Back to Journals » International Journal of Nanomedicine » Volume 11
Formulation, characterization and tissue distribution of a novel pH-sensitive long-circulating liposome-based theranostic suitable for molecular imaging and drug delivery
Authors Duan Y, Wei L, Petryk J, Ruddy TD
Received 24 April 2016
Accepted for publication 30 July 2016
Published 1 November 2016 Volume 2016:11 Pages 5697—5708
DOI https://doi.org/10.2147/IJN.S111274
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Thomas Webster
Yin Duan,1,2 Lihui Wei,1–3 Julia Petryk,2,3 Terrence D Ruddy2,3
1Nordion Inc., 2Cardiac Positron Emission Tomography (PET) Radiochemistry Research Core Laboratory, Canadian Molecular Imaging Center of Excellence, University of Ottawa Heart Institute, 3Division of Cardiology, University of Ottawa Heart Institute, Ottawa, ON, Canada
Purpose: When designing liposome formulas for treatment and diagnostic purposes, two of the most common challenges are 1) the lack of a specific release mechanism for the encapsulated contents and 2) a short circulation time due to poor resistance to biological fluids. This study aimed to create a liposome formula with prolonged in vivo longevity and pH-sensitivity for cytoplasmic drug delivery.
Materials and methods: Liposomal particles were generated using hydrogenated soy (HS) phosphatidylcholine, cholesteryl hemisuccinate (CHEM), polyethylene glycol (PEG) and diethylenetriaminepentaacetic acid-modified phosphatidylethanolamine with film hydration and extrusion methods. The physicochemical properties of the different formulas were characterized. pH-sensitivity was evaluated through monitoring release of encapsulated calcein. Stability of the radiolabeled liposomes was assessed in vitro through incubation with human serum. The best formula was selected and injected into healthy rats to assess tissue uptake and pharmacokinetics.
Results: Liposomal particles were between 88 and 102 nm in diameter and negatively charged on the surface. Radiolabeling of all formulas with indium-111 was successful with good efficiency. 1%PEG-HS-CHEM not only responded to acidification very quickly but also underwent heavy degradation with serum. The 4%PEG-HS-CHEM, which exhibited both comparatively good pH-sensitivity (up to 20% release) and s.tisfactory stability (stability >70% after 24 h), was considered the best candidate for in vivo evaluation. Tissue distribution of 4%PEG-HS-CHEM was comparable to that of 4%PEG-HS-Chol, a long-circulating but pH-insensitive control, showing major accumulation in liver, spleen, intestine and kidneys. Analysis of blood clearance showed favorable half-life values: 0.6 and 14 h in fast and slow clearance phases, respectively.
Conclusion: 4%PEG-HS-CHEM showed promising results in pH-sensitivity, serum stability, tissue uptake and kinetics and is a novel liposome formulation for multifunctional theranostic applications.
Keywords: hydrogenated soy phosphatidylcholine, cholesteryl hemisuccinate, PEGylated liposome, pH-triggered release, long in vivo half-life
Introduction
The importance of nanotechnology to medical applications such as diagnosis and the delivery of therapeutic agents has received much recognition. Theranosis, a new interdisciplinary field in the realm of biomedical sciences, has the ultimate goal of forming optimized and personalized diagnostic and therapeutic strategies.1–3 The development of theranostic agents has greatly benefited from the advancement of micro- or nano-scale drug delivery and release mechanisms and from the progress made in diagnostic imaging.
Compared to platforms such as copolymers, dendrimers, micelles and metallic- and oxide-based nanoparticles, liposome-based theranostic carriers have received much attention due to their biodegradable nature, versatility in composition and ease of surface modification. Early exploration of liposomal nanoparticles as a type of drug delivery vehicle resulted in a few successful FDA-approved drug products.4 However, the development of liposomes for large-scale clinical applications has been met with two major challenges: rapid elimination by the reticuloendothelial system (RES) and inefficient drug release.5–8 Various strategies have been developed. The circulation time of liposomes in the bloodstream can be prolonged with the insertion of sterically stabilizing amphiphiles such as polyethylene glycol (PEG)-modified phospholipids.8–11 Fusogenic and/or pH-sensitive lipid combinations can be used to facilitate cytoplasmic delivery.8,10,12–21
Non-invasive imaging techniques such as single photon emission computed tomography (SPECT), positron emitting tomography (PET) and magnetic resonance imaging (MRI) have long been the go-to methods for diagnosis of diseases in cardiology, neurology and oncology. These imaging modalities often utilize radioactive or magnetic probes that target specific tissues or physiological processes, so that the molecular and cellular natures of disorders can be visualized.22,23 However, it is challenging to find multiple favorable qualities such as ease of fabrication and labeling, long circulating half-life, high labeling specificity, low imaging background and minimum toxicity in one single tracer molecule. Therefore, versatile drug delivery platforms are being developed and have shown promising and even superior characteristics over traditional diagnostic agents.
This study aimed to develop a liposome-based theranostic that combines an extended biological half-life, a pH-sensitive release mechanism and ready-to-label surface chelation chemistry. When considering the ingredients for the liposome formulations, we selected a group of lipids for their unique physicochemical nature. Hydrogenated soy phosphatidylcholine (HSPC), the major building block of our liposome formulas (57% in molar ratio), was chosen for its desirable stability due to its high transition temperatures (Tm =53°C).10 Cholesteryl hemisuccinate (CHEM), the hemisuccinate derivative of cholesterol (Chol), is a popular ingredient appearing in various pH-sensitive liposome constructs.8,10,19–21,24,25 Like other PEGylated lipids, PEG2000 conjugated distearoyl phosphatidylethanolamine (DSPE-PEG2000) has been proven to prolong the circulation of sterically stabilized liposomes usually at 5%–8% of molar ratio.10,11 Diethylenetriaminepentaacetic acid-derivatized DSPE (DSPE-DTPA) is a chelate-modified phospholipid that allows chelation to the metal tracers that enable imaging with SPECT, PET and MRI. The generated liposomes were characterized for physicochemical properties, resistance to serum degradation and ability to release encapsulated content upon acidification. One of the formulas was selected as the best candidate and injected into healthy rats and assessed for tissue distribution and clearance, in comparison to a non-pH-sensitive formula.
Materials and methods
Materials
HSPC, Chol, CHEM, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[methoxy(polyethylene glycol)-2000] (DSPE-PEG2000) and 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-diethylenetriaminepentaacetic acid (DSPE-DTPA) were purchased from Avanti Polar Lipids Inc (Alabaster, AL). Phosphate-buffered saline (PBS) pH 7.2 (1×) was obtained from Life Technologies (Burlington, ON, Canada). Chloroform, indium (III) chloride (InCl3), sodium acetate (NaOAc), trifluoroacetic acid and tetrabutylammonium phosphate (TBAP) were purchased from Sigma-Aldrich (St Louis, MO, USA). High-performance liquid chromatography (HPLC)-grade methanol (CH3OH), acetonitrile (CH3CN) and methylene chloride (CH2Cl2) were obtained from Thermo Fisher Scientific (Waltham, MA, USA). Radionuclide 111InCl3 in 0.05 M HCl solution was supplied by Nordion Inc (Ottawa, ON, Canada). Deionized and filtered water used in experiments was obtained through a Barnstead Nanopure Infinity water system (Dubuque, IA, USA). A Waters HPLC system (Milford, MA, USA) consisting of a 1525 Binary Pump, 717+ Autosampler, 2998 Photodiode Array Detector, 474 Scanning Fluorescence Detector, as well as a PerkinElmer Radiomatic Flow Scintillation Analyzer (Waltham, MA, USA) was used to assay the fluorometric and radiometric characteristics of different liposome formulas.
Preparation of liposomal nanoparticles
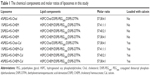
A Hashimoto® Automated Multifunctional Liposome Manufacturing Equipment (“liposome automaker” in the following texts) and a Hashimoto® Liposome Auto-Extruder (“liposome auto-extruder” in the following texts) were used in the preparation and extrusion of the liposome samples. A total of 60 μmol of lipid molecules in various ratios (Table 1) was first dissolved in a chloroform/methanol (10:1, v/v) mixture and pumped into the mixing tube of the liposome automaker, where it was then subjected to vortex action of 2,000 rpm at 60°C for 30 min under reduced pressure to form a thin lipid film. At the end of the lipid film formation, the organic solvent mixture was completely evaporated. A total of 6 mL of PBS with or without 80 mM calcein as solute (pH was re-adjusted to 7.4 after dissolution of calcein) was pumped into the mixing tube to mix with the lipid film under a vortex of 2,500 rpm at 60°C for 3 min to generate multilamellar vesicles (MLVs). The MLV suspension was later transferred into a sonicator where it received sonication for 20 min to form small unilamellar vesicles (SUVs). The sonication process was cooled to 4°C by a circulator to prevent over-heating. The finished SUV liposome was then centrifuged at 2,500× g for 10 min at 15°C, in order to precipitate the titanium (Ti) powder residue from the in-line coating of the sonicator. The supernatant was carefully removed and put under a second centrifugation (2,500× g, 5 min, 15°C) for further precipitation of Ti powder.
The Ti-free SUV liposome was first warmed up to 60°C in water bath and then injected into the auto-extruder for extrusion. Extrusion was carried out by passing the liposome suspension through membrane filters with five different pore sizes 800, 600, 400, 200 and 100 nm sequentially at room temperature. For the calcein-encapsulated liposomal nanoparticles, a centrifugation procedure was used to remove free calcein in the suspension: 0.5 mL of liposome aliquot was added to an Ultra-0.5 mL (30,000 MWCO) filtration device (Millipore, Billerica, MA, USA) and centrifuged at 14,000× g for 25–30 min at 15°C. The purified liposome was collected from the filter basket and brought back to original volume through dilution in 1× PBS. For the study, a total of eight different formulas of liposomes were generated, and their ingredients and ratios are listed in Table 1.
Size determination and characterization
Hydrodynamic diameters and polydispersity of liposomal particles were measured in ultrapure water through dynamic light scattering using a Malvern Nano ZS Zetasizer (Malvern, UK). Zeta potential values were measured in 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) buffer (final pH 7.2) using dip cells of the same Zetasizer. The electrode was cleaned between each measurement to guarantee accuracy.
Lipid recovery in liposome products
A small portion of lipid components was expected to be lost during the manufacturing and extrusion of liposomes. Therefore, the amounts of two major lipids phosphatidylcholine and Chol or CHEM in each liposome preparation were measured to determine how much of the lipids were in the final product. Freshly prepared liposome samples were analyzed with a Waters HPLC system that comprised a 1,525 Binary Pump, a 717 Autosampler and a 2,996 PDA Detector (Waters, Milford, MA, USA) equipped with a Phenomenex Luna C18(2) column (Torrance, CA, USA), using an ion-pair reversed phase method. Samples were dissolved in mobile phase CH2Cl2/CH3OH/CH3CN/H2O (200:560:180:60) modified with 15 mM TBAP and eluted at 1.6 mL per min. The UV absorbance at 225 nm was monitored. The identities and concentration of test lipids were determined by using chromatograms of pure lipid standards of various concentrations as reference.
Encapsulation efficiency of calcein
The amount of encapsulated calcein was measured following a reported method,8 using a Cary Eclipse fluorescence spectrophotometer (Agilent Technologies, Santa Clara, CA, USA) with λexc at 475 nm and λem at 510 nm. With an endoliposomal concentration of 80 mM, the fluorescence of calcein was self-quenched. When the liposomal structure is disrupted by detergent, the encapsulated calcein can escape and cause a spike in the fluorescence reading. The calcein-encapsulated liposome suspension was treated with Triton X-100 (0.1% w/w) to release all calcein. The effect of Triton X-100 was corrected by subtracting readings from non-Triton X-100-treated samples.
Calcein release
The pH-dependent leakage of liposomal calcein was measured using a modified method from the literature.8,20 Briefly, a 10 μL purified calcein-capsulated liposome sample was first diluted 100 times in HEPES buffers (10 mM HEPES, 140 mM sodium chloride) of acidic pH and a physiological pH of 7.2. pH 4.5 and 5.5 were used to imitate the endosomal pH environment to which liposomes are exposed to after internalization. The diluted samples were incubated at 37°C and under constant swirl at 400 rpm for 30, 60, 90, 120 and 180 min. Samples were then removed and measured in a fluorescence spectrophotometer with λexc at 475 nm and λem at 510 nm. Measurement of fluorescence was also taken at 0 min for each pH group for baseline. The total release of encapsulated calcein was determined following the steps above with the presence of Triton X-100 (0.1% w/w). The percentage of calcein release was calculated using the following equation:
Release (%) = ((IpH − I0)/(I100 − I0)) ×100 |
IpH represents the intensity measured at the certain test pH, I0 represents the baseline measurement and I100 represents the 100% release under the treatment of Triton X-100.
Surface radiolabeling and in vitro stability
A 450 μL aliquot of the non-calcein-doped liposome formulas was first diluted with 50 μL of 0.5 M NaOAc solution to adjust its pH to around 5.0. A 24 μL of 0.05 M HCl solution with 2 mCi (74 MBq) of 111InCl3 and 27 nmol of non-active InCl3 (as carrier) was added to the liposome suspension for radiolabeling. The reaction was incubated with 600 rpm mixing at 37°C for 1 h. The percentage of the radiochemical purity (%RCP) of 111In-labeled liposome was assessed with a Waters HPLC system (1525 Binary Pump and 717 Autosampler) connected to a Phenomenex BioSep S2000 SEC column (300×7.8 mm) and a PerkinElmer Radiomatic 150TR Flow Scintillation Counter. Samples were diluted and eluted in 1× PBS buffer at pH 7.2 at 1 mL per min. The radiomatic signal for 111In-liposomes appeared between 5.5 and 6.0 min, whereas any signal appearing in the later retention time was considered to be a fragment of 111In-labeled liposome or unbound 111In stripped off the liposome.
The stability of radiolabeled liposome was analyzed following a published method.26 An aliquot of 111In-liposomes was diluted with human serum (Thermo Fisher Scientific, Waltham, MA, USA) at two different ratios (2 and 0.5 μmol lipid/mL serum) and incubated at 37°C with continuous mixing for up to 48 h. The stability of 111In-liposomes was assayed with the same radio-HPLC method described earlier. At different times, a small volume of the incubation was removed and examined for the %RCP of the 111In-liposome in the sampled solution.
111In-Liposome tissue distribution
The use of animals in this study was conducted in accordance with the guidelines of the Canadian Council on Animal Care (CCAC) and with approval from the Animal Care Committee at the University of Ottawa. We studied the tissue uptake of 111In-labeled 4%PEG-HS-Chol and 4%PEG-HS-CHEM using male Sprague Dawley rats from Charles River Laboratories (Wilmington, MA, USA) weighing 357.8±45.4 g. An average dose of 1.307±0.279 mCi (48.4±10.3 MBq) of radiolabeled liposome suspension with specific activity at 5.2 mCi (192.4 MBq) per μmol lipid was injected into the animals (nine animals for each formula, three animals per time point) under sedation. Animals were allowed to recover from anesthesia before returning to regular housing. At each time point of 2, 24 and 48 h after the injection of the liposome, a group of three animals were euthanized and their tissues such as heart, liver, kidney, muscle, femur, spleen, blood, brain, intestine, lung, stomach, urine/bladder, testes and thyroid were extracted, weighed and analyzed for total gamma counts using a PerkinElmer Wizard3 2480 Automatic Gamma Counter. The tissue uptake was expressed as the percentage of injected dose per gram (%ID/g) or per organ (%ID). To study blood clearance of the 111In-labeled liposomes, rats (n=2 per formula) received an injection of ~0.1 mCi (3.7 MBq) of 111In labeled liposome with similar specific activity as the biodistribution study. At selected time points post injection (15, 30, and 60 min, 2, 4, 6, 24 and 48 h), blood samples were collected from the tail vein, weighed and measured for liposome-associated radioactivity. To determine the total activity in blood, the blood volume of each animal was estimated using the following equation: blood volume of rat (mL) =0.06× body weight (g) +0.77.27 Blood liposome content at 2, 24 and 48 h from tissue uptake experiments was pooled in the clearance analysis in order to achieve a larger sample size (n=5) at the respective time points.
Data analysis and statistics
Average values (mean) and corresponding standard deviation (SD) were calculated with Microsoft Excel (Redmond, WA, USA) expressed as mean ± SD, and the number of measurements or samples was expressed as n. Statistical analyses such as one-way analysis of variance (ANOVA) and Student’s t-test, and non-linear curve fitting were performed with Excel or GraphPad Prism 5 (GraphPad Software, La Jolla, CA, USA). In order to determine the statistical significance of differences between test groups and controls, we applied one-way ANOVA with matched measurement followed by Dunnett’s post hoc tests when analyzing the data from pH-induced calcein release and the serum stability challenge. The two-tailed Student’s t-test was used to compare characteristics between empty and calcein-loaded liposomes and uptake in selected tissues between liposome formulas. In all of our analyses, a P-value of <0.05 was considered to be statistically significant, whereas ns indicates not statistically significant.
Results
Physicochemical characterization of liposomal nanoparticles
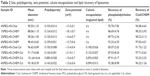
Highly homogeneous liposomal nanoparticles were produced with expected physical and chemical parameters (Table 2). The mean size of liposomal particle ranged from 88 to 102 nm. Calcein encapsulation did not result in significant alteration in particle diameter or polydispersity (P>0.05). The zeta potential assay showed that all particles bear negative surface charges, and again no differences were observed between formulas with and without calcein (P>0.05). Two major lipid components phosphatidylcholine and Chol/CHEM were measured in the final liposome products. Among all formulas, the rate of recovery of HSPC ranged from 85% to 96%, whereas Chol/CHEM ranged from 92% to 98%. No statistical difference was observed with the incorporation of calcein (P>0.05). All four calcein-encapsulated formulas showed comparable encapsulation efficiency.
pH-dependent calcein release
The calcein leakage of liposomal nanoparticles in acidic solutions and physiological pH was evaluated (Figure 1). While the pH-insensitive formula 4%PEG-HS-Chol-Cal released no more than 10% of its encapsulated content (Figure 1D), the three CHEM-based liposome formulas demonstrated 20% or more release in response to an acidic environment over a period of 180 min (Figure 1A–C). With only 1% PEGylated lipid, 1%PEG-HS-CHEM-Cal released 13%–14% of its calcein content at 30 min, whereas release from 2% and 4%PEG-HS-CHEM-Cal appeared more gradual. At the physiological pH, 1%PEG-HS-CHEM-Cal had an initial release of 13%, almost doubling that of 2% and 4%PEG-HS-CHEM-Cal, indicating its innate instability and tendency to leak out its content. Under acidic pHs, the three CHEM-based liposome showed significant increase of release over time (P<0.05). The pattern of release by the same liposomes at pH 7.2, however, showed no significant increase (P>0.05). Therefore, 1%, 2% and 4%PEG-HS-CHEM-Cal were responsive to acidification of their environment. Unlike the CHEM-based liposomes, 4%PEG-HS-Chol-Cal exhibited no pH-sensitivity given its identical release trend at each of the three pH conditions.
111Indium labeling and in vitro radiolabeling stability
High RCP was achieved without purification post radiolabeling: 4%PEG-HS-Chol at 100.0%±0.0%, 4%PEG-HS-CHEM at 98.0%±1.9%, 2%PEG-HS-CHEM at 98.5%±2.7% and 1%PEG-HS-CHEM at 98.2%±0.7%.
The influence of lipid composition on serum stability is presented in Figure 2. As the well-known sterically stable lipid combination, the Chol-based formula 4%PEG-HS-Chol retained 93.3%±4.5% (2 μmol lipid/mL serum) and 83.8%±12.3% (0.5 μmol lipid/mL serum) of its integrity (as the measurement of RCP) at 24 h (Figure 2D). The three CHEM-based liposome formulas, however, underwent various degrees of degradation (Figure 2A–C) (P<0.05 versus PBS control). After a 24-hour incubation, the stability of 111Inlabeled 4%PEG-HS-CHEM dropped to 27% at 2 μmol lipid/mL serum and 39% at 0.5 μmol lipid/mL serum. With lower molar ratio of PEGylated lipid, 1% and 2%PEG-HS-CHEM had a more pronounced decline in stability, having merely one-third and a quarter of their starting RCP after 24 h. Results from incubation in PBS solution revealed that irrespective of the lipid composition, all 111In-labeled liposomes remained stable for as long as 24 h.
Biodistribution and blood clearance of 111In-labeled liposomes
Out of the three CHEM-based pH-sensitive formulas, 4%PEG-HS-CHEM was selected to proceed with the tissue distribution and clearance study, due to its better stability with serum compared to 1% and 2%PEG-HS-CHEM.
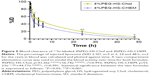
The uptake results of 4%PEG-HS-CHEM and 4%PEG-HS-Chol are presented in Table 3. The two formulas demonstrated similar tissue distribution (Figure 3A and B). Both 111In-labeled liposomes had highest uptake in the spleen, reaching close to 5%ID/g at 24 h and remaining unchanged at 48 h, while there was less accumulation of the activity in the liver, intestine, kidneys, heart and lungs. The blood activity concentration of both formulas was highest at 2 h post injection at ~2%ID/g, and then dropped at 24 h. Change in tissue uptake over time suggested both formulas were able to remain in the circulation system at early time points post injection and were later removed from the blood by the spleen and liver, a result comparable to existing reports of liposomes of similar compositions.28 We also identified the major organs of accumulation and/or catabolism as the liver, spleen, intestine and kidneys (Figure 4A–D). At 24 h post injection, the liver accounted for the accumulation of 12% of 4%PEG-HS-Chol and 10% of 4%PEG-HS-CHEM; 4%–6% of liposome-associated activity was found in the spleen and intestine. Compared to its Chol-based counterpart, 111In-labeled 4%PEG-HS-CHEM had significantly less accumulation in all examined tissues (lung, liver, kidneys and blood [P<0.05 or less]) except for the spleen (P>0.05). The clearance of both liposome formulas from blood circulation is illustrated in Figure 5. A two-compartment exponential decay model was fitted to estimate the biological half-life for the two liposomes (Table 4). The 4%PEG-HS-Chol had a 0.9 h half-life in fast-phase clearance and a 15 h half-life in slow-phase clearance. The clearance of pH-sensitive 4%PEG-HS-CHEM was only slightly faster, with a 0.6 h fast half-life and a 14 h slow half-life.
Discussion
This study represents our first development of a novel liposome-based theranostic agent that combines targeted drug delivery and molecular imaging applications. The 1%, 2% and 4%PEG-HS-CHEM exhibited the capability of pH-induced release in response to acidification of the external environment. Among the three CHEM-based liposome formulas, we found that the 4% molar PEG-lipid anchor conferred the best stability to the liposomes when incubated with human serum. Our tissue distribution study revealed that 4%PEG-HS-CHEM had moderate accumulation in the liver and spleen and little uptake in the lungs, heart, intestine and kidneys. About 55% of the CHEM-based liposome cleared during the fast clearance phase and the remainder cleared in the slow phase. Overall, our liposome formula 4%PEG-HS-CHEM demonstrated great potential for theranostic applications. To further prove their suitability, tissue-based uptake and animal imaging studies are warranted. Depending on the intended applications, our CHEM-based liposome formulas would require extra modifications to further enhance their targeting ability and stability, to allow them to carry other imaging agents and to promote their responsiveness and/or drug release efficiency.
Potential applications of theranostics include image-guided drug delivery, imaging drug release, monitoring therapeutic outcomes, delivering radiation therapy and image-guided surgery.3 The recent development of liposome-based theranostics holds the potential to personalize treatments, decrease invasiveness in diagnosis and therapy and monitor therapeutic outcomes in real time.1,2,29
The imaging function requires the labeling of theranostic carriers with radioactive or non-radioactive isotopes on the bilayer surface or through encapsulation. While some prefer the design that shields the imaging elements from the outer biological environment, others appreciate surface chelation for its versatility in the choice of radionuclides and its high labeling efficiency. Early surface-labeling studies tagged liposomes with technetium-99m via non-specific ionic attraction, but the radionuclides quickly dissociated once the carriers were injected into humans.30 To better retain the imaging metal isotopes, many tried incorporation of chelate–phospholipid derivatives into the liposome formulation that enables surface chelation of metal cations. Seo et al31–33 experimented with copper cation-specific bifunctional chelators (BFCs) such as 6-[p-(bromoacetamido)benzyl]-1,4,8,11-tetraazacyclotetradecane-N, N′, N″, N″′-tetraacetic acid, (6-(6-(3-(2-pyridyldithio)propionamido)hexanamido)benzyl)-1,4,8,11-tetraazacyclotetradecane-1,4,8,11-tetraacetic acid, 4-(2-(2-pyridyldithioethyl)ethanamido)-11-carboxymethyl-1,4,8,11-tetraazabicyclo(6.6.2)hexadecane, as well as distearoyl and dipalmitoyl maleimide lipids serving as the base for BFCs, in order to generate copper-64 surface-labeled liposomes for PET imaging and therapy monitoring. Other chelate–isotope combinations such as indium-111 and DTPA,26,34,35 technetium-99m (in the form of pertechnetate) and hydrazine nicotinamide36,37 have also been assessed and proven feasible for creating stable liposomes for SPECT imaging. We selected DTPA-derivatized phospholipid for our liposome formulation due to its known versatility in chelating metal of different imaging modalities. Helbok et al38 synthesized PEG-modified DTPAderivative-based liposomes that are suitable for labeling with several metallic trivalent ions such as indium-111 (SPECT), technetium-99m-CO3 (SPECT), lutetium-177 (radiotherapy) and gallium-68 (PET) with high RCP and specific activity. DTPA derivatization also showed potential for MRI when chelated with gadolinium.30
Another important aspect of theranostic carriers, especially in the context of image-guided drug delivery, is the delivery and release mechanism. PEGylated and other polymer/copolymer-based lipid anchors have been extensively used to avoid clearance by the RES and to prolong blood circulation. To overcome the lack of drug release from liposomal particles, stimuli-specific release mechanisms have been added to improve the bioavailability of encapsulated therapeutics at the target tissues. The types of stimuli include light,39 pH,13,14 enzymatic degradation40 and gain or loss of heat.12,41,42 Previous approaches to generate pH-sensitive liposomes using CHEM in conjunction with various lipids have been reported. At physiological pH, the lipid combinations such as egg PC/dimethyldioctadecylammonium bromide/CHEM,18 egg PC/oleyl alcohol/CHEM19 and diolein/CHEM25 conferred net negative charges to liposomal particles and maintained a stable bilayer. Once placed under acidic pH, the weakly anionic and/or cationic amphiphilic lipids within the bilayer became partially protonated, causing the liposomes to undergo rapid aggregation and membrane fusion due to the removal of electrostatic colloidal stabilization.24,43 However, for the pH-sensitive liposome, decrease in pH-responsiveness has been observed as the molar ratio of PEGylated lipid anchor or the size of PEG group increased,8,20,44,45 creating a stability–pH-sensitivity dilemma. Observations of our PEGylated CHEM-based liposomes reflect this same conundrum.
Strategies to enable slow clearance and more efficient drug release would improve our current design. Xu et al utilized poly(2-ethyl-2-oxazoline)(PEtOz), a substitute for conventional PEG-derivatized phospholipids, in their liposome applications. They demonstrated that PEtOz-modified liposomes were not only more sensitive to an acid pH environment than conventional PEGylated liposomes but also demonstrated favorable stability in both in vitro and in vivo experiments.46 Adding extra releasing mechanisms is also considered crucial for promoting drug delivery. For instance, magnetically and pH dual responsive dendrosomes were created by incorporating magnetic nanoparticles and folate-targeted dendrimers inside PEG-modified 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine/CHEM liposomes.47 These dual-sensitive carriers demonstrated enhanced release of encapsulated dendrimer–rhodamine conjugate upon exposure to acidic environment and magnetic field. Li et al constructed a type of pH and esterase–dual-sensitive liposome complex. To form the lipoplexes, zwitterionic polymer poly(carboxybetaine) was conjugated with chemotherapy drug camptothecin via an ester bond that is cleavable under low acid pH and by esterase. The lipoplexes were capable of releasing camptothecin in a sustained manner in response to pH and esterase in both in vitro and in vivo assessment.40
Conclusion
In this study, we investigated liposomes of different compositions in order to identify an optimal formula that is capable of cytoplasmic delivery of therapeutic agents and prolonged circulation in the blood stream. Our novel liposome formula 4%PEG-HS-CHEM demonstrated satisfactory serum stability, suitable pH-responsiveness, high radiolabeling efficiency with 111In, slow blood clearance and moderate to little uptake in major organs. These are all considered to be favorable features of a theranostic vehicle.8
Acknowledgments
The authors would like to thank Dr Shubing (Steve) Zhao and Professor Warren C W Chan for conducting the characterization of our liposome samples. We would also be grateful to Dr Eric Rentschler and Hashimoto Electronic Industry Co., Ltd, for kindly providing us liposome automaker and liposome auto-extruder.
Disclosure
Yin Duan was an employee of Nordion Inc. during this study, but he is no longer with the organization; Lihui Wei is an employee of Nordion Inc. The authors report no other conflicts of interest in this work.
References
Chakravarty R, Hong H, Cai W. Positron emission tomography image-guided drug delivery: current status and future perspectives. Mol Pharm. 2014;11(11):3777–3797. | ||
Chakravarty R, Hong H, Cai W. Image-guided drug delivery with single-photon emission computed tomography: a review of literature. Curr Drug Targets. 2015;16(6):592–609. | ||
Terreno E, Uggeri F, Aime S. Image guided therapy: the advent of theranostic agents. J Control Release. 2012;161(2):328–337. | ||
Barenholz Y. Doxil(R) – the first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160(2):117–134. | ||
Straubinger RM, Hong K, Friend DS, Papahadjopoulos D. Endocytosis of liposomes and intracellular fate of encapsulated molecules: encounter with a low pH compartment after internalization in coated vesicles. Cell. 1983;32(4):1069–1079. | ||
Huang A, Kennel SJ, Huang L. Interactions of immunoliposomes with target cells. J Biol Chem. 1983;258(22):14034–14040. | ||
Dijkstra J, Van Galen M, Scherphof GL. Effects of ammonium chloride and chloroquine on endocytic uptake of liposomes by Kupffer cells in vitro. Biochim Biophys Acta. 1984;804(1):58–67. | ||
Slepushkin VA, Simões S, Dazin P, et al. Sterically stabilized pH-sensitive liposomes. Intracellular delivery of aqueous contents and prolonged circulation in vivo. J Biol Chem. 1997;272(4):2382–2388. | ||
Lasic DD, Vallner JJ, Working PK. Sterically stabilized liposomes in cancer therapy and gene delivery. Curr Opin Mol Ther. 1999;1(2):177–185. | ||
Simoes S, Moreira JN, Fonseca C, Duzgunes N, de Lima MC. On the formulation of pH-sensitive liposomes with long circulation times. Adv Drug Deliv Rev. 2004;56(7):947–965. | ||
Woodle MC. Sterically stabilized liposome therapeutics. Adv Drug Deliv Rev. 1995;16(2–3):249–265. | ||
Chen D, Sun K, Mu H, et al. pH and temperature dual-sensitive liposome gel based on novel cleavable mPEG-Hz-CHEMS polymeric vaginal delivery system. Int J Nanomedicine. 2012;7:2621–2630. | ||
Chen Y, Sun J, Lu Y, et al. Complexes containing cationic and anionic pH-sensitive liposomes: comparative study of factors influencing plasmid DNA gene delivery to tumors. Int J Nanomedicine. 2013;8:1573–1593. | ||
Karanth H, Murthy RSR. pH-Sensitive liposomes-principle and application in cancer therapy. J Pharm Pharmacol. 2007;59(4):469–483. | ||
Kono K, Igawa T, Takagishi T. Cytoplasmic delivery of calcein mediated by liposomes modified with a pH-sensitive poly(ethylene glycol) derivative. Biochim Biophys Acta. 1997;1325(2):143–154. | ||
Momekova D, Rangelov S, Yanev S, et al. Long-circulating, pH-sensitive liposomes sterically stabilized by copolymers bearing short blocks of lipid-mimetic units. Eur J Pharm Sci. 2007;32(4–5):308–317. | ||
Sawant RM, Hurley JP, Salmaso S, et al. “SMART” drug delivery systems: double-targeted pH-responsive pharmaceutical nanocarriers. Bioconjug Chem. 2006;17(4):943–949. | ||
Shi G, Guo W, Stephenson SM, Lee RJ. Efficient intracellular drug and gene delivery using folate receptor-targeted pH-sensitive liposomes composed of cationic/anionic lipid combinations. J Control Release. 2002;80(1–3):309–319. | ||
Sudimack JJ, Guo W, Tjarks W, Lee RJ. A novel pH-sensitive liposome formulation containing oleyl alcohol. Biochim Biophys Acta. 2002;1564(1):31–37. | ||
Vanic Z, Barnert S, Suss R, Schubert R. Fusogenic activity of PEGylated pH-sensitive liposomes. J Liposome Res. 2012;22(2):148–157. | ||
Xu H, Deng Y, Chen D, et al. Preparation and characterization of pH-sensitive vesicles made of cholesteryl hemisuccinate. Drug Dev Ind Pharm. 2008;34(2):134–141. | ||
Ametamey SM, Honer M, Schubiger PA. Molecular imaging with PET. Chem Rev. 2008;108(5):1501–1516. | ||
Mariani G, Bruselli L, Kuwert T, et al. A review on the clinical uses of SPECT/CT. Eur J Nucl Med Mol Imaging. 2010;37(10):1959–1985. | ||
Hafez IM, Cullis PR. Cholesteryl hemisuccinate exhibits pH sensitive polymorphic phase behavior. Biochim Biophys Acta. 2000;1463(1):107–114. | ||
Guo W, Gosselin MA, Lee RJ. Characterization of a novel diolein-based LPDII vector for gene delivery. J Control Release. 2002;83(1):121–132. | ||
Mougin-Degraef M, Bourdeau C, Jestin E, et al. Doubly radiolabeled liposomes for pretargeted radioimmunotherapy. Int J Pharm. 2007;344(1–2):110–117. | ||
Lee HB, Blaufox MD. Blood volume in the rat. J Nucl Med. 1985;26(1):72–76. | ||
Goins BA. Radiolabeled lipid nanoparticles for diagnostic imaging. Expert Opin Med Diagn. 2008;2(7):853–873. | ||
Shapiro B, Kulkarni S, Nacev A, Muro S, Stepanov PY, Weinberg IN. Open challenges in magnetic drug targeting. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2015;7(3):446–457. | ||
Torchilin VP, Trubetskoy VS. In vivo visualizing of organs and tissues with liposomes. J Liposome Res. 1995;5(4):795–812. | ||
Seo JW, Mahakian LM, Kheirolomoom A, et al. Liposomal Cu-64 labeling method using bifunctional chelators: poly(ethylene glycol) spacer and chelator effects. Bioconjug Chem. 2010;21(7):1206–1215. | ||
Seo JW, Qin S, Mahakian LM, Watson KD, Kheirolomoom A, Ferrara KW. Positron emission tomography imaging of the stability of Cu-64 labeled dipalmitoyl and distearoyl lipids in liposomes. J Control Release. 2011;151(1):28–34. | ||
Seo JW, Zhang H, Kukis DL, Meares CF, Ferrara KW. A novel method to label preformed liposomes with 64Cu for positron emission tomography (PET) imaging. Bioconjug Chem. 2008;19(12):2577–2584. | ||
Holmberg E, Maruyama K, Litzinger DC, et al. Highly efficient immunoliposomes prepared with a method which is compatible with various lipid compositions. Biochem Biophys Res Commun. 1989;165(3):1272–1278. | ||
Rauscher A, Frindel M, Maurel C, et al. Influence of pegylation and hapten location at the surface of radiolabelled liposomes on tumour immunotargeting using bispecific antibody. Nucl Med Biol. 2014;41:e66–e74. | ||
Brouwers A, De Jong D, Dams E, et al. Tc-99m-PEG-liposomes for the evaluation of colitis in Crohn’s disease. J Drug Target. 2000;8(4):225–233. | ||
Laverman P, Brouwers AH, Dams ET, et al. Preclinical and clinical evidence for disappearance of long-circulating characteristics of polyethylene glycol liposomes at low lipid dose. J Pharmacol Exp Ther. 2000;293(3):996–1001. | ||
Helbok A, Decristoforo C, Dobrozemsky G, et al. Radiolabeling of lipid-based nanoparticles for diagnostics and therapeutic applications: a comparison using different radiometals. J Liposome Res. 2010;20(3):219–227. | ||
Melancon MP, Zhou M, Li C. Cancer theranostics with near-infrared light-activatable multimodal nanoparticles. Acc Chem Res. 2011;44(10):947–956. | ||
Li Y, Liu R, Yang J, Ma G, Zhang Z, Zhang X. Dual sensitive and temporally controlled camptothecin prodrug liposomes codelivery of siRNA for high efficiency tumor therapy. Biomaterials. 2014;35(36):9731–9745. | ||
Yarmolenko PS, Zhao Y, Landon C, et al. Comparative effects of thermosensitive doxorubicin-containing liposomes and hyperthermia in human and murine tumours. Int J Hyperthermia. 2010;26(5):485–498. | ||
de Smet M, Langereis S, van den Bosch S, et al. SPECT/CT imaging of temperature-sensitive liposomes for MR-image guided drug delivery with high intensity focused ultrasound. J Control Release. 2013;169(1–2):82–90. | ||
Hafez IM, Ansell S, Cullis PR. Tunable pH-sensitive liposomes composed of mixtures of cationic and anionic lipids. Biophys J. 2000;79(3):1438–1446. | ||
Zignani M, Drummond DC, Meyer O, Hong K, Leroux J-C. In vitro characterization of a novel polymeric-based pH-sensitive liposome system. Biochim Biophys Acta. 2000;1463(2):383–394. | ||
Hong M-S, Lim S-J, Oh Y-K, Kim C-K. pH-sensitive, serum-stable and long-circulating liposomes as a new drug delivery system. J Pharm Pharmacol. 2002;54(1):51–58. | ||
Xu H, Hu M, Yu X, et al. Design and evaluation of pH-sensitive liposomes constructed by poly(2-ethyl-2-oxazoline)-cholesterol hemisuccinate for doxorubicin delivery. Eur J Pharm Biopharm. 2015;91:66–74. | ||
Wang M, Li J, Li X, et al. Magnetically and pH dual responsive dendrosomes for tumor accumulation enhanced folate-targeted hybrid drug delivery. J Control Release. 2016;232:161–174. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.