Back to Journals » International Journal of General Medicine » Volume 13
From Best Evidence to Best Practice: Enteral Nutrition from Continuous Nasal Feeding in Stroke Patients
Authors Sheng L, Yin L, Peng D, Zhao L
Received 3 July 2020
Accepted for publication 8 October 2020
Published 22 October 2020 Volume 2020:13 Pages 927—936
DOI https://doi.org/10.2147/IJGM.S269393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lijuan Sheng,1 Lihong Yin,1 Dezhen Peng,1 Liping Zhao2
1Department of Neurology, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, People’s Republic of China; 2Department of Nursing, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, People’s Republic of China
Correspondence: Liping Zhao
Department of Nursing, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, People’s Republic of China
Tel/ Fax +86 731-8529-4072
Email [email protected]
Background: Best evidence regarding enteral nutrition from continuous nasal feeding in stroke patients is limited. The aim of this study was to explore the best evidence of continuous nasal feeding in stroke patients and translate the evidence into clinical practice.
Methods: This study utilized the standard procedures of the Joanna Briggs Institute (JBI) evidence-based nursing centers’ clinical evidence-practice application system. The baseline assessment of stroke patients in the neurology ward was conducted. A pre- and post-implementation audit approach was used in this study and adopted the Getting Research into Practice program. We analyzed the compliance of nurses with best practice and its impact on patients’ gastrointestinal function and complications, aspiration, aspiration pneumonia, nurses’ daily workload of nasal feeding, and the length of hospitalization before and after implementing the evidence-based strategies.
Results: After application of the evidence-based strategies, nurses’ compliance with best practice was improved. The incidence of patients’ gastrointestinal complications including vomit (χ 2 = 5.195, P=0.023), palirrhea (χ 2 = 4.216, P=0.039), diarrhea (χ 2 = 4.514, P=0.042), constipation (χ 2 = 5.535, P=0.035) and gastric retention (χ 2 = 4.541, P=0.042) decreased significantly after the application of the best evidence. The working time of nurses undergoing nasal feeding decreased from 23.71 ± 3.22 min to 7.73 ± 1.14 min (P =0.000) and the length of patient’s hospitalization decreased from 35.63 ± 4.45 days to 35.00 ± 3.70 days (P=0.534). The rate of aspiration, aspiration pneumonia did not show a significant difference after implementation of the evidence-based strategies.
Conclusion: The results revealed that the evidence-based practice of continuous nasal feeding in stroke patients is an effective method to improve nursing quality and reduce gastrointestinal complications, which was worthy of clinical application.
Keywords: stroke, nasal feeding, evidence-based nursing, best evidence, complications
Introduction
Nutritional supportive therapies, as an important measure for the treatment of critically ill patients, are divided into parenteral nutrition (PN) and enteral nutrition (EN). EN generally refers to the nutritional therapy in which liquid formulations or mixed foods are delivered to the gastrointestinal tract to supplement or provide all the calorie needs of the individual through a feeding tube or mouth.1 Nasal feeding is one of the main ways of EN, and it is an important treatment measure to improve the prognosis of critically ill patients. It can maintain the function of the gastrointestinal tract, reduce infectious complications, and shorten hospitalization time compared to PN.2 Methods of nasal feeding mainly included continuous (continuously pumped through the nutrition pump for 24 hours), cyclic (through the nutrition pump cycle, less than 24 hours a day), intermittent (every 4 to 6 hours per time, each time continuous 20 to 60 min) and bolus feeding (through gravity or syringe to complete nasal feeding in a very short time, several times a day).3 Stevens et al4 found that diarrhea caused by intermittent nasal feeding occurred more frequently and lasted longer than continuous nasal feeding in the study of nasal feeding for trauma patients, and intermittent nasal feeding caused reflux aspiration more often. In addition, McClave et al5 found that continuous nasal feeding was more beneficial for critically ill patients. Metanalyses have shown that continuous pump nasal feeding could reduce the incidence of enteral nutrition-related complications, and it was better than intermittent nasal feeding in terms of safety.6,7 However, due to the low level of literature evidence grade in these studies, there are still limitations in its clinical application. Nevertheless, some studies also suggested that intermittent nasal feeding did not increase the incidence of nasal feeding complications, and in the effect on the gastric acid secretion and pH value, it was less than that of continuous nasal feeding.4 Therefore, there is still controversy and a lack of best evidence about which nasal feeding method is the most effective and reliable. This study summarized the best evidence of nasal feeding and applied it to the clinical practice of stroke patients in the acute setting in the department of neurology, in order to optimize the nursing norms of nasal feeding, reduce the incidence of adverse complications and improve the quality of nursing.
Methods
Study Design and Population
The study was conducted to stroke patients in the department of neurology, the Second Xiangya Hospital of Central South University, Changsha, Hunan, China. Before and after the application of the evidence, 12 clinical nurses were included in the department of neurology. All of them were registered nurses, working in the neurology department for 2–20 years, with an average of 8.08 ±5.70 years; and 11 of them with a bachelor’s degree, 1 with master’s degree. Before the application of the evidence, 38 stroke patients were included and 125 episodes of nasal feeding were performed. After the application of the evidence, 30 patients were included and 60 episodes nasal feeding was performed. The baseline characteristics such as age, gender, nation, marital status, education, medical payment mode, and Glasgow Coma Scale (GCS) score were collected in stroke patients. The criteria for inclusion of patients were as follows: (1) ischemic stroke patients according to the diagnostic criteria revised by the fourth National Conference on Cerebrovascular Diseases and finally diagnosed by CT or MRI; (2) dysphagia and water swallow test ≥ 3 grade; (3) ≥ 18 years old; (4) EN was applied within 48 hours after admission. The exclusion criteria including: (1) intestinal obstruction, active gastrointestinal bleeding, severe intestinal infection, diarrhea, shock, acute pancreatitis; (2) gastrointestinal failure, severe dyspepsia or poor absorption, severe heart, liver, and kidney dysfunction, pneumonia or suspected pneumonia. Termination criteria: (1) unable to complete the intervention; (2) nasal feeding time <7 days. This study acquired the ethics approval from the medical ethics committee of the Second Xiangya Hospital of Central South University. All the patients or the patient’s relatives and nurses agreed to join the research and signed the informed consent. This study was conducted in accordance with the declaration of Helsinki.
Evidence Retrieval
Establishment of the Question
Evidence-based questions were formed using PIPOST8 model. P (Population): Stroke patients with enteral nutrition support therapies; I (Intervention): Continuous nasal feeding measures; P (Professional): physicians and nurses in department of neurology; O (Outcome), O1, Nurse’s compliance and workload, O2, gastrointestinal function and complications (vomit, palirrhea, diarrhea, constipation, gastric retention; O3, aspiration and aspiration pneumonia; O4, the length of hospitalization); S (Setting): department of neurology. T (Type of evidence): Recommendation practice, evidence summary, guidelines and systematic reviews.
Search for Evidence
The time span of the data was from the establishment of the database to October 2018. Database including: China Guide Network; China Biomedical Literature Database (CBM); Fudan evidence-based Nursing Center Database; National Guideline Clearinghouse (NGC); Guidelines International Network (GIN); BMJ Best Practice; Cochrane Library; PubMed; Cumulative Index to Nursing and Allied Health Literature (CINAHL). Keywords including: enteral nutrition, nasogastric feeding, tube feeding, nasogastric tube feeding, enteral feeding pump, enteral nutrition pump, continuous pump feeding, intermittent bolus, intermittent nasogastric feeding, intermittent tube feeding.
Criteria for Inclusion and Exclusion of Evidence
The inclusion criteria of evidence resources in this practice were decision support systems, clinical practice guideline reports, evidence summary, and systematic review. Exclusion criteria included all kinds of original research.
The Results of the Literature Search
A total of 315 articles were searched. After screening, 288 articles were excluded, of which 220 were inconsistent with the subject, 88 cannot find the original articles, and finally, 7 were initially included. After the final screening, 6 articles were included in the evidence resources of this project, including 3 systematic reviews6,7,9 (2 CBM and 1 Cochrane Library) and 3 clinical guidelines10−12 (1 NGC, 1 GIN1, and 1 China Guide Network). One updated guideline of the European Society of Clinical and Metabolic (ESPEN) for nutritional support treatment for critically ill patients in 2018 was excluded since the ESPEN guidelines provide the best medical nutritional therapy to critically ill patients, define how to assess the nutritional status of an ICU patient and particular conditions frequently observed in intensive care such as patients with dysphagia, frail patients, multiple trauma patients, abdominal surgery, sepsis, and obesity are discussed to guide the practitioner toward the best evidence-based therapy, which there were some limitations in the application of evidence in this study.
Evaluation Criteria for the Quality of Evidence
Articles meeting inclusion criteria were appraised for methodological quality independently by two nurses, who were trained in evidence-based nursing. Any inconsistency was resolved by consultation until a consensus was reached.13 We followed the update of the clinical guidelines research and evaluation system (AGREE II)14 in 2012 to comprehensively judge the recommended levels of the guidelines. At the same time, the JBI quality evaluation tool15 was used to evaluate the quality of the systematic evaluation, best practices, and evidence summary. For evidence derived from JBI, the results of its evidence rating and recommendation level were directly applied. In addition, for the evidence that did not come from JBI, the 2014 version of JBI evidence pre-classification and evidence recommendation level system was adopted.
Summary of Evidence
Draft recommendations were developed based on the included evidence. After consultation and discussion among one evidence-based nursing expert, two nasal feeding experts, and two clinical nursing managers, the evidence was divided into six topics including: a nursing group of nasal feeding (A multi-disciplinary nutrition support group); The patient’s condition must be evaluated before choosing a certain method of nasal feeding; nasal feeding posture; nasal feeding checking; special nursing; and complications monitoring. The extracted evidence was classified independently by two researchers, and any inconsistency was resolved by consultation until a consensus was reached.
Developing Standard Audit Criteria of the Evidence
According to the (FAME),16 the evidence including its feasibility, appropriateness, meaningfulness and effectiveness were audited. All retrieved B-level and above evidence was applied in this study. In addition, the evidence application project team has developed six standard audit criteria via FAME. Standard 1, nurses were aware of the importance of continuous nasal feeding and followed its standard procedures; Standard 2, nurses evaluated patients clinical situation before nasal feeding; Standard 3, nurses performed nasal feeding for patients rather than other medical staff; Standard 4, nurses could evaluate and deal with the patient’s adverse reactions or complications correlated with nasal feeding timely; Standard 5, nurses provided oral care for nasal feeding patients; Standard 6, nurses inspected and maintenance the nutrition pump regularly.
Clinical Application of Evidence
Data Collection
During the working day, two graduate students trained in evidence-based medicine were responsible for data collecting. One nurse and one trainee nurse were scheduled for data collecting on weekends and holidays. The night work nurse was assigned for collecting data at night and checked the information in the morning of the next day. A trainee nurse with a regular shift was arranged as an observer. The observation ended immediately after the nasal feeding tube was removed. The methods of data collection included the following three items:
Field Observation Method
Using the single-blind method, the nurses with fixed shifts (worked at the same time) were arranged as observers every day. The nurses were trained by the permanent staff in the quality audit team. The significance of the project, the observed contents, and the attention points were informed. Whether the nurses carried out continuous nasal feeding in accordance with the audit criteria were observed and recorded.
Quality Audit
The collected data, including the basic characteristics such as the age of the patients, the time of admission, the time of discharge, the time of nurses’ nasal feeding operation, the occurrence of gastrointestinal complications were reviewed.
Barriers to Best Practice
The baseline data of 12 nurses and 38 patients who met the inclusion criteria were audited from August 13 to November 19, 2018. Through the results of nurses compliance before application of the best evidence, we found that the main obstacles to the implementation of evidence included: (1) The nurse was lack of evidence-based nursing awareness; (2) No relevant continuous nasal feeding system and guidelines in neurology departments; (3) the choice of continuous nasal feeding methods were mainly based on clinical experience rather than evidence-based evidence. In response, the evidence application group has developed the following innovative approaches:
Strategy 1: Evidence-Based Nursing Training and Assessment for Nurses
In the daily process of nasal feeding, nurses did not know the evidence-based evidence. They mainly relied on clinical experience. In addition, they did not know that the patient’s condition needed to be specifically assessed when choosing nasal feeding procedures. The solution adopted by this group was to carry out evidence-based training and education on continuous nasal feeding rules and regulations for all nurses in the neurology department. This kind of training and education was presented in the way of multimedia teaching. The knowledge of nurses was evaluated before and after teaching, and the effect of nurse training was confirmed by asking questions in the morning and pushed this in the WeChat (a Chinese multi-purpose messaging, social media) group of nurses.
Strategy 2: A Standardized Nasal Feeding Process Was Developed
At present, there were no standard nasal feeding procedures and regulations in the neurology department of this study. The solution was to establish and improve the procedures and regulations through the related evidence-based resources. After that, the evaluation criteria were established as the basis for the effect of nurses’ nasal feeding training and daily inspection of nurses’ implementation. At the same time, the workflow of nasal feeding was introduced among nurses, and the time of nasal feeding operation was defined. In addition, the management of continuous nasal feeding has also been the daily duties of nurses.
Strategy 3: Strengthen Continuous Nasal Feeding Training
In the past, the traditional intermittent nasal feeding method was used in the training of nurses, so that they were not clear about the purpose and process of continuous nasal feeding. The solution was to shoot a video of continuous nasal feeding based on evidence and send it to the WeChat group of nurses, which was used for them to learn. After that, an assessment was conducted on each nurse to ensure that they had mastered the evidence-based method of continuous nasal feeding.
Re-Audit After the Application of the Evidence
After the evidence-based continuous nasal feeding evidence was applied and practiced in clinical, a study of 12 nurses and 30 patients who met the inclusion criteria was completed from December 11, 2018, to February 18, 2019.
Effectiveness Evaluation
Nurses’ Compliance with an Evidence-Based Continuous Nasal Feeding
An audit sheet used to record the implementation of each item was self-designed according to the constructed audit standards. The sheet was also used to analyze nurses’ compliance with evidence-based criteria. If the nurse completed the item of audit standard, marked “√” in the space, if not, marked “×”. In addition, if the criterion was not observed, it needed to be recorded or explained. The frequency of nurses on the completion of each item of evidence-based criteria was counted separately.
The Gastrointestinal Complications of Nasal Feeding
The complications included vomit, palirrhea, diarrhea, constipation, and gastric retention. Vomit is the involuntary, forceful expulsion of the contents of one’s stomach through the mouth and sometimes the nose. Palirrhea is defined as no symptoms of choking and coughing before nasal feeding but choking or wheezing and reflux in the process of nasal feeding. Diarrhea means that the patient defecates more than 3 times a day. Constipation is thought of as infrequent bowel movements, usually less than 3 stools per week. In this experiment, constipation is defined as having no defecation within 3 days. Gastric retention refers to the aspiration of gastric contents of the patient every 4 hours through the nasal feeding tube. If the amount of gastric contents extracted exceeds 200mL, the patient occurred gastric retention.
Aspiration and Aspiration Pneumonia
Aspiration refers to the countercurrent of stomach contents into the pharynx and trachea. Aspiration pneumonia means that the patient has an obvious history of aspiration and the chest X-ray examination of the patients showed that there were signs of infection in the lung compared to before. Or patients with two or more of the following manifestations, including fever, body temperature above 38.5°C; chest auscultation indicated rales; cough purulent sputum or sputum volume significantly increased; white blood cell count or neutrophil count increased; sputum culture was positive.
The Workload of Nurses on Nasal Feeding
To record the time spent by nurses on nasal feeding for each patient every day.
The Length of Hospitalization
The hospitalization days of the patient was recorded.
Statistical Methods
EpiData 3.1 was used for data entry and management, and the data entry quality was checked by the double data entry verification method. Data were analyzed using SPSS version 22. Descriptive analyses were performed using mean, standard deviation and frequency. χ2 test or Fisher’s exact test was used to compare the incidence of nasal feeding complications and aspiration and aspiration pneumonia before and after the application of evidence. T-test was used to compare the nutritional index of patients, the workload of nurses and the length of stay of patients before and after the application of evidence. A P value of less than 0.05 was considered statistically significant.
Results
Demographic Characteristics of the Stroke Patients
Based on the inclusion and exclusion criteria, a total of 68 participants were selected for final data analysis. The average age of 30 observation group participants was 61.71±10.17 years old, and about 21 of them were male. The results showed that there was no difference among age, gender, nation and any other characteristics in the observation group compared with the control group (P > 0.05). The details of these stroke patients’ features are shown in Table 1.
 |
Table 1 Demographic Characteristics of Stroke Patients |
Summary of the Best Evidence of Continuous Nasal Feeding
A consensus expert opinion about the best evidence for nasal feeding in stroke patients was finally compiled and used as a basis for decision-making after repeated consultation, induction, and modification (Table 2).
 |
Table 2 Summary of the Best Evidence of Continuous Nasal Feeding |
Nurses’ Compliance Before and After the Application of the Best Evidence
After the application of the evidence, the compliance rate of standard 1 increased from 20% to 100% and standard 2, 3 increased from 0% to 100%. In addition, the compliance rate of standard 4 increased from 71.2% to 100% and standard 5 increased from 44% to 100%. Besides, the compliance rate of standard 6 increased from 21.6% to 100%. The compliance of nurses’ evidence-based behavior was significantly improved (Table 3).
 |
Table 3 Compliance of Nurses Before and After the Application of the Best Evidence |
The Incidence of Gastrointestinal Complications Before and After the Application of Evidence
After the application of the evidence, the gastrointestinal complications including vomiting (χ2=5.195, P=0.023), palirrhea (χ2=4.216, P=0.039), diarrhea (χ2=4.514, P=0.042), constipation (χ2=5.535, P=0.035), gastric retention (χ2=4.541, P=0.042) were lower than that before the evidence. The difference was statistically significant (P <0.05) (Table 4).
 |
Table 4 The Incidence of Gastrointestinal Complications Before and After Application of the Best Evidence |
Incidence of Aspiration and Aspiration Pneumonia in Patients Before and After the Application of Evidence
After the application of evidence, the incidence of aspiration (F=2.478, P=0.249) and aspiration pneumonia (F=1.627, P=0.500) in patients with nasal feeding was lower than that before the application of evidence, and there was no case after the application of evidence, but the difference was not statistically significant (P > 0.05), as shown in Table 5.
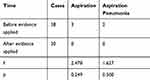 |
Table 5 The Incidence of Aspiration and Aspiration Pneumonia Before and After Application of the Best Evidence |
The Workload of Nurses on Nasal Feeding and Hospitalization Days Before and After the Application of Evidence
After the application of the evidence, the time of the nurses spent on nasal feeding was decreased from 23.71±3.22 min to 7.73 ±1.14 min, and the difference was statistically significant (P <0.05). The hospitalization days were decreased from 35.63±4.45 days to 35.00±3.70 days, and the difference was not statistically significant (P> 0.05), as shown in Table 6.
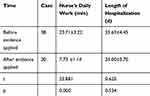 |
Table 6 The Workload of the Nurse and the Length of Hospitalization of Patients Before and After the Application of the Best Evidence |
Discussion
Feasibility Analysis of Clinical Evidence Applied to Practice
In this study, the clinical feasibility and suitability were fully considered in the application of evidence. After strict literature screening and quality evaluation, three systematic reviews and three clinical guidelines were included. Through the back-to-back evaluation and classification of the evidence by two evidence-based nursing training personnel, and screened by experts in this field, the best practice evidence suitable for the clinical situation and patients’ wishes was obtained finally, which was scientific and practical.
Application of the Best Evidence of Continuous Nasal Feeding into Practice Can Improve the Condition of the Stroke Patient
Currently, some researches support that continuous pump nasal feeding could reduce the incidence of nasal feeding complications, and it was better than traditional intermittent nasal feeding in ensuring the safety of nasal feeding. However, there was some clinical heterogeneity among these studies.17 In addition, due to the limitation of patients’ economic ability and medical operation habits in clinical nursing practice, continuous nasal feeding was not always widely used in clinical practice. Moreover, clinical nursing practice mainly depends on doctors’ decision-making or clinical experience and lacks the guidance of evidence-based practice. Based on the evidence-based practice, the latest evidence of continuous nasal feeding was applied to the nursing practice of stroke patients. The incidence of gastrointestinal complications was significantly lower than that before the application of the evidence. In addition, the workload of nurses was reduced. Before the application of the best evidence, the nurses always used intermittent nasal feeding method for stroke patients, so it took a relatively long time for each patient. Besides, nurses were not clear about the requirement and purpose of continuous nasal feeding and the operation was not up to the standard. However, after applying the best evidence, the method adopted by nurses was based on evidence-based medicine, which not only standardized the nasal feeding operation procedure but also shortened the time spent on each patient. Also, the incidence of aspiration and aspiration pneumonia in patients with continuous nasal feeding and the hospitalization days decreased, but the difference was not statistically significant. This may be related to the small sample size. In addition, the length of hospitalization may also be related to many factors such as the severity of the patient’s clinical condition, so it needs to be verified in large sample size in the future.
The Application of the Best Evidence of Continuous Nasal Feeding Effectively Improves the Quality of Nursing
Some studies have shown that continuous nasal feeding has advantages over intermittent nasal feeding and can effectively improve the quality of nursing.18–20 In this study, evidence-based continuous nasal feeding practice was introduced into clinical practice, which can enable nurses to better understand evidence-based nursing and solidify nursing behavior in their daily work. This not only updated nurses’ knowledge of evidence-based continuous nasal feeding but also significantly improved their compliance. In addition, through the analysis of obstacle factors, this study further put forward improvement measures and standardized the process of continuous nasal feeding in the hospital. It can standardize the nursing practice behavior of nurses and effectively improve the quality of clinical nursing.
To sum up, how to apply the best evidence to clinical practice has been the focus of attention in the field of nursing. Gurzick et al21 indicated that the promotion of evidence application project could improve the evidence-based thinking ability and compliance of clinical nurses, so as to improve the quality of clinical nursing.
Limitations
When we summarize the evidence, there may be conflicts in the review of evidence-based practice due to the cultural differences between China and the West, which may lead to the failure of evidence-based practice in clinical application. Therefore, we should consider the localization of evidence in the audit and application of evidence. In addition, the collection of data in this study was limited to one hospital, so the sample size was small. In order to better understand the effectiveness of the evidence-practice, it is also necessary to carry out multicenter, large sample studies and increase research in a patient with other diseases. Finally, a major limitation is a bias in the observer’s assessment, given that they are aware of the pre-/post-intervention study design.
Conclusions
In this study, evidence was obtained by the evidence-based method, and strict quality evaluation was carried out. Through the implementation of the best evidence of continuous nasal feeding, the compliance of nurses’ evidence-based practice was significantly improved and the incidence of complications was effectively reduced. This not only made nurses have a deeper understanding of the evidence-based practice but also promoted the wide promotion of evidence-based nursing practice in the neurology department. In addition, it also provided a reference for the follow-up work of evidence-based nursing and the transformation of evidence.
Data Sharing Statement
The datasets used and/or analyzed during the present study were availed by the corresponding author on reasonable request.
Funding
This work was supported by the Clinical Nursing Research Fund Project of the Second Xiangya Hospital. (2018-YHL-50).
Disclosure
The authors report no conflicts of interest for this work.
References
1. Bankhead R, Boullata J, Brantley S, et al. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33:122–167. doi:10.1177/0148607108330314
2. McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009;33:277–316.
3. Ichimaru S. METHODS of enteral nutrition administration in critically ill patients: continuous, cyclic, intermittent, and bolus feeding. Nutr Clin Pract. 2018;33:790–795.
4. Steevens EC, Lipscomb AF, Poole GV, et al. Comparison of continuous vs intermittent nasogastric enteral feeding in trauma patients: perceptions and practice. Nutr Clin Pract. 2002;17:118–122.
5. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40:159–211.
6. Wang YHYC. Effects of continuous nasogastric feeding on the incidence of complications:a systematic review. J Nurs. 2014;22:83–87.
7. Jianguo Yang JZBY. Effects of enteral feeding pump and intermittent bolus nasogastric feeding on reducing complications of enteral nutrition: a meta-analysis. Chin J Evid Based Med. 2014;2:197–204.
8. Aromataris E, Fernandez R, Godfrey CM, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–140. doi:10.1097/XEB.0000000000000055
9. White H, King L. Enteral feeding pumps: efficacy, safety, and patient acceptability. Med Devices (Auckl). 2014;7:291–298.
10. Hu Yanqiu CYWY. Construction of clinical practice guidelines for adult feeding through the nasogastric tube. Chin J Nurs. 2016;2:133–141.
11. Gomes F, Hookway C, Weekes CE. Royal College of Physicians Intercollegiate Stroke Working Party evidence-based guidelines for the nutritional support of patients who have had a stroke. J Hum Nutr Diet. 2014;27:107–121.
12. Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutri. 2019;38:48–79. doi:10.1016/j.clnu.2018.08.037
13. Newhouse RP, Dearholt SL, Poe SS, et al. Johns Hopkins Nursing Evidence-Based Practice Model and Guidelines. Indianapolis, IN: Sigma Theta Tau International Honor Society of Nursing; 2007.
14. Brouwers MC, Kho ME, Browman GP, et al. The Global Rating Scale complements the AGREE II in advancing the quality of practice guidelines. J Clin Epidemiol. 2012;65:526–534. doi:10.1016/j.jclinepi.2011.10.008
15. Duffy ME. The Joanna Briggs Institute: its contribution to evidence-based practice. Clin Nurse Spec. 2005;19:184–186. doi:10.1097/00002800-200507000-00007
16. Reynolds S. Evidence-Based Practice: A Critical Appraisal. John Wiley & Sons; 2008.
17. Lee JS, Auyeung TW. A comparison of two feeding methods in the alleviation of diarrhoea in older tube-fed patients: a randomised controlled trial. Age Ageing. 2003;32:388–393. doi:10.1093/ageing/32.4.388
18. Ichimaru S. Methods of enteral nutrition administration in critically ill patients: continuous, cyclic, intermittent, and bolus feeding. Nutr Clin Pract. 2018;33:790–795. doi:10.1002/ncp.10105
19. Shahriari M, Rezaei E, Bakht LA, et al. Comparison of the effects of enteral feeding through the bolus and continuous methods on blood sugar and prealbumin levels in ICU inpatients. J Educ Health Promot. 2015;4:95.
20. Evans DC, Forbes R, Jones C, et al. Continuous versus bolus tube feeds: does the modality affect glycemic variability, tube feeding volume, caloric intake, or insulin utilization? Int J Crit Illn Inj Sci. 2016;6:9–15.
21. Gurzick M, Kesten KS. The impact of clinical nurse specialists on clinical pathways in the application of evidence-based practice. J Prof Nurs. 2010;26:42–48.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
