3).
 |
Table 3 Foot Wearing and Personal Hygiene Related Characteristics of the Study Participants, 2022 |
Knowledge Related Aspects Among People with and without Podoconiosis
Only 159 participants (32.3%) out of 491 heard about podoconiosis. More than one-fourth (n = 43, 26.8%) of respondents who had heard of the condition stated that soil particles are the cause of podoconiosis, and more than three-quarters (n = 124, 78.01%) of participants believed that podoconiosis is a preventable disease (Table 4).
 |
Table 4 Knowledge Related Aspects the Study Participants, 2022 |
Prevalence of Podoconiosis
The prevalence of Podoconiosis in this study was found to be 5.7% (95% CI: 3.6–7.2) (Figure 2).
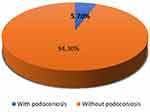 |
Figure 2 Prevalence of Podoconiosis among Ilu Aba Bor residents, Ethiopia, 2022. (n = 491). |
ALA, Clinical Feature and Coping Strategies
About 74.8% of the cases did not hear about podoconiosis. Over-55-year-old age groups had the highest prevalence of podoconiosis (36.6%). From every case combined, it was found that 55.3%, 29%, and 15.7% were in clinical stages 1, 2, and 3 respectively.
Around (n = 2, 8.6%) of the patients had ALA at the time of the interview based on their medical history and physical examination. The coping mechanisms used to lessen morbidity during ALA episodes included (n = 11, 40.5%) staying in bed, (n = 13, 47.6%) using antibiotics, (n = 17, 59.5%) reducing exertion, and (n = 7, 26.2%), utilizing traditional herbs (Table 5).
 |
Table 5 Clinical Features of Podoconiosis and ALA of the Study Participants, 2022 |
Factors Associated with Podoconiosis
Variables like marital status, wealth status, educational level, number of pairs of shoes owned, average distance from water source to home, and whether or not podoconiosis was known were significant on bi-variable logistic regression analysis with a p-value of less than 0.25. All of these independent variables were examined using multivariable logistic regression analysis, and three of the six independent variables had a significant association with the prevalence of podoconiosis at a p-value of 0.05.
Respondents from lower tertile wealth status households were 2.09 times more likely to be afflicted by podoconiosis than respondents from higher tertile wealth status households [AOR = 2.09; CI:(1.384, 5.343)]. When compared to respondents with educational status of secondary or higher, those with no formal education were 2.23 times more likely to be affected by podoconiosis [AOR = 2.23; CI: (1.179–3.820)]. The results of this study also showed that those who traveled more than 30 minutes to the nearest water source from their homes were 2.06 times more likely to have podoconiosis than those who traveled less than 30 minutes [AOR = 2.06; CI: (1.78–7.35)] (Table 6).
 |
Table 6 Multivariable Logistic Regression Output for Factors Associated with Podoconiosis in Ilu Aba Bor Residents, Ethiopia, 2022 |
Discussion
Podoconiosis is common in tropical and subtropical regions, particularly in African nations, among the world’s poorest, most isolated, and underprivileged populations. This study found that 5.7% of people in the study area are affected by podoconiosis. This finding is higher than a study conducted in Rwanda which ranged 16.5 to 45.5 per 100,000,33 Gulliso district (2.8%)11 and Wayu district (3.05%) of Ethiopia.32 This study was also found to be higher than the study conducted in volcanic mount of great rift valley in Kenya with overall prevalence of 3.4%.34 The higher prevalence of podoconiosis in our study than in other districts of Rwanda might result from differences in areas targeted for the survey (this study was done in endemic area). However, another possible reason might be a greater use of prevention measures, such as footwear and improved access to water in Rwanda.
Moreover, the prevalence of podoconiosis in this study is in line with studies conducted in Sodo district (5.4%),27 Bedelle Zuria (5.6%)25 and Gamo zone (6.3%) of Ethiopia.26 But the finding is lower the study conducted in Midakegn district, Ethiopia 7.4%.35 The difference might be due to the difference in study setting as the all districts located in Ethiopia share similar socio-demographic and lifestyles. Furthermore, the highest podoconiosis prevalence in these areas may be related to low foot wear use, limited access to water, and an environment that is conducive to the development of the disease, including soil that is often rich in clay particles.36
Wealth status was found to be significantly associated with podoconiosis in this study. Participant who had lower tertile wealth status was two times more likely to develop podoconiosis than participants who had higher tertile wealth index. The finding of this study is in line with study conducted in north Ethiopia and Waghamra zones of Amhara region.28,37 This might be because as family income declines, living conditions deteriorate, people are more likely to go barefoot and have trouble getting to school, which results in a lack of knowledge about preventative techniques.
In this study, those who travelled more than thirty minutes to get to the water source had a higher risk of developing podoconiosis than those who travelled less than thirty minutes. This might be due to that, as far they go barefoot across farming lands, they more likely to be affected by the disease.
Level of education is another factor associated with podoconiosis in this study. The odds of acquiring podoconiosis were higher among study participants who had no formal education as compared to those study participants with secondary schools and above. The finding of this study is line with study conducted in Sodo Zuria, Ethiopia.27 The likelihood of developing podoconiosis rises with lesser levels of schooling. As the sickness advances in its stages, victims abandon their families as a result and turn to begging, which is one of the reverse effects.38,39
Despite, Podoconiosis is an easily preventable and manageable disease; still, there is high prevalence. As far as podoconiosis is concerned, treatment of the early stages of disease is relatively straightforward, and comprises daily washing with soap and dilute bleach, topical ointment, elastic bandages where swelling is predominant, and routine use of socks and shoes.40
Strengths and Limitations of This Study
The fact that this study was a community-based study, the study has some limitations. First, due to stigma, families may choose to conceal individuals who are affected. Second, important variables like knowledge, attitude, and practice of the community toward podoconiosis were absent from the study because there was no validated tool to measure them in Ethiopia.
Conclusion
In comparison to earlier investigations, this study discovered that podoconiosis is highly prevalent in the study area, affecting one in every seventeen participants. Podoconiosis development was significantly affected by the wealth index of the households, level of education, and average dwelling distance from water source. Therefore, local government and non-government stakeholders have to integrate NTDs preventive and curative interventions with existing programs. So, government organizations have to plan modalities to enhance the shoe wearing and feet washing practices in line with the primary health care programs in where it is endemic.
Abbreviation
AOR, Adjusted Odd Ratio; ALA, Aden lymphangitis; COR, Crude Odd Ratio; DALYs, Disability-adjusted life years; MFTPA, Mossy Foot Treatment and Prevention Association; NTD, Neglected Tropical Diseases; PCA, Principal Component Analysis; SD, Standard Deviation; WHO, World Health Organization.
Data Sharing Statement
Data will be available from the corresponding author upon request.
Acknowledgments
Our heartfelt gratitude goes to the Mattu University for support by all necessary services. Additionally, we appreciate the support from Hospital’s administrations and data collector.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kebede B, Martindale S, Mengistu B, et al. Integrated morbidity mapping of lymphatic filariasis and podoconiosis cases in 20 co-endemic districts of Ethiopia. PLoS Negl Trop Dis. 2018;12(7):e0006491. doi:10.1371/journal.pntd.0006491
2. Deribe K, Wanji S, Shafi O, et al. The feasibility of eliminating podoconiosis. Bull World Health Organ. 2015;93:712–718. doi:10.2471/BLT.14.150276
3. Nenoff P, Simon JC, Muylowa GK, Davey GJ. Podoconiosis–non‐filarial geochemical elephantiasis–a neglected tropical disease? JDDG. 2010;8(1):7–13. doi:10.1111/j.1610-0387.2009.07099_supp.x
4. Johnston EA, Teague J, Graham JP. Challenges and opportunities associated with neglected tropical disease and water, sanitation and hygiene intersectoral integration programs. BMC Public Health. 2015;15(1):1–14.
5. Wanji S, Deribe K, Minich J, et al. Podoconiosis–From known to unknown: obstacles to tackle. Acta Trop. 2021;219:105918. doi:10.1016/j.actatropica.2021.105918
6. Deribe K, Cano J, Newport MJ, et al. The global atlas of podoconiosis. Lancet Glob Health. 2017;5(5):e477–e9. doi:10.1016/S2214-109X(17)30140-7
7. World Health Organization. Control of neglected tropical diseases: podoconiosis: endemic non-filarial elephantiasis. Available from: https://www.who.int/teams/control-of-neglected-tropical-diseases/lymphatic-filariasis/podoconiosis-endemic-non-filarial-elephantiasis.
8. Tora A, Franklin H, Deribe K, Reda AA, Davey GJS. Extent of podoconiosis-related stigma in Wolaita Zone, Southern Ethiopia: a cross-sectional study. Springerplus. 2014;3(1):1–7.
9. World Health Organization. Accelerating work to overcome the global impact of neglected tropical diseases: a roadmap for implementation. World Health Organization; 2012.
10. Burn H, Aweke S, Wondie T, et al. Podoconiosis, trachomatous trichiasis and cataract in northern Ethiopia: a comparative cross sectional study. PLoS Negl Trop Dis. 2017;11(2):e0005388.
11. Alemu G, Tekola Ayele F, Daniel T, Ahrens C, Davey GJ. Burden of podoconiosis in poor rural communities in Gulliso woreda, West Ethiopia. PLoS Negl Trop Dis. 2011;5(6):e1184. doi:10.1371/journal.pntd.0001184
12. Mengitsu B, Shafi O, Kebede B, et al. Ethiopia and its steps to mobilize resources to achieve 2020 elimination and control goals for neglected tropical diseases: spider webs joined can tie a lion. Int Health. 2016;8(suppl_1):i34–i52. doi:10.1093/inthealth/ihw007
13. Ethiopian Federal Misitry of Health. National neglected tropical diseases master plan 2015/16–2019/20; 2016.
14. Davey G, Burridge EJP. Community-based control of a neglected tropical disease: the mossy foot treatment and prevention association. PLoS Negl Trop Dis. 2009;3(5):e424. doi:10.1371/journal.pntd.0000424
15. Tomczyk S, Tamiru A, Davey GJ. Addressing the neglected tropical disease podoconiosis in Northern Ethiopia: lessons learned from a new community podoconiosis program. PLoS Negl Trop Dis. 2012;6(3):e1560. doi:10.1371/journal.pntd.0001560
16. Deribe K, Kebede B, Tamiru M, et al. Integrated morbidity management for lymphatic filariasis and podoconiosis, Ethiopia. Bull World Health Organ. 2017;95(9):652. doi:10.2471/BLT.16.189399
17. Ethiopian Federal Misitry of Health. The third national neglected tropical diseases strategic plan 2021–2025; 2021.
18. Deribe K, Negussu N, Newport MJ, Davey G, Turner RS. The health and economic burden of podoconiosis in Ethiopia. Hygiene. 2020;114(4):284–292.
19. Deribe K, Tomczyk S, Tekola-Ayele FJ. Ten years of podoconiosis research in Ethiopia. PLoS Negl Trop Dis. 2013;7(10):e2301. doi:10.1371/journal.pntd.0002301
20. Tekola-Ayele F, Yeshanehe WE. Podoconiosis: tropical lymphedema of the lower legs; 2014.
21. Mousley E, Deribe K, Tamiru A, Davey GJH. The impact of podoconiosis on quality of life in Northern Ethiopia. Health Qual Life Outcomes. 2013;11(1):1–11.
22. Shahvisi A, Meskele E, Davey GJH, Rights H. A human right to shoes? Establishing rights and duties in the prevention and treatment of podoconiosis. Health Hum Rights. 2018;20(1):53.
23. Deribe K, Cano J, Giorgi E, et al. Estimating the number of cases of podoconiosis in Ethiopia using geostatistical methods. Wellcome Open Res. 2017;2017:2.
24. Ethiopian Central Statistical Agency MPC. Population and Housing Census; 2007. Available from: https://www.statsethiopia.gov.et/census-2007-2/.
25. Tekola Ayele F, Alemu G, Davey G, Ahrens CJ. Community-based survey of podoconiosis in Bedele Zuria woreda, west Ethiopia. Int Health. 2013;5(2):119–125. doi:10.1093/inthealth/iht003
26. Getachew T, Churko CJ. Prevalence of podoconiosis and its associated factors in Gamo Zone, Southern Ethiopia. J Foot Ankle Res. 2021;15(1):1–12.
27. Elias A, Yemane H, Meskele MJ, Medicine A. Podoconiosis prevalence and its associated factors in Soddo Zuria district, Wolaita zone, south Ethiopia. J Pharm Altern Med. 2016;13:48–56.
28. Getie A, Atamenta T, Nigatu R, Abera A, Girma MJ. Magnitude of Podoconiosis and its associated factors among an adult population in Waghmra Zone, Ethiopia: a cross-sectional study. BioMed Res Int. 2020;2020:1.
29. Deribe K, Florence L, Kelemework A, et al. Developing and validating a clinical algorithm for the diagnosis of podoconiosis. Trans R Soc Trop Med Hyg. 2020;114(12):916–925. doi:10.1093/trstmh/traa074
30. Tekola F, Ayele Z, Mariam DH, Fuller C, Davey GJ, Health I. Development and testing of a de novo clinical staging system for podoconiosis (endemic non‐filarial elephantiasis). Trop Med Int Health. 2008;13(10):1277–1283. doi:10.1111/j.1365-3156.2008.02133.x
31. Southampton N, Centre BR. National institute for health research. 2017. Available from: https://www.uhs.nhs.uk/Media/Southampton-Clinical-Research/Procedures/BRCProcedures/Procedure-for-adult-circumference-measurements.pdf.
32. Bekele K, Deribe K, Amberbir T, Tadele G, Davey G, Samuel AJ. Burden assessment of podoconiosis in Wayu Tuka woreda, east Wollega zone, western Ethiopia: a community-based cross-sectional study. BMJ open. 2016;6(9):e012308. doi:10.1136/bmjopen-2016-012308
33. Deribe K, Mbituyumuremyi A, Cano J, et al. Geographical distribution and prevalence of podoconiosis in Rwanda: a cross-sectional country-wide survey. Lancet Glob Health. 2019;7(5):e671–e80. doi:10.1016/S2214-109X(19)30072-5
34. Muli J, Gachohi J, Kagai JJ. Soil iron and aluminium concentrations and feet hygiene as possible predictors of Podoconiosis occurrence in Kenya. PLoS Negl Trop Dis. 2017;11(8):e0005864. doi:10.1371/journal.pntd.0005864
35. Geshere Oli G, Tekola Ayele F, Petros BJ, Health I. Parasitological, serological and clinical evidence for high prevalence of podoconiosis (non‐filarial elephantiasis) in Midakegn district, central Ethiopia. Trop Med Int Health. 2012;17(6):722–726. doi:10.1111/j.1365-3156.2012.02978.x
36. Deribe K, Brooker SJ, Pullan RL, et al. Epidemiology and individual, household and geographical risk factors of podoconiosis in Ethiopia: results from the first nationwide mapping. Am J Trop Med Hyg. 2015;92(1):148. doi:10.4269/ajtmh.14-0446
37. Molla YB, Tomczyk S, Amberbir T, Tamiru A, Davey GJP. Podoconiosis in East and west gojam zones, northern Ethiopia. PLoS Negl Trop Dis. 2012;6(7):e1744. doi:10.1371/journal.pntd.0001744
38. Yimer M, Hailu T, Mulu W, Abera BJ. Epidemiology of elephantiasis with special emphasis on podoconiosis in Ethiopia: a literature review. J Vector Borne Dis. 2015;52(2):111.
39. Berhane Y, Mariam DH, Kloos H. Epidemiology and Ecology of Health and Disease in Ethiopia. Shama Books; 2006.
40. Yakob B, Deribe K, Davey GJ. Health professionals’ attitudes and misconceptions regarding podoconiosis: potential impact on integration of care in southern Ethiopia. Hygiene. 2010;104(1):42–47.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.