Back to Journals » Patient Preference and Adherence » Volume 17
Factors Influencing the Choice of Automated Peritoneal Dialysis Treatment by Patients Receiving Home Peritoneal Dialysis
Authors Cao F, Hong F, Ruan Y, Lin M
Received 29 May 2023
Accepted for publication 18 October 2023
Published 3 November 2023 Volume 2023:17 Pages 2797—2804
DOI https://doi.org/10.2147/PPA.S423443
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jongwha Chang
Fang Cao,1,2 Fuyuan Hong,1 Yiping Ruan,1 Miao Lin1
1Department of Nephrology, Provincial Clinical College, Fujian Medical University, Fujian Provincial Hospital, Fuzhou, 350001, People’s Republic of China; 2Department of Nursing, Provincial Clinical College, Fujian Medical University, Fujian Provincial Hospital, Fuzhou, Fujian, 350001, People’s Republic of China
Correspondence: Fang Cao; Miao Lin, Department of Nephrology, Provincial Clinical College, Fujian Medical University, Fujian Provincial Hospital, 134 East Street, Fuzhou, 350001, People’s Republic of China, Tel +86-591-87557768, Email [email protected]; [email protected]
Objective: This study was conducted to understand the influencing factors for home peritoneal dialysis patients choosing APD and to provide a scientific basis for improving the completion rate of APD treatment and the follow-up of peritoneal dialysis patients.
Methods: The study was a cross-sectional questionnaire-based study. A total of 588 patients on peritoneal dialysis were randomly selected from 6 regions in Fujian Province in southern China using a stratified cluster sampling method.
Results: The mean age of the patients were 56.5 ± 14.73 years. In the univariate analysis, knowledge, user experience and family support were the factors that affected patients’ choice of APD (all P < 0.05) and were positively correlated with the treatment utilization rate. In the multivariate analysis, 3 factors (treatment with APD, knowledge of APD, and family support) remained significantly associated not choosing APD. The selection rate for APD was 2.594 times higher among patients who had received APD than among patients who had never received APD. The selection rate for patients with “a lot of knowledge” about APD was 10.75 times that of patients with “no knowledge”.
Conclusion: Patients’ knowledge of APD, experience in application and family support were the main factors affecting the choice of APD as a treatment mode (P < 0.05) and were positively correlated with the treatment utilization rate. Further studies are needed to improve the APD treatment completion rates by modulation the above-mentioned factors.
Relevance to Clinical Practice: This study provides scientific evidence for improving APD treatment completion rates and improving patient quality of life.
Keywords: peritoneal dialysis, APD, dialysis mode, influencing factors, follow up, end-stage kidney disease
Background
Peritoneal dialysis (PD) is an effective way to treat end-stage kidney disease at home. The purpose of post-dialysis nursing is to reduce the incidence of dialysis complications and improve the quality of life.1,2 Automated peritoneal dialysis (APD) has outstanding advantages over continuous ambulatory peritoneal dialysis (CAPD) in public emergencies, such as earthquakes, wars, and traffic control. It can reduce the medical expenses and complication rates for patients while improving treatment effects.3 APD is a dialysis treatment method that uses a peritoneal dialysis machine for automatic peritoneal dialysis fluid exchange. Before resting at night, the peritoneal dialysis catheter is connected to the machine, and the dialysis parameters are set. The dialysis machine automatically completes the infusion and drainage of dialysis fluid. A computer system records all dialysis parameters, such as infusion volume, ultrafiltration volume, and drainage time. After dialysis, the data are automatically uploaded to the cloud. Automatic peritoneal dialysis offers additional advantages over CAPD, such as greater control of fluids, less risk of infection and now closer surveillance through telemedicine devices, which reduces complications.4,5 APD can reduce the treatment burden for both patients and medical staff.6 APD is simple and safe, provides therapy during sleep, improves dialysis adequacy, and improves the clinical effectiveness and the overall quality.7,8
APD is very common worldwide and is favoured by patients.9 Previous studies have shown that 40% of peritoneal patients worldwide receive APD. However, less than 2% receive APD treatment in China. In Fujian Province in southern China, only approximately 1.5% of patients receive APD, a percentage that is lower than the national average of 1.9%. The potential factors influencing the selection of APD may include the following: (1) contraindications to the use of APD in patients with recurrent abdominal infections; (2) Patients with mental illness or obvious physical defects; (3) socio-economic factors and machine performance, etc. This study was conducted to understand the influencing factors for home peritoneal dialysis patients choosing APD, and then to provide a scientific basis for improving the completion rate of APD treatment during the follow-up of peritoneal dialysis patients. It may facilitate effective measures and suggestions for PD patient education.
Participants and Methods
Participants
Fujian Province in southern China was divided into 6 regions (eastern Fujian, western Fujian, northern Fujian, southern Fujian, central Fujian, and Fuzhou), and 1 city (district) was randomly selected from each region. The names of counties and cities in the classified regions were put into envelopes. An assistant randomly selected one of the envelopes. Using a stratified cluster sampling method, 588 patients undergoing home peritoneal dialysis were selected from 6 cities (districts) (Table 1). There were 283 patients (48.13%) in the Fuzhou, 53 patients (9.01%) in the eastern Fujian, 78 patients (13.27%) in the western Fujian, 46 patients (7.82%) in the northern Fujian and 85 patients (14.46%) in the central Fujian. The process of cluster sampling can be divided into the following steps: (1) The researchers identified the total population as peritoneal dialysis patients in Fujian province; (2) We divided Fujian Province into 6 non-overlapping regions and marked them. Each region is a small group; (3) The ratio of the total number of patients in each region to the total number of patients in Fujian Province was set as A1, and the estimated total number of samples was multiplied by A1 to obtain the estimated number of samples of patients in each subgroup at least. The inclusion criteria were as follows: (1) Regular peritoneal dialysis treatment ≥3 months; (2) communicate normally and understand the purpose of the investigation. Exclusion criteria included: (1) do not know the name of automated peritoneal dialysis mode; (2) peritoneal dialysis combined with hemodialysis.
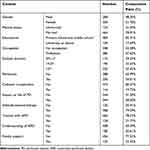 |
Table 1 Baseline Characteristics of Study Patients |
Methods
Study Design
Before the survey, the researchers invited relevant experts to conduct special training for the investigators, focusing on questionnaire survey technology and quality control during the survey process. Through questionnaire quality control, 588 valid questionnaires were retrieved. Sample size calculation: This study includes general data, APD has 2 dimensions and 40 items, and 5 to 10 times of variables are the sample size. The minimum sample size required for this study is 40×5=200, and the maximum sample size is 400. Considering the sample loss rate of 20%, 200×20%=40, the total sample size included is at least 240–480 patients.
We obtain the consent of each patient before the investigation and sign an informed consent form. The study procedure was approved by the Ethics Committee of Fujian Provincial Hospital (K2021-03-026). Participants provided written informed consent, and the study was conducted in accordance with the Declaration of Helsinki.
Questionnaires
A questionnaire was designed by the researchers, and the items were developed by the research team after reading a large number of publications, after a discussion with a nephrology professional group, and after consultation with relevant experts in the field of peritoneal dialysis in the province. The research team uses “Delphi” method to compile the questionnaire, and tests the reliability and validity of the questionnaire. The preparation process of the first draft of the questionnaire is as follows: (1) Establishment of a research group: The research group consists of 5 members, including 1 professor, 2 PHDS, and 1 supervisor for postgraduate students; (2) The research team is responsible for searching and analysing literature, conducting in-depth interviews to determine articles, drafting consultation questionnaires and selecting consulting experts, and conducting data collection and statistical analysis. (3) A total of 12 experts were invited, and the research team discussed and decided to modify the items of the scale based on the expert opinions. (4) The final version of the initial survey questionnaire, a total of 40 items in 2 dimensions. The content included general information (such as social and demographic characteristics of PD patients), patients’ current treatment patterns, complications, APD experience, and family support. Select Yes or No for the questionnaire.
The reliability and validity of the scale were tested in the outpatient follow-up of peritoneal dialysis patients, and the Cronbach’s α coefficient of the scale as a whole was 0.831. Cronbach’s α coefficients of each dimension ranged from 0.816 to 0.825.
Data Collection
Patients fill in the questionnaire through interviews or star scan codes, and multi-center researchers unify guidelines to explain the purpose, content and process of the study to the study subjects, as well as the methods and precautions to fill in the questionnaire, so as to ensure that patients can understand the contents of the questionnaire and complete the questionnaire. Obtain their consent and sign informed consent. Patients filled in the questionnaire independently on their mobile phones to ensure the authenticity of the results; If you have any questions, you can consult the researchers immediately and submit them on site. Researchers should pay attention to check the data to see if there are invalid answers and avoid mistakes. Researchers use two-person data entry board, check the original questionnaire immediately if any problem is found, and correct the input errors to ensure the correct data. The database is managed by the study leader and only members of the research team have access to the survey data.
Statistical Analysis
Data analysis was performed using SPSS version 23.0. Categorical variables were expressed as number(%). Continuous variables are expressed as the mean ± standard deviation. The χ2 test was used to compare the differences in categorical data between different groups, and multiple logistic regression analysis was used to identify correlations between the selection rate and influencing factors. P ≤ 0.05 was considered statistically significant.
Results
Patient Demographics, APD Administration, and Follow-Up
Sociological and demographic characteristics, treatment patterns, complications, APD use experience, family support status, and follow-up locations were investigated in 588 PD patients. A total of 588 valid questionnaires were retrieved, and the recovery rate was 100%. Among the 588 patients studied, there were 284 males (48.30%) and 304 females (51.70%), with an average age of 56.5 ± 14.73 years. There were 484 patients (82.31%) with primary and secondary education levels. The main reasons for not choosing APD were never using APD (78.23%), no knowledge of APD (69.39%), and family did not support using APD (77.55%) (Table 1).
Factors Influencing the Completion Rate of APD Treatment
In the univariate analysis, marital status, educational background, occupation, dialysis duration, peritonitis and catheter complications were not associated with acceptance of APD (P > 0.05). Patients with higher education levels did not have higher APD selection rates than did patients with lower education levels (P= 0.289), and patients with longer years on dialysis did not have higher APD selection rates than did patients with fewer years on dialysis. Knowledge of APD (P= 0.273). The occurrence of peritonitis did not affect the choice of APD (P=0.57), the occurrence of catheter complications did not affect the choice of APD (P=0.738), and the cooperative attitude toward treatment did not affect the choice of APD (P=0.795). User experience and family support were the factors that affected patients’ choice of APD (all P < 0.05) and were positively correlated with the treatment utilization rate. Patients’ experience with APD affected APD selection rate (P=0.023), knowledge of APD affected APD selection rate (P=0.000), and family members’ support affected APD selection rate (P=0.000). (Table 2).
 |
Table 2 Factors Related to the APD Selection Rate of Patients |
In the multivariate analysis, 3 variables (treatment with APD, knowledge of APD, and family support) remained significantly associated with the selection of APD. The selection rate for APD was 2.594 times (P=0.026) higher among patients who had received APD than those who had not received APD before. The selection rate for patients with “a lot of knowledge” about APD was 10.75 times (P=0.002) that of patients with “no knowledge” and 3.839 times (P=0.002) that of patients with “partial knowledge”. The APD selection rate with family support was 8.778 times (P < 0.001) higher than that without family support. Among the options for reasons for choosing APD, “a good knowledge of APD” had the highest selection rate (Table 3).
 |
Table 3 Factors Related to the APD Selection Rate of Patients by Logistic Regression Analysis |
Discussion and Conclusion
Discussion
As an alternative treatment for end-stage renal disease, APD is more convenient than CAPD for individuals with study and work needs. Because multiple manual operations are not required during the fluid exchange process, the rate of peritonitis and catheter-associated infection is reduced. The dialysis parameters can be adjusted quickly and accurately to obtain adequate toxin clearance for personalized dialysis.10,11 Studies have shown that APD is safe and easy, has little impact on life and social roles, and can significantly improve the quality of life of patients. APD has become the prevalent mode of peritoneal dialysis in most high-income countries.12,13 Previously studies showed that factors such as educational background, occupation, dialysis duration, knowledge of APD, and family support may affect that influence patients’ choosing APD.5 In this study, we performed a cross-sectional questionnaire-based study to investigate the factors that affect the patients’ choice for APD treatment.
The present study indicates that the main reasons for not choosing APD as a treatment mode are lack of previous APD use (78.23%), lack of APD understanding (69.39%), and lack of family support of ADP use (77.55%). Our results were consistent with the study by Domenici et al, which showed that the choice of treatment was based on patient preference.13 The perception of advantages and disadvantages of APD differed between patients undergoing APD and CAPD. Health care providers’ preference for dialysis mode may affect patients’ choice of APD as a treatment mode. With an insufficient introduction of APD-related dialysis knowledge by PD training, patients and their family members cannot obtain comprehensive dialysis knowledge about APD, which may affect their choice for the mode of PD. Studies have shown that important factors contributing to APD selection were better adjustment of APD to the patient’s lifestyle and the flexibility that APD offers.14 Patients did not voluntarily choose APD, resulting in a low APD selection rate. Peritoneal dialysis specialist nurses can provide APD information via leaflets, posters and video while performing PD training. The contents could include the indications for APD, and the advantages of ADP compared with CAPD.
Never having used APD before was the predominant (78.23%) reason for not choosing APD as the treatment mode. APD has not been widely used in China until recent years, lack of APD machines in the most PD centres, or lack of the experiences by health care providers could be the reasons for not enough APD treatment performed during post-surgical hospitalization. Moreover, remote monitoring of APD is increasingly used in peritoneal dialysis, but little is known about its acceptability by patients and caregivers.15 Remote monitoring of APD has become an emerging trend in the field of APD.14 Nephrologists and dialysis nurses should acquire more learning and training opportunities and update their knowledge about remote monitoring of APD to improve the effectiveness and efficiency of PD patients’ follow-up.
Patients often expect family support when making choices, and the attitudes of family support staff influence patients’ choices. The patient’s dialysis treatment will affect most of the life of family members, and family members hope to take part in the choice of dialysis mode. For major and long-term medical decisions, family discussions are generally needed to decide. For the elderly and patients with mobility difficulties, the attitude of family members towards APD dialysis treatment, the ability to assist in APD treatment and care affect the choice of APD. Strong family support helps to ensure that patients have the right to choose their own dialysis modalities. In this study, 77.55% of families did not support the choice of APD as a treatment mode. The high cost of APD treatment is one of the main reasons for the low family support rate. The cost of APD treatment is higher than that of CAPD. In China, the APD machine needs to be purchased or rented by patients without covering by medical insurance, and its price is around 30,000 ~ 80,000 RMB. Expensive APD machines and associated dialysis sets undoubtedly increase family expenses. Strong social support, including medical insurance policies and support from social charities, may help to ensure patients’ independent choice of dialysis mode.
Compared with CAPD, APD does not affect patient activities nor patients’ families during the day. Studies have shown that APD patients have a good quality of life and are less troubled by dialysis-related symptoms.14–16 APD is flexible and free, allowing individualized treatment for greater independence and safety at home. The remote monitoring of APD may enable residents in rural areas to receive specialist care, resolve problems fast, reduce rate hospitalization, and improve quality of life.6,17 In addition, remote therapy management of patients on APD may demonstrate cost savings.18 Recently, especially after the COVID-19 pandemic, more and more provinces in China, including Fujian Province, has begun to include the cost of APD treatment and machine in the local medical insurance, the rate of APD treatment will continue to increase in the near future.
Conclusion
Patients’ knowledge of APD, experience in application and family support were the most important factors affecting the choice of APD as a treatment mode and were positively correlated with the treatment utilization rate. Health care providers should raise awareness of APD among patients and their families, allowing patients to experience APD treatment if possible. When helping patients choose APD and CAPD, it is important to consider the medical, physiological, social, and economic aspects of each PD patient, as well as the patient’s preferences.
Limitations of the Study
This study has some limitations. As of 2019, the number of PD patients in China exceeded 103,000, and there were approximately 4000 PD patients in Fujian Province in southern China. The study only randomly included 588 patients in 6 regions. Therefore, the sample size was small, which may limit the results of this study being expanded to the other provinces in China. However, we minimized the occurrence of limiting events through patient inclusion criteria and sample size calculations.
Relevance to Clinical Practice
Understanding the influencing factors for the choice of APD by PD patients in Fujian Province, southern China, can help health care professionals to formulate more effective interventions. This study provides scientific evidence for improving APD treatment completion rates and improving patient quality of life.
Abbreviations
APD, automated peritoneal dialysis; PD, peritoneal dialysis; CAPD, continuous ambulatory peritoneal dialysis; ESRD, end stage renal disease.
Acknowledgment
Program of Fujian, a special grant for education and research from Fujian Department of Finance (2022)840, The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Cao F, Li L, Lin M, Lin Q, Ruan Y, Hong F. Application of instant messaging software in the follow-up of patients using peritoneal dialysis, a randomised controlled trial. J Clin Nurs. 2018;27(15–16):3001–3007. doi:10.1111/jocn.14487
2. Cao F, Hong F, Ruan Y, Lin M. Effect of patient-empowerment interaction model on self-management ability of peritoneal dialysis patients: a randomized controlled trial. Patient Prefer Adherence. 2023;17:873–881. doi:10.2147/PPA.S402698
3. Cuevas-Budhart MA, Celaya Pineda IX, Perez Moran D, et al. Patient experience in automated peritoneal dialysis with telemedicine monitoring during the COVID-19 pandemic in Mexico: qualitative study. Nurs Open. 2023;10(2):1092–1101. doi:10.1002/nop2.1377
4. Yeter HH, Manani SM, Ronco C. The utility of remote patient management in peritoneal dialysis. Clin Kidney J. 2021;14(12):2483–2489. doi:10.1093/ckj/sfab111
5. Walker RC, Morton RL, Palmer SC, Marshall MR, Tong A, Howard K. A discrete choice study of patient preferences for dialysis modalities. Clin J Am Soc Nephrol. 2018;13(1):100–108. doi:10.2215/CJN.06830617
6. Uchiyama K, Morimoto K, Washida N, et al. Effects of a remote patient monitoring system for patients on automated peritoneal dialysis: a randomized crossover controlled trial. Int Urol Nephrol. 2022;54(10):2673–2681. doi:10.1007/s11255-022-03178-5
7. Sanabria M, Vesga J, Lindholm B, Rivera A, Rutherford P, Uribarri J. Time on therapy of automated peritoneal dialysis with and without remote patient monitoring: a cohort study. Int J Nephrol. 2022;2022:8646775. doi:10.1155/2022/8646775
8. Cao XY, He YN, Zhou JH, et al. Safety, effectiveness, and manipulability of peritoneal dialysis machines made in china: a randomized, crossover, multicenter clinical study. Chin Med J. 2018;131(23):2785–2791. doi:10.4103/0366-6999.246079
9. Uzun Kenan B, Demircioglu Kilic B, Akbalik Kara M, et al. Evaluation of the Claria sharesource system from the perspectives of patient/caregiver, physician, and nurse in children undergoing automated peritoneal dialysis. Pediatr Nephrol. 2023;38(2):471–477. doi:10.1007/s00467-022-05563-9
10. Li X, Xu H, Chen N, et al. The effect of automated versus continuous ambulatory peritoneal dialysis on mortality risk in China. Perit Dial Int. 2018;38(Suppl 2):S25–S35. doi:10.3747/pdi.2017.00235
11. Ye H, Zhou Q, Fan L, et al. The impact of peritoneal dialysis-related peritonitis on mortality in peritoneal dialysis patients. BMC Nephrol. 2017;18(1):186. doi:10.1186/s12882-017-0588-4
12. Tong Y, Wang H, Cao X, Cai G, Chen X, Zhou J. Research hotspots and emerging trends of automated peritoneal dialysis: a bibliometric analysis from 2000 to 2020. Semin Dial. 2023;36(2):117–130. doi:10.1111/sdi.13078
13. Domenici A, Giuliani A. Automated peritoneal dialysis: patient perspectives and outcomes. Int J Nephrol Renovasc Dis. 2021;14:385–392. doi:10.2147/IJNRD.S236553
14. Nakamoto H. How automated peritoneal dialysis is applied and maintained in Japan. Contrib Nephrol. 2012;177:13–23.
15. Walker RC, Tong A, Howard K, Darby N, Palmer SC. Patients’ and caregivers’ expectations and experiences of remote monitoring for peritoneal dialysis: a qualitative interview study. Perit Dial Int. 2020;40(6):540–547. doi:10.1177/0896860820927528
16. Yang F, Luo N, Lau T, Yu ZL, Foo MWY, Griva K. Health-related quality of life in patients treated with continuous ambulatory peritoneal dialysis and automated peritoneal dialysis in Singapore. Pharmacoecon Open. 2018;2(2):203–208. doi:10.1007/s41669-017-0046-z
17. Amici G, Lo Cicero A, Presello F, et al. I vantaggi dell’applicazione del monitoraggio da remoto in dialisi peritoneale automatizzata domiciliare [The advantages of remote patient monitoring in automated peritoneal dialysis]. G Ital Nefrol. 2020;37(3):2020–vol3. Italian.
18. Borrelli S, Frattolillo V, Garofalo C, et al. Monitoraggio da remoto del paziente in dialisi: il cambio di passo per la dialisi domiciliare? [Remote patient monitoring in dialysis patients: the “change of pace” for home dialysis]. Recenti Prog Med. 2020;111(7):404–410. Italian. doi:10.1701/3407.33922
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
