Back to Journals » Research and Reports in Urology » Volume 12
Factors Impacting Stone-Free Rate After Retrograde Intrarenal Surgery for Calyceal Diverticular Calculi
Authors Boonyapalanant C, Saksirisampant P , Taweemonkongsap T, Leewansangtong S, Srinualnad S, Chotikawanich E
Received 12 June 2020
Accepted for publication 5 August 2020
Published 20 August 2020 Volume 2020:12 Pages 345—350
DOI https://doi.org/10.2147/RRU.S265959
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jan Colli
Chatporn Boonyapalanant, Pat Saksirisampant, Tawatchai Taweemonkongsap, Sunai Leewansangtong, Sittiporn Srinualnad, Ekkarin Chotikawanich
Division of Urology, Department of Surgery, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Ekkarin Chotikawanich
Division of Urology, Department of Surgery, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand
Tel +66-2-419-8010
Email [email protected]
Objective: To evaluate the outcomes of retrograde intrarenal surgery (RIRS) treatment of calyceal diverticular calculi and identify the associated factors affecting post-operative stone-free rate.
Materials and Methods: From August 2015 to May 2019, data of 32 patients with calyceal diverticular calculi who were treated by RIRS in a Siriraj Hospital were retrospectively studied. All operations were performed by the same surgeon using flexible ureterorenoscopy (f-URS) and holmium YAG laser lithotripsy. Calyceal diverticula were identified by our refluxing technique and from the collected demographic, diverticular and stone data. Operative outcomes were retrospectively evaluated. Data were analysed to identify the factors associated with stone-free outcomes. Stone-free was defined as no residual stones remaining after surgery.
Results: Mean age of the patients was 55.7 years. Stone locations were non-lower pole in 81.2% of cases and lower pole for the remaining 18.8% of cases. Median stone size was 1.2 cm with three as the median number of stones per patient. Calcium oxalate was the most common stone composition (56.3%). Positions of the diverticulum were anterior calyx (34.4%) and posterior calyx (50%), while the remainder were undetermined (incomplete data). Average length of the diverticular neck was 0.4 cm. Mean operative time was 46 minutes and mean hospital stay was 2.9 days. Complications included fever in three patients (9.3%) and sepsis in two patients (6.3%), with overall post-operative stone-free rate at 75%. Factors significantly affecting stone-free status were stone size (P=0.003) and length of diverticular neck (P=0.038). Multivariate analysis determined that only stone size had a statistically significant effect on post-operative stone-free status (P=0.015). Cut off point for stone size that increased the chances of a post-operative stone-free outcome was less than 1.5 cm, as determined by the ROC curve.
Conclusion: RIRS was found to be an effective and safe treatment option for the removal of calyceal diverticular calculi. Stone size of less than 1.5 cm offered a better chance of post-operative stone-free condition.
Keywords: calyceal diverticular calculi, retrograde intrarenal surgery, endoscopy
Introduction
A calyceal diverticulum is a urothelium-lined cystic dilatation of the renal collecting system. This presents as an uncommon anatomic abnormality of the kidney with incidence of about 4.5 per 1000 population.1 However, 9.5–50% of calyceal diverticula are associated with internal calculi formation that appear to be caused by anatomical obstruction and urine stasis.1–3 The disease occurs more commonly in women than in men.2,3 Nowadays, the treatment option with the optimal post-operative stone-free rate is percutaneous nephrolithotomy (PCNL),4,5 whereas retrograde intrarenal surgery (RIRS) is an optional treatment for small calculi located in the upper and middle calyces.5
Recently, stone management using the endourological technique has become more advanced, thus RIRS can now treat large calyceal diverticular calculi in the lower calyx with improved treatment outcomes. Previous studies determined that the stone-free rate of treating calyceal diverticular calculi by RIRS was 85%.6 However, to the best of our knowledge, there are no published reports concerning the factors that affect the post-operative stone-free rate for RIRS.
Therefore, this study was conducted to identify factors affecting treatment outcomes of calyceal diverticular calculi by RIRS.
Materials and Methods
This study was approved by the Ethics Committee of the Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand, protocol number 738/2560(EC3). In this IRB certificate of approval for the study, patient consent was waived for this retrospective study due to a retrospective study protocol in Siriraj Hospital. However, all patient data retained confidentiality and compliance with the Declaration of Helsinki. Charts of patients with renal diverticular calculi who underwent RIRS at Siriraj Hospital from August 2015 to May 2019 were retrospectively reviewed. All surgical procedures were performed by the same experienced urologist. Each patient was diagnosed before the operation by a computerized tomography (CT) scan or intravenous pyelography (IVP) to evaluate the calculi and calyceal diverticulum. RIRS was considered to be the first option for all cases. Under general anesthesia, all patients were treated using flexible ureterorenoscopy (f-URS) and holmium YAG laser lithotripsy. Enlarging the opening of the calyceal diverticulum was also performed by laser before lithotripsy was conducted to remove the stone fragments. The location of the diverticulum was confirmed before using a laser to widen its opening by the refluxing technique comprising the contrast medium methylene blue. The mixture was injected through the ureteroscope in front of the suspected diverticular opening, previously confirmed by fluoroscopy, until filling the entire collecting system. Endoscopy with normal saline was continued until the methyl blue was cleared and fluid irrigation was then discontinued. Refluxing of the methylene blue was revealed from the diverticular opening (Figure 1). This technique is useful to identify the opening before precise cutting using a laser. The opening and the neck were cut until the ureteroscope was able to enter into the diverticulum. Laser lithotripsy was performed following a similar technique for non-diverticular calculi depending on the size of the stone. At the end of the procedure, a contrast study was performed to evaluate the diameter of the diverticular neck and confirm that there was no leakage. A double-J stent was retained while the upper coil was inside the diverticulum (Figure 2). The stent was removed at the first follow-up, 2 weeks after the operation. Ultrasonography or KUB film was performed to determine the stone status by radiologists as a matter of routine. KUB film was used to evaluate opaque stones, while ultrasonography was used to evaluate non-opaque stones. Stone-free status described no post-operative residual stones.
 |
Figure 1 A refluxing technique with methylene blue was used to identify the diverticular opening. (A) Suspected opening. (B) Refluxing of methylene blue through the opening. |
Demographic, diverticular, and stone data were collected. All patients were categorized into two groups as stone-free and remaining with residual stones. Data from both groups were analyzed to identify factors associated with stone-free outcomes.
Statistical analysis was conducted using PASW (SPSS) Statistics version 18.0 software. Demographic data were presented as mean±SD. In the case of a normal distribution, independent sample t-test, Fisher’s exact test, and Pearson’s chi-square were used to compare the results between both groups using a P-value of less than 0.05 to determine statistical significance. An ROC curve was used to determine the cut-off point of stone size and length of diverticular neck on post-operative stone-free outcome. Logistic regression for multivariate analysis was used to identify the statistically significant factors that affected the stone-free rate.
Results
Thirty-two patients were enrolled in this study, with demographic data shown in Table 1. Ten patients (31.3%) were male and 22 (68.8%) were female. Mean age was 55.7 years old and the most common presenting symptom was pyuria.
 |
Table 1 Demographic Data |
Stone location was non-lower pole in 81.2% of cases and lower pole for the remaining 18.8% of cases. Overall median stone size was 1.2 cm, with the median number of stones per patient being three. The most common stone composition was calcium oxalate (56.3%), followed by calcium phosphate (25%). Positions of calyceal diverticulum were 34.4% anterior, 50.0% posterior, and 15.6% unknown (incomplete data). Stones located in the anterior and posterior diverticulum had median cumulative sizes of 1.21.6 cm respectively, while the average length of the diverticular neck was 0.4 cm.
Mean operative time was 46 minutes and mean hospital stay was 2.9 days, with an average follow-up time of 2.3 weeks. Incidence of complications after surgery was 15.6% (Table 2). Three patients (9.3%) had post-operative fever and two patients (6.3%) developed sepsis. All these patients were successfully treated with antibiotics. There was no major ureter injury related to f-URS, and the stone-free rate after the operation was 75%.
 |
Table 2 Complications |
Factors affecting stone-free status included stone size, stone position, position of diverticulum, and length of diverticular neck, measured from the opening to the diverticulum (Figure 3). Stone size and diverticular neck length were evaluated utilizing the ROC curve to determine the optimal cut-off point. For stone size, this was 1.5 cm with sensitivity of 75% and specificity of 87.5% (Figure 4), while the optimal length of the diverticular neck was 0.4 cm with sensitivity and specificity of 70.875% (Figure 5). These factors were compared between the stone-free group and the residual stone group, with results shown in Table 3. There were statistically significant differences for stone size (P-value=0.003) and length of diverticular neck (P-value=0.038), while no statistically significant differences were recorded for stone location (P-value=0.625) and position of diverticulum (P-value=1.000). However, multivariate analysis revealed that only stone size was statistically significant (P-value=0.015), as shown in Table 4.
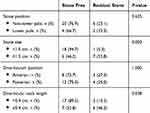 |
Table 3 Outcomes |
 |
Table 4 Multivariate Analysis of the Factors Affecting the Stone-Free Rate |
 |
Figure 3 The length of the diverticular neck was measured from the opening to the diverticulum. |
 |
Figure 4 ROC curve, optimal cut-off point of stone size. |
 |
Figure 5 ROC curve, optimal cut-off point of diverticulum neck length. |
Discussion
In recent years, PCNL has been accepted as the first-line treatment of calyceal diverticular calculi, while RIRS was an optional procedure for small stones located in the upper or middle calyx. Bas et al7 reported that the overall stone-free rate for PCNL was 82.8%, with 62% of stones in the lower calyx, while the overall stone-free rate for URS was 76%, with 80% of stones in the non-lower calyx. In our study, total stone-free rate was 75%, which included 18.8% of lower pole calculi. There was no patient selection and all of the diverticular calculi patients underwent RIRS as the first treatment, including both favorable and unfavorable outcomes. However, post-operative stone-free rates were 94.7% for stones with a diameter less than 1.5 cm and 89.5% for stones located in the diverticulum, with a diverticular neck length of less than 0.4 cm, regardless of the calyceal location. The diverticular neck length was considered to be a factor affecting stone-free status, as a longer neck length caused misdirection in laser cutting from the opening to the diverticulum. However, a stone diameter of less than 1.5 cm was the only significant factor affecting stone-free rates according to multivariate analysis.
Previous studies reported that an anteriorly located diverticulum is difficult to manage by PCNL due to the longer distance or inaccessible angle.1,8 Significant hemorrhage is one of the complications when the tract has to traverse through the renal parenchyma to access anterior lesions.8,9 Percutaneous access is commonly preferred for a posterior diverticulum as a direct puncture to reach the stone.7,10 In this study, 34.4% of cases had the diverticulum located in the anterior position, with stones at a median size of 1.2 cm. The success rate for anterior diverticula was 72.7% stone-free, although this was not statistically different from the posterior case. Thus, it was worthwhile to consider RIRS as a procedure for diverticular calculi located in the anterior calyx.
After stone removal, destroying the diverticular mucosa to prevent recurrent stasis of urine in the diverticulum was recommended, especially for percutaneous access. For retrograde access, after widening the diverticular neck, urine was able to pass into the calyx as an internal shunt; therefore, here, the mucosa of the diverticulum were not destroyed. A ureteral stent was retained in all cases. The upper coil of the stent was located in the diverticulum to drain the urine, while the stent passed through the diverticular neck to prevent stenosis. The mean follow-up period in this study was 2.3 weeks with no diverticulum recurrence. However, a longer follow-up is recommended to ensure no further diverticulum recurrence.
The occurrence of complications in this study was similar to levels reported in previous studies5,11-13 at 15.6%. The most common complication was fever (9.3%) followed by sepsis (6.3%). These were successfully treated by antibiotics without further intervention being required. The rate of infectious complications in this study was comparable to that of RIRS for kidney stones without diverticulum.14,15
Our results indicated that RIRS achieved a 94.7% post-operative stone-free result for stones less than 1.5 cm in diameter, regardless of diverticulum position.
There were some limitations in this study. These included bias, which is inevitable in a retrospective research study, incomplete data, and a small number of patients due to low incidence of the disease.
Conclusions
RIRS is a treatment option for treating calyceal diverticular calculi. Stone size less than 1.5 cm was a factor in achieving optimal post-operative stone-free rate. A diverticular neck length of less than 0.4 cm had a higher chance of attaining a stone-free result. Operative outcomes for the anterior and posterior calyceal diverticulum were similar.
Abbreviations
RIRS, retrograde intrarenal surgery; KUB, kidneys, ureters, and bladder; CT, computerized tomography; IVP, intravenous pyelogram; US, ultrasound; PCNL, percutaneous nephrolithotomy; URS, ureteroscopy; f-URS, flexible ureteroscopy; ROC, receiver operating characteristics; AUC, area under the curve.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gross AJ, Herrmann RW. Management of stones in calyceal diverticulum. Curr Opin Urol. 2007;17:136–140. doi:10.1097/MOU.0b013e328011bcd3
2. Timmons JW
3. Middleton AW
4. Auge BK, Munver R, Kourambas J, Newman GE, Preminger GM. Endoscopic management of symptomatic caliceal diverticula: a retrospective comparison of percutaneous nephrolithotripsy and ureteroscopy. J Endourol. 2002;16:557–563. doi:10.1089/089277902320913233
5. Waingankar N, Hayek S, Smith AD, Okeke Z. Calyceal diverticula: a comprehensive review. Rev Urol. 2014;16:29–43.
6. Erkurt B, Kiremit MC, Altay B, et al. Is retrograde flexible nephrolithotripsy feasible for calyceal diverticular stone? Urolithiasis. 2014;42:347–351. doi:10.1007/s00240-014-0672-1
7. Bas O, Ozyuvali E, Aydogmus Y, et al. Management of calyceal diverticular calculi: a comparison of percutaneous nephrolithotomy and flexible ureterorenoscope. Urolithiasis. 2015;43:155–161. doi:10.1007/s00240-014-0725-5
8. Matlaga BR, Jansen JP, Meckley LM, Byrne TW, Lingeman JE. Treatment of ureteral and renal stones: a systematic review and meta-analysis of randomized, controlled trials. J Urol. 2012;188:130–137. doi:10.1016/j.juro.2012.02.2569
9. Tepeler A, Bozkurt OF, Resorlu B, et al. Is the percutaneous nephrolithotomy procedure complicated in patients with anterior caliceal stones? Urol Int. 2013;90:389–393. doi:10.1159/000345711
10. Canales B, Monga M. Surgical management of the calyceal diverticulum. Curr Opin Urol. 2003;13:255–260. doi:10.1097/00042307-200305000-00015
11. Chong TW, Bui MH, Fuchs GJ. Calyceal diverticula. Ureteroscopic Management Urol Clin North Am. 2000;27:647–654. doi:10.1016/S0094-0143(05)70114-2
12. Zhang JQ, Wang Y, Zhang JH, Zhang XD, Xing NZ. Retrospective analysis of ultrasound-guided flexible ureteroscopy in the management of calyceal diverticular calculi. Chin Med J. 2016;129:2067–2073. doi:10.4103/0366-6999.189060
13. Grasso M, Lang G, Loisides P, Bagley D, Taylor F. Endoscopic management of the symptomatic caliceal diverticular calculus. J Urol. 1995;153:1878–1881. doi:10.1016/S0022-5347(01)67337-3
14. Li T, Sun XZ, Lai DH, Li X, He YZ. Fever and systemic inflammatory response syndrome after retrograde intrarenal surgery: risk factors and predictive model. Kaohsiung J Med Sci. 2018;34:400–408. doi:10.1016/j.kjms.2018.01.002
15. Baseskioglu B. The prevalence of urinary tract infection following flexible ureterenoscopy and the associated risk factors. Urol J. 2019;16:439–442. doi:10.22037/uj.v0i0.4340
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.