Back to Journals » Clinical Ophthalmology » Volume 17
Four-Year Outcome of XEN 45 Gel Stent Implantation in a Swedish Population
Authors Busch T , Skiljic D , Rudolph T , Bergström A , Zetterberg M
Received 14 March 2023
Accepted for publication 30 May 2023
Published 3 July 2023 Volume 2023:17 Pages 1897—1910
DOI https://doi.org/10.2147/OPTH.S412400
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tobias Busch,1 Dragana Skiljic,1,2 Thiemo Rudolph,1 Anders Bergström,1,3 Madeleine Zetterberg1,2
1Department of Ophthalmology, Sahlgrenska University Hospital, Mölndal, Region Västra Götaland, Sweden; 2Department of Clinical Neuroscience, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 3Department of Ophthalmology, Skåne University Hospital, Lund, Sweden
Correspondence: Madeleine Zetterberg, Department of Clinical Neuroscience/ Ophthalmology, Institute of Neuroscience and Physiology, The Sahlgrenska Academy at University of Gothenburg, Mölndal, SE-431 80, Sweden, Tel +46 31 342 10 00, Fax +46 31 41 29 04, Email [email protected]
Purpose: To report the long-time success rate of XEN 45 gel stent implantation in a Scandinavian population.
Patients and Methods: This was a retrospective single-center analysis of all patients undergoing XEN 45 stent surgery between December 2015 and May 2017. The main outcome was success rate according to several definitions of success. Subgroup analysis was performed. Secondary outcomes were change in intraocular pressure (IOP) and number of IOP-lowering agents. Need for secondary glaucoma surgery, needling rate and complications were recorded.
Results: A total of 103 eyes could be evaluated after four years. Mean age was 70.6 years. Primary open-angle glaucoma (POAG) accounted for 46.6% and exfoliative glaucoma (PEXG) for 39.8%. Mean IOP dropped from 24.0 to 15.9 mmHg (p< 0.001) and IOP-lowering agents from 3.5 to 1.5 (p< 0.001). The success rate with individual target pressures after four years was 43.7%. Secondary glaucoma surgery was performed in 45 (43.7%) of cases. Combined cases (n=12) were not statistically different to stand-alone procedures (p=0.28). No difference between PEXG and POAG could be detected (p=0.44). During the learning curve, stent misplacement was common and resulted in worse outcome for less experienced surgeons.
Conclusion: The overall success rate of XEN 45 gel stent surgery in the present cohort is relatively low in a long-time follow-up under the given circumstances if all initial patients are included to follow-up. The influence of the surgeon’s learning curve is obvious, and improvement in success can be expected when used by experienced and high-volume surgeons. No significant differences were found in PEXG compared to POAG or in XEN surgery combined with cataract surgery compared to stand-alone.
Keywords: ab interno implant, glaucoma, minimal invasive glaucoma surgery, pseudoexfoliative glaucoma, surgical success, XEN 45 gel stent
Introduction
Primary open-angle glaucoma is characterized by chronic progressive loss of the retinal nerve fiber layer and reduction of the optic nerve border, resulting in progressive reduction of the visual field. The risk for glaucoma rises with older age, heredity, elevated intraocular pressure (IOP), pseudoexfoliative syndrome (PEX), diabetes mellitus and ethnicity among other risk factors.1
To inhibit progression of visual field loss, treatment consists mainly of lowering the IOP.2 The hallmarks of glaucoma management are early detection and initiation of treatment as well as continuous compliance to medical treatment.
First-line treatment consists of topical IOP-lowering pharmacologic agents or selective laser trabeculoplasty (SLT).3,4 Different substances have proven efficient and can be combined for additional IOP-lowering effect. In case of insufficient IOP control, intolerance due to side effects or suboptimal adherence to treatment, surgical intervention may become necessary.
Traditionally, the most frequent type of surgery has been filtering procedures (trabeculectomy, glaucoma shunts). Of these, trabeculectomy has been regarded as the gold standard procedure until recently.5 The complication profile of these procedures includes risk of infections, persistent hypotony, leakage, and fibrosis of the filtration bleb.6 Several new surgical techniques and devices have been introduced during the last years, often summarized as Minimal Invasive (or Incision) Glaucoma Surgery (MIGS), with the ambition for faster surgery, and better safety profile.7
The XEN 45 gel stent device (AbbVie Inc., North Chicago, IL, USA) consists of a 6 mm long gelatin tube with an internal diameter of 45 µm. It creates a new outflow facility for aqueous humor from the anterior chamber to the subconjunctival space.8 The mechanism of action is therefore comparable with trabeculectomy. As the device is implanted through a self-sealing limbal tunnel, neither conjunctival incision nor suturing is required, significantly shortening the surgery time compared to trabeculectomy.
The XEN gel stent is indicated for the management of refractory glaucoma as a stand-alone procedure or in combination with cataract surgery. In most studies, the type of procedure has no significant effect on the outcome,9–11 while some studies found significantly more failures in combined cases in POAG.12
Long-time results with this relatively novel technique are still scarce. Published results in large cohorts are limited to three years at the best of our knowledge.13,14 Furthermore, studies focusing on a Scandinavian cohort are lacking, which is of particular interest because of the high proportion of pseudoexfoliative glaucoma in this population.15 We consider it interesting to report the long-time results of our initial cohort, of which one-year results have been published earlier.16
Materials and Methods
Study Design
This was a single-center, retrospective observational chart review of all patients with open-angle-glaucoma who underwent glaucoma surgery with XEN 45 gel stent at the Department of Ophthalmology at Sahlgrenska University Hospital in Mölndal, Sweden between 1 December 2015 and 31 May 2017. The study protocol was approved by the local ethical committee before study initiation and was conducted in compliance with the declaration of Helsinki. The presented data was anonymized and due to the retrospective chart review, no written consent of the enrolled patients was regarded necessary by the ethical committee. For case presentation, written consent by the involved patient was obtained for publication, including photographs.
Study Population
All consecutive patients who underwent XEN 45 gel stent surgery alone (XEN stand-alone) or in combination with cataract surgery (combined XEN and cataract) during the study period were enrolled retrospectively. Patients were offered XEN 45 gel stent implantation if suitable as assessed by the surgeon. In our hands, the indication for XEN and trabeculectomy are virtually the same, as both methods have the same principal working mechanism. In cases with cataract and glaucoma, we prefer combined surgery with phacoemulsification and XEN stent instead of trabeculectomy. Indications for surgery were either uncontrolled intraocular pressure (IOP), intolerance to anti-glaucoma drugs, progression of visual field defects, or a combination of the factors mentioned above. There were no limitations concerning preoperative level of IOP, grade of visual field defect, or type of glaucoma. Eyes with previous filtrating glaucoma surgery including previous failed XEN surgery were excluded from analysis. In case of bilateral implantation, both eyes were included.
The data comprises the result of surgery performed by four anterior segment surgeons, none of whom had any previous experience of the XEN 45 gel stent.
Surgical Technique
The surgery was performed either as a stand-alone procedure or in combination with cataract surgery. Some patients received preservative-free dexamethasone a week prior to surgery, but most patients did not. Standard preoperative preparation was performed including local anesthesia with topical tetracaine (1%) (Tetracaine, Bausch&Lomb Nordic AB, Stockholm, Sweden). Preoperative miosis was achieved by topical pilocarpine 2% (Trimb Healthcare AB, Stockholm, Sweden) for stand-alone procedures. In the event of combined surgery, cataract surgery was performed first, after which mydriasis was converted to miosis by intracameral acetylcholine chloride, 10 mg/mL (Miochol-E®, Bausch&Lomb Nordic AB, Stockholm, Sweden). In stand-alone procedures the anterior chamber was infused with xylocaine 10 mg/mL (Aspen Nordic, Ballerup, Denmark) and then filled with ocular viscoelastic device Healon GV (Johnson & Johnson Vision, Uppsala, Sweden). The conjunctiva in the upper nasal quadrant was hydrodissected by injection of 0.1 mL Mitomycin C 0.2 mg/mL or 5-Fluorouracil 50 mg/mL (extempore, Apoteket AB, Stockholm, Sweden). A peripheral corneal incision 1.2 mm wide was made nasally for later insertion of a counter-traction Vera hook (a1 medical GmbH, Radolfzell am Bodensee, Germany). The main incision of 1.8 mm width was placed as a peripheral corneal tunnel in the temporal inferior quadrant. The XEN® 45 Gel Stent, preloaded into a XEN® Injector (Allergan plc, Dublin, Ireland), was advanced through the anterior chamber, trabecular meshwork, and sclera. The XEN 45 gel stent was then released into the subconjunctival or subtenonal space. If unproperly positioned, further manipulations could be performed to optimize positioning, ie, explantation and reloading of the stent, or grasping the stent with forceps for manipulation of the stent through the intact conjunctiva. Intracameral Healon was removed and cefuroxime (Aprokam® Laboratoires Théa, Clermont-Ferrand, France) was instilled in the anterior chamber at the end of the procedure.
Postoperatively, all topical and systemic (acetazolamide; Diamox®, Amdipharm Ltd, London, Great Britain) anti-glaucomatous drugs were suspended, and anti-inflammatory topical therapy initiated with preservative-free dexamethasone 1 mg/mL (Dexafree®, Laboratoires Théa, Clermont-Ferrand, France) 6–8 times/day. Depending on individual assessment, dexamethasone drops were tapered during a period of at least two months. Typically, follow-ups were scheduled at day 1 and after 1, 2, 3, 4, 6 and 8 weeks, with individual adjustments. In case of encapsulation or fibrosis, needling procedures were performed to cut adhesions between sclera and conjunctiva.
Baseline data included age at surgery, sex, type, and duration of glaucoma diagnosis, average IOP at the last three preoperative measurements, number of antiglaucoma agents, and dosage of oral acetazolamide. Postoperative IOPs at years 1, 2, 3 and 4 were retrieved from medical records. Adverse events and the need for interventions, ie, needling or secondary surgical interventions (SSI), were also noted. Needling of the failing filtration bleb could be used in cases with bleb fibrosis or tenon cysts as a rescue procedure. Needling was not considered as an SSI.
Outcomes and Definitions
Primary outcome was a clinical success rate, either complete or partial success. Complete success was defined as achieving target IOP four years after XEN implantation, without any medical treatment or SSI (ie, incisional surgery, laser treatments), while partial success was defined as reaching target IOP with pharmacologic IOP-lowering treatment but without SSI. Four levels of target-IOP were analyzed (Table 2). All other patients not meeting success-criteria were defined as failure. In addition, stents which were obviously non-functioning, ie, broken or without physical connection with the anterior chamber, were classified as failure. Secondary outcomes were changes in IOP and number of IOP lowering agents compared to baseline.
Statistical Analysis
All eyes with available medical charts were included in the analysis, but eyes which were classified as failure prior to the endpoint were considered as failure even when lost to follow-up. Mean ± standard deviation (SD) or proportions (%) are given. For outcome at four-year follow-up, Chi-square test or one-way analysis of variance (ANOVA) with Dunnett’s post hoc test were used. Survival plots based on Kaplan–Meier estimates were generated for cumulative survival (probability of clinical success) and Cox proportional hazard ratio was calculated. A p<0.05 was considered statistically significant. All statistics were performed on IBM SPSS Statistics for Macintosh, version 25.0 (IBM Corp, Armonk, NY, USA).
Results
During the study period, a total of 139 XEN 45 gel stents were implanted. Of these, 20 eyes were excluded from this study because of previous glaucoma surgery, resulting in a study cohort of 119 eyes. At the study endpoint at four years, 103 datasets were still available since 5 patients were deceased and 11 were lost to follow-up (Figure 1).
At the time of surgery, the average age was 70.6 ±12.1 years. Gender was almost equally distributed. Most cases were either classified as primary open-angle glaucoma (46.6%) or pseudoexfoliative glaucoma (39.8%). Other types of glaucoma were rare, including secondary glaucoma after IOL-luxation, iridocyclitis, goniodysplastic glaucoma, previous angle closure glaucoma, venous stasis glaucoma and pigment dispersion glaucoma. The average duration of glaucoma, as defined from the time of diagnosis, prior to surgery was 9.2 years (Table 1). Mean preoperative IOP was 24.0 mmHg, ranging from 12.3 to 40.0 mmHg and the average number of pharmacologic IOP-lowering substances prior to surgery was 3.5 (range 0–6). At baseline, 54 eyes (52.4%) were pseudophakic. Antifibrotic agents were used in all cases. In 12 patients, both eyes were operated and included in the study. In 17 eyes, the target IOP was defined as lower than 20 mmHg (average 15 mmHg, range 12–18 mmHg). Overall, for the complete cohort, the average target IOP was 19.5 mmHg.
 |
Table 1 Demographic Description for Study Population with Four-Year Outcome |
Surgical Outcomes
Of 103 surgeries, 12 were combined with cataract surgery, while 91 were performed as stand-alone procedures. A total of 14 patients were bilateral cases. Previous analysis showed no correlation between first and second eye outcome, leading to the decision not to exclude the second eye in our analysis.15
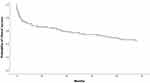
The overall success rate according to our individual IOP criteria was 43.7% (complete success 22.3%, partial success 21.4%). The success rate for different target IOP is shown in Table 2. The fastest decrease of success occurred during the first two months after surgery, as seen in a survival plot based on Kaplan–Meier estimates (Figure 2).
 |
Table 2 Outcome with Different Intraocular Pressure (IOP) Targets |
Accordingly, the failure rate was 56.3% (n=58). Of these, 45 cases (43.7%) have been subject for secondary glaucoma surgery at the study endpoint.
IOP reduction: In all eyes the mean IOP decreased from 24.0 mmHg at baseline to 16.0 mmHg (−33.3%), 15.1 mmHg (−37.1%), 15.1 mmHg (−37.1%) and 15.9 mmHg (−33.8%) at 1, 2, 3 and 4 years (p<0.001), respectively.
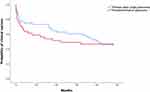
At the day of surgery, all medical glaucoma therapy was cancelled. For some patients, anti-glaucoma medication had to be reintroduced during the study period (Figure 3). Forty-five eyes underwent additional IOP-lowering procedures. The average number of substances was significantly reduced from 3.5 preoperatively to 1.5 at 4 years postoperatively, p<0.001 (ANOVA with Dunnett’s post hoc). Before surgery, 36 cases were treated with oral acetazolamide, at four-year follow-up, no patient was in need for this medication.
Type of Glaucoma
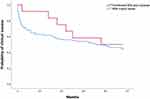
Cases with pseudoexfoliative glaucoma (PEX) showed an initial trend towards higher failure rates compared to simplex glaucoma (Figure 4), but this difference diminished over time and there was no significant detectable difference between these groups at the study endpoint (p=0.44).
Combined versus Stand-Alone Surgery
One year after surgery, combined cases seemed to have a more favorable outcome compared to stand-alone surgery (Figure 5), but this initial trend faded over time and there was no significant difference between the two groups at study endpoint (p=0.28).
Surgeon’s Impact
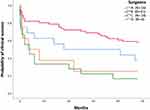
The outcome for the four surgeons involved in this study differed significantly (Table 3). The most productive surgeon had a clinical success rate of 55.7% (N=61) at four years, compared to 37.5% (N=16), 16.7% (N=18) and 25.0% (N=8), respectively, for lower-volume surgeons (Figure 6).
 |
Table 3 Stent misplacement and Final Failure Rates |
Second Eye Surgery
In 14 cases second eye surgery occurred. No statistical difference in outcome between first and second eye surgery was observed, failure rate was 54% in total (50% for first eye surgery, 57% for second eye surgery).
Complications
Misplacement
Of 103 stents, 73 (70.9%) were judged to be perfectly implanted with straight extraocular appearance and correct placement in relation to anterior chamber anatomy and length inside/outside the eye. Ten stents (9.7%) were seen with curved extraocular appearance indicating incarceration in subconjunctival tissues. Of these, 7 (70%) had failed at the study endpoint, 2 (20%) had partial success and one converted to complete success after intensive needling on five occasions.
A total of 20 stents (19.4%) were incorrectly implanted. Of these, 13 were entrapped in iris tissue, 3 too short externally, 3 too long externally (no contact with anterior chamber) and one stent was judged being in contact with endothelium (later explanted). Of these 20 stents, 16 (80%) had failed at the study endpoint (of these, 14 had secondary glaucoma surgery), three stents fulfilled the criteria for partial success and one for complete success (entrapped iris which resolved after YAG iridotomy).
Other Complications
The most common complications were temporary hypotony on the first postoperative day with IOP below 7 mmHg (n=16); persistent hypotony <7 mmHg was not observed, shallow anterior chamber (n=11) (iridocorneal contact was not observed) and choroidal detachment (n=14). Smaller hyphemas were often evident on day one postoperatively (n=18). Prolonged bleeding for more than one week was rare (n=2). All hyphemas resolved without surgical intervention. Other complications occurred seldomly (Table 4). No endophthalmitis or blebitis was observed. Only a few complications occurred after the first year: in two patients the visual field was completely lost, both patients had undergone secondary glaucoma surgery at that time. One late migration of XEN stent was observed, see case presentation below and Figure 7A–C. One surgical revision was necessary because of avascular conjunctiva. Surgical revision of encapsulated blebs was performed instead of needling in four cases, all of these were automatically classified as failure (secondary surgical intervention) regardless of outcome. In one of these cases, the XEN stent was accidentally damaged by surgical manipulation, and surgery converted to trabeculectomy in the same session. Late needling was performed in two cases, one leading to complete success, the other one a failure due to later cyclodiode laser treatment.
 |
Table 4 Complication Rates |
Case Presentation
One exceptional case demonstrates the potential of late needling even after several years: We would like to present the case of a female patient with bending of the functioning stent (Figure 7A). The inner stent lumen had been implanted adjacent to the iris surface, but its inner lumen was free as observed by gonioscopy, and filtration was observed, although the outer portion of the stent was bend. Three months after surgery, the stent migrated outside the anterior chamber, and a thin layer of iris tissue was observed overlying the inner stent lumen. IOP raised, which was treated with several IOP-lowering agents. Two years after surgery, occlusion of the entire stent lumen with agglomerated pigmented material and absence of filtration was documented (Figure 7B). In the meantime, the patient had even undergone cataract surgery. By manipulation in the slit lamp, the stent could be re-located some millimeter towards the anterior chamber two years after implantation, while the stent was straightened, and filtration restored by needling (Figure 7C). During the following year, the IOP was well controlled without medication. One year later, renewed stent migration towards the sclera led to complete failure (disconnection between inner stent lumen and anterior chamber).
Discussion
The basic surgical XEN stent implantation technique is relatively easy to learn for an experienced anterior segment surgeon. However, our data indicate that surgeons with higher volumes are more likely to achieve better results than low-volume surgeons. In our cohort, results between different surgeons varied significantly. We believe that this is not due to follow-up management, because most patients were treated by a variety of different surgeons after surgery. Aspects that may influence the surgical outcome are technique and choice of antimetabolite injection, positioning of the stent in relation to chamber angle structures and iris, adjustments of stent position under Tenons capsule and conjunctiva and primary needling of subconjunctival adhesions around the stent. Our study was not designed to determine which of these above-mentioned aspects that may play a crucial role for the outcome. Nevertheless, the high proportion of incorrectly positioned (n=20) and curved stents (n=10) indicate that high precision in stent positioning is crucial. The surgeon with the lowest rate of malpositioning also had the lowest rate of failure.
Some aspects of malpositioning were not yet known by the time of introduction of the XEN gel stent: curved stents can show normal filtration behavior during surgery and the first weeks after surgery. Primary needling, which is now the technique of choice to achieve a straight and freely mobile stent,17 was not launched in the beginning of this study. Even obliterated stents by iris incarceration can initially present with functioning filtration blebs by side-flow through the intrascleral implantation channel.
Short-Time Failure
Our survival plot demonstrates a rapid decline in function during the first weeks after surgery. We interpret this as being the result of partly insufficient implantation technique during the learning curve, as several implanted stents never came into proper function due to for instance stent damage or improper implantation, ie, iris incarceration. In our previous study, we were able to show that the initial 30 patients during the learning curve had a three times higher failure rate at one year post surgery than the following 30 patients by the same surgeon, indicating large improvement potential by experience.16
Long-Time Failure
Scar-formation and fibrosis are unlikely to occur during the first two weeks after surgery but are the main reason for declining success rate in the long term. Needling of fibrosis or Tenon cysts around the XEN gel stent ostium can resolve malfunction. In our cohort, 44 eyes (42%) underwent at least one needling procedure during the first six months after surgery. This is in line with other published cohorts; 43.0%, 36.6%, and 55.4%.12,18,19 Thereafter, needling was seldomly performed. In some cases, function of the stent could nevertheless be re-established a long time after surgery. Five cases were identified obtaining needling >12 months after surgery. Of these, two were converted from failure to complete success, two from partial success to complete success and one failed at the study endpoint.
In the systematic review of Chen et al, eight publications with 36 months of follow-up were identified, three of these with cohorts of more than 50 surgeries.14 Table 5 gives an overview over these together with our own data.
 |
Table 5 Comparison of Our Data at Four Years and Some of the Largest Studies with at Least Three Years of Follow-Up |
In comparison with these long-term publications, our population presented with a higher level of IOP and more extensive medication at baseline. This indicates differences in study populations (more advanced stage of glaucoma) and later surgical intervention in our study. The Scandinavian population is characterized by a high proportion of pseudoexfoliative glaucoma. In our cohort, PEX accounted for 39.8% of all cases, compared to 11.8%.9 However, our study could not detect any significant difference between PEX and primary open-angle glaucoma at the study endpoint. This is in line with most published results as summarized by Fea et al.20
A strength of the present study is that we report the results of a complete cohort over the duration of four years, while comparable studies have a significant reduction in number of cases over time (3-year-drop-out 52.4%9 and 74.1%10 respectively). Most researchers exclude failed cases after secondary glaucoma surgery, so that the results of the remaining study population appear to be more successful than the initial cohort. In short-term studies in which no patient is excluded from follow-up, the failure rate at 12 months can be as high as 51.4% in a population with difficult cases, with 60% previous incisional glaucoma surgery,21 which seems to be a realistic real-world result. To ensure the most comprehensive follow-up, cases with early failure were enclosed in the outcome, even if the patients later were lost to follow-up, thus leading to an overrepresentation of negative events.
A limitation of the present study is the retrospective study design. Follow-up was performed by multiple clinics, and the postoperative treatment was not standardized. No definition of success was established before surgery, thus leading to different interpretation of outcome and management of the patient’s medication. Some IOP-lowering effect may be caused by cataract surgery in combined cases. Caution should be taken with subgroup analysis, since it may lead to small subgroups with compromise of statistical power.
The present results are reported according to internationally recommended standards, although the criteria are not perfectly suited for a retrospective study approach. It is impossible to isolate the IOP-lowering effect of the XEN gel stent expressed in percentage as we compare preoperatively heavily treated IOP with post-surgery IOP under a significantly reduced medication. Thus, the demand of at least 20% IOP reduction can be too strict under certain circumstances. Some authors therefore extend the definition of success to include even cases with reduction of antihypertensive medication without an increase in baseline IOP.10
Conclusions
In summary, the present study demonstrates that XEN gel stent surgery is a safe small-incision-procedure which has the potential to lower IOP substantially. Patients should be informed about the potential need for postsurgical needling, medication and/or secondary surgical interventions to achieve target IOP. Only a minority of patients reach low IOP (<15 mmHg).
The majority of drop-out occurs during the first months after surgery and might be due to suboptimal placement of the stent. Outcomes can be maximized by correct placement of the stent both in relation to anterior chamber structures and subconjunctivally (primary needling). We recommend performing XEN stent surgery in a specialized glaucoma clinic with high volumes.
Funding
The study was financed by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (ALF-GBG-725041), Göteborg Medical Society, Dr Reinhard Marcuses Foundation, Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse, Hjalmar Svensson Foundation, Greta Andersson Foundation, Agneta Prytz-Folkes och Gösta Folkes stiftelse, De Blindas Vänner and Kronprinsessan Margaretas Arbetsnämnd för Synskadade.
Disclosure
TB and AB have received lecture fees and travel expenses from AbbVie. The authors report no other conflicts of interest in this work.
References
1. Coleman AL, Miglior S. Risk factors for glaucoma onset and progression. Surv Ophthalmol. 2008;53(Suppl 1):S3–10. doi:10.1016/j.survophthal.2008.08.006
2. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120(10):1268–1279. doi:10.1001/archopht.120.10.1268
3. Kass MA, Heuer DK, Higginbotham EJ, et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. doi:10.1001/archopht.120.6.701
4. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393(10180):1505–1516. doi:10.1016/S0140-6736(18)32213-X
5. Kirwan JF, Lockwood AJ, Shah P, et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology. 2013;120(12):2532–2539. doi:10.1016/j.ophtha.2013.07.049
6. Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153(5):804–814 e801. doi:10.1016/j.ajo.2011.10.024
7. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi:10.2147/OPTH.S80490
8. Chaudhary A, Salinas L, Guidotti J, Mermoud A, Mansouri K. XEN Gel Implant: a new surgical approach in glaucoma. Expert Rev Med Devices. 2018;15(1):47–59. doi:10.1080/17434440.2018.1419060
9. Reitsamer H, Vera V, Ruben S, et al. Three-year effectiveness and safety of the XEN gel stent as a solo procedure or in combination with phacoemulsification in open-angle glaucoma: a multicentre study. Acta Ophthalmol. 2021;100(1):e233–e245. doi:10.1111/aos.14886
10. Gabbay IE, Goldberg M, Allen F, et al. Efficacy and safety data for the Ab interno XEN45 gel stent implant at 3 Years: a retrospective analysis. Eur J Ophthalmol;2021. 11206721211014381. doi:10.1177/11206721211014381
11. Nicolaou S, Khatib TZ, Lin Z, et al. A retrospective review of XEN implant surgery: efficacy, safety and the effect of combined cataract surgery. Int Ophthalmol. 2022;42(3):881–889. doi:10.1007/s10792-021-02069-5
12. Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K. Combined and stand-alone XEN 45 gel stent implantation: 3-year outcomes and success predictors. Acta Ophthalmol. 2021;99(4):e531–e539. doi:10.1111/aos.14605
13. Buffault J, Baudouin C, Labbe A. XEN((R)) gel stent for management of chronic open angle glaucoma: a review of the literature. J Fr Ophtalmol. 2019;42(2):e37–e46. doi:10.1016/j.jfo.2018.12.002
14. Chen XZ, Liang ZQ, Yang KY, et al. The outcomes of XEN gel stent implantation: a systematic review and meta-analysis. Front Med. 2022;9:804847. doi:10.3389/fmed.2022.804847
15. Astrom S, Linden C. Incidence and prevalence of pseudoexfoliation and open-angle glaucoma in northern Sweden: i. baseline report. Acta Ophthalmol Scand. 2007;85(8):828–831. doi:10.1111/j.1600-0420.2007.00992.x
16. Busch T, Skiljic D, Rudolph T, Bergström A, Zetterberg M. Learning curve and one-year outcome of XEN 45 gel stent implantation in a Swedish population. Clin Ophthalmol. 2020;14:3719–3733. doi:10.2147/OPTH.S267010
17. Vera V, Sheybani A, Lindfield D, Stalmans I, Ahmed IIK. Recommendations for the management of elevated intraocular pressure due to bleb fibrosis after XEN gel stent implantation. Clin Ophthalmol. 2019;13:685–694. doi:10.2147/OPTH.S195457
18. Reitsamer H, Sng C, Vera V, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):983–996. doi:10.1007/s00417-019-04251-z
19. Gabbay IE, Allen F, Morley C, Pearsall T, Bowes OM, Ruben S. Efficacy and safety data for the XEN45 implant at 2 years: a retrospective analysis. Br J Ophthalmol. 2020;104(8):1125–1130. doi:10.1136/bjophthalmol-2019-313870
20. Fea AM, Durr GM, Marolo P, Malinverni L, Economou MA, Ahmed I. XEN((R)) gel stent: a comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020;14:1805–1832. doi:10.2147/OPTH.S178348
21. Thatcher MD, Coupal DJ, Cheng Y, Podbielski DW. Short-term efficacy and safety of open conjunctiva Ab externo XEN45 gel stent implantation in glaucoma patients. J Glaucoma. 2022;31(9):757–762. doi:10.1097/IJG.0000000000002064
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.