Back to Journals » Open Access Emergency Medicine » Volume 14
Factors Associated with Unscheduled Emergency Department Revisits in Children with Acute Lower Respiratory Tract Diseases
Authors Sakulchit T , Thepbamrung S
Received 22 January 2022
Accepted for publication 3 June 2022
Published 21 June 2022 Volume 2022:14 Pages 275—282
DOI https://doi.org/10.2147/OAEM.S359505
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Teeranai Sakulchit, Suphakorn Thepbamrung
Department of Emergency Medicine, Songklanagarind Hospital, Prince of Songkla University, Hatyai, Songkhla, Thailand
Correspondence: Teeranai Sakulchit, Department of Emergency Medicine, Faculty of Medicine, Prince of Songkla University, Karnjanavanich Road, Korhong, Hatyai, Songkhla, 90110, Thailand, Tel +66817379179, Fax +6674451704, Email [email protected]
Purpose: To identify factors associated with unscheduled emergency department (ED) revisits within 72 hours in children with acute dyspnea from lower respiratory tract diseases.
Patients and Methods: This retrospective cohort study included pediatric patients (age group: one month to 15 years old) who visited the ED with acute lower respiratory tract diseases between January 1st, 2017 and February 28th, 2019. The medical records were reviewed and discharged patients were dichotomized into revisit and non-revisit groups, based on whether the patients needed a revisit or not. Baseline characteristics, vital signs, diagnosis, treatment, pediatrician consultation, ED length of stay, and primary doctor of both groups were compared. Univariate and multivariate analyses by logistic regression were used to determine the significant factors associated with the revisits.
Results: Medical records of 918 eligible pediatric patients (1417 visits) were reviewed. Factors significantly associated with the revisits were history of asthma or current controller use (odds ratio [OR]: 3.08: 95% confidence interval [CI]: 1.86– 5.1). Not prescribing systemic corticosteroids (P < 0.001), or prescribing them upon discharge without first dose in the ED (P = 0.022) were significantly associated with revisits.
Conclusion: No prescription of systemic corticosteroids or prescription upon discharge, without an immediate dose at the ED, in children with history of asthma or current controller use were associated with revisits.
Keywords: child, dyspnea, emergency department, respiratory system abnormalities, revisit
Introduction
Unscheduled revisits to the emergency department (ED) within 72 hours after initial presentation is a major problem of many EDs. These unscheduled revisits indicate failure to provide proper assessment, diagnosis, treatment, and patient or parental instructions.1–5 Revisits contribute to ED overcrowding, and thus lead to a delay in treatment, patient dissatisfaction, increased utilization of ED resources, and increased healthcare expenses.3
Factors such as young age, race, specific triage level, chronic medical conditions, tachycardia, diagnosis related to respiratory or gastrointestinal conditions, intravenous fluid administered in the ED, and parental concern have been reported to be associated with unscheduled revisits in children.1,3,6–8 Revisits result in additional interventions such as, supplemental oxygen, respiratory medications, antibiotics, peripheral intravenous line placement, and hospitalization.7–9 However, most studies evaluated revisits in general, with only few reports focusing on specific complaints or conditions such as fever, dyspnea, vomiting or diarrhea.1,6
The concept of safety netting10,11 has been proposed to reduce unscheduled revisits. It involves clinicians providing parents and guardians instructions to identify alarming signs and symptoms, and for follow-up. Moreover, scheduled appointment with the pediatric outpatient clinic for children discharged from the ED can reduce these visits; however, they can still occur. From our ED’s revisit reviews, acute dyspnea caused by lower respiratory pathology is one of the most common causes of revisits for pediatric patients.
Therefore, the primary objective of this study was to identify factors associated with unscheduled revisits in children with acute dyspnea caused by lower respiratory disorders, after being discharged from the ED of our tertiary care hospital. The secondary objective involved investigation of the prevalence and timing of the revisit, the disposition, and the adverse events following the revisits. This information will be useful to improve the process of safety netting in the future.
Materials and Methods
Study Design
This was a retrospective cohort study of pediatric patients who had dyspnea caused by acute lower respiratory tract disorders, visiting the ED of Songklanagarind Hospital, Thailand between January 1st, 2017 and February 28th, 2019. The study was approved by the Ethics Committee of the Faculty of Medicine, Prince of Songkla University (Approval number REC. 63-107-20-4). Informed consent was waived due to the retrospective nature of the study. Medical records of the participants were reviewed and no intervention was involved. The study was conducted according to the guidelines of the Declaration of Helsinki and hence the participants were deidentified.
Patients
The inclusion criteria for the study were 1) pediatric patients from 1 month to 15 years of age; and 2) patients who had dyspnea caused by acute lower respiratory tract disorders; including, bronchitis, bronchiolitis, viral induced wheezing, asthma, and pneumonia. The exclusion criteria were 1) pediatric patients who had dyspnea from upper airway or lung parenchymal diseases; including, tracheitis, laryngitis, viral croup, pulmonary edema, interstitial lung disease, pneumothorax, and pneumonitis due to chemical agents; 2) patients who had chronic lung diseases (eg, bronchopulmonary dysplasia); 3) patients who had chronic aspiration syndromes (eg, cerebral palsy, tracheostomy status or tracheoesophageal fistula); 4) patients who had dyspnea from other organ systems (eg, cardiovascular diseases or metabolic disorders); 5) parents or guardians refusing further treatment or investigation in the ED; 6) patients who were not evaluated by the emergency physician; and 7) patients with irrelevant causes of revisit after the first visit.
Study Protocol
The electronic medical records of the eligible participants were retrospectively reviewed. Age groups, gender, history of preterm birth, previous history of endotracheal intubation, history of asthma, history of current controller use (inhaled corticosteroids with or without long acting beta-2 agonist or leukotriene receptor antagonist), Emergency Severity Index (ESI) level, vital signs, test results of influenza or RSV infection, diagnosis, treatment (numbers of inhaled bronchodilator received in the ED, oxygen supplementation, antibiotics, and systemic corticosteroids used), pediatrician consultation, disposition (admit, refer, or discharge), emergency department length of stay (EDLOS), level of experience of the primary doctor, and revisit status were recorded.
All patients were classified based on disposition into those who were hospitalized, referred, and discharged. Patients discharged from the ED were further classified into two groups, according to the revisit status (revisit and non-revisit). In cases of revisit, the clinical information as well as time to revisit, change of diagnosis, change of treatment, adverse events (fluid resuscitation, endotracheal intubation, cardiac arrest, and death), and disposition (with intervention, hospitalization, or ICU admission) of the second visit were reviewed and recorded. Factors between revisit and non-revisit groups were analyzed and compared.
Statistical Analysis
Data were recorded in Microsoft Excel 2016, and the statistical analysis was conducted using R software (version 3.6.3). Continuous variables with skewed distribution were reported as median; whereas, discrete variables were reported as frequencies and percentage. Comparison of the continuous variables between two independent groups was performed by Wilcoxon rank-sum test. Pearson’s Chi-squared test or Fisher’s exact test was used to compare discrete variables between two independent groups. Comparisons of the continuous and discrete variables between two dependent groups were conducted using Wilcoxon signed rank and McNemar tests, respectively. Univariate logistic regression analysis and subsequent multivariate logistic regression analysis were used to determine significant factors associated with unscheduled ED revisits in children with acute lower respiratory tract disorders. Analytical results were described as odds ratio (OR), with 95% confidence interval (CI). A P-value of less than 0.05 was considered statistically significant.
Results
Demographic Data
A total of 1417 visits by 918 pediatric patients who visited the ED for acute lower respiratory disorders within the study period were analyzed in this study. Of the 1417 visits, 407 visits resulted in admission or referral of the patients to other hospitals and 1010 visits resulted in discharge of the patients. Among those discharged, 870 visits did not result in revisit; whereas 70 visits resulted in a revisit (total 140 visits by 70 patients).
The demographic data of the study participants are presented in Table 1. Of the 1417 visits 896 (63.2%) visits were by male patients. The median age of the participants was 3.04 years (IQR: 1.52, 5.24). Preschool children (3–5 years of age) were the most common group to visit the ED due to complications caused by acute lower respiratory tract diseases (N=508 visits, 35.9%). Children with a history of asthma or current controller accounted for 497 (35.1%) visits.
 |
Table 1 Baseline Characteristics of the Children |
Primary Outcome
Among discharged patients, a higher proportion of children with a history of asthma or current controller use were in the revisit group compared to the non-revisit group; by both univariate (OR 2.95, 95% CI 1.79–4.87) and multivariate analyses (OR 3.08, 95% CI 1.86–5.1, P < 0.001). Whereas, a higher proportion of children with a history of preterm birth were present in the revisit group as compared to the non-revisit group. However, a significant difference was observed when the data were analyzed by univariate analysis (P = 0.047), but not when analyzed by multivariate analysis.
Vital signs at admission and prior to discharge, investigations, and treatment of both revisit and non-revisit groups are presented in Table 2. Both revisit and non-revisit groups showed no significant difference with respect to these parameters.
 |
Table 2 Comparison of Children’s Vital Signs, Investigations, and Treatment |
A higher proportion of patients with history of asthma or current controller use, that were not administered systemic corticosteroids throughout the course of treatment were in the revisit group compared to the non-revisit group (P< 0.001). Moreover, the proportion of children who did not receive systemic corticosteroids in the ED, but were prescribed systemic corticosteroids upon discharge were significantly higher in the revisit group compared with the non-revisit group (P = 0.022) (Table 3).
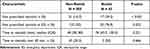 |
Table 3 Corticosteroids Use in Children with History of Asthma or Current Controller Use |
Secondary Outcomes
A majority of patients in the revisit group were back in the ED within 24 hours (N = 50, 71.4%). While 16 patients (22.9%) revisited between 24 to 48 hours, and 4 patients (5.7%) revisited between 48 to 72 hours. The patients received new diagnosis in eight of the visits. Some interventions such as supplemental oxygen (P < 0.001), intravenous fluid hydration (P = 0.022), and pediatrician consultation (P < 0.001) were more frequent at the second visit as compared to that in the first visit (Table 4). Hospital admissions or referrals were more common during the second visit (N = 36, 51.4%) as compared to that during the first visit (N = 407, 31.9%) (P < 0.001). No serious adverse events (fluid resuscitation, endotracheal intubation, cardiac arrest, and death) were observed during the second visit. Only one case from the revisited group was admitted to the ICU, for high flow oxygen therapy, and the patient was discharged after three days of admission without complications.
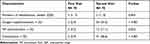 |
Table 4 Comparison of Children’s Intervention Following Revisit |
Discussion
In this study, overall revisit rate of children visiting the ED of Songklanagarind Hospital due to acute lower respiratory problems was estimated to be 4.9% (70 revisits from 1417 visits within the study period). This number was lower than the revisit rate of other complaints in most previous studies (3.3% to 21.4%).1,6–9 However, this study found that the rate of interventions (supplemental oxygen, intravenous fluid hydration, and pediatrician consultation) was significantly increased in the second visit, which was similar to previous studies.7–9 Fortunately, no serious adverse events occurred in the second visits. Moreover, we analyzed the factors associated with unscheduled ED revisits in children with acute lower respiratory tract disorders using univariate and multivariate logistic regression analysis. A history of asthma, current controller use, no administration of systemic corticosteroids throughout the course of the ED stay, and administration of systemic corticosteroids only after discharge were associated with ED revisits.
Previous studies reported that patients with acute asthma exacerbations treated with systemic corticosteroids had better outcome than those treated with placebo. Preschoolers with asthma or recurrent wheezing receiving oral corticosteroids in the ED had lower risk of hospital admissions (Relative Risk [RR] 0.58; 95% CI: 0.37 to 0.92, I2 = 0%), and those receiving oral corticosteroids as inpatients needed less additional corticosteroids (RR 0.57; 95% CI: 0.40 to 0.81, I2 = 0%).12 A study in both children and adults with asthma exacerbation revealed that those treated with systemic corticosteroids had fewer hospital revisits in the first week (RR 0.38; 95% CI 0.2–0.74). Those in the corticosteroids group also had fewer hospitalizations (RR 0.35, 95% CI: 0.13–0.95) and reduced need for beta-2 agonists (mean difference [MD] −3.3 activations/day; 95% CI −5.6 to −1.0). Moreover, the side effects of corticosteroids use (SMD 0.03; 95% CI: −0.38 to 0.44) were not significantly different relative to those of placebo.13 In children hospitalized due to severe acute asthma, those treated with systemic corticosteroids were discharged early at the first re-examination after admission (>4 hours) (OR 7.0; 95% CI: 2.98 to 16.45) with Number Needed to Treat (NNT) of 3 (95% CI: 2 to 8). Children in the treatment group also had short length of stay (WMD −8.75; 95% CI −19.23 to 1.74) and were less likely to relapse within three months of hospitalization (OR 0.19; 95% CI: 0.07 to 0.55) with NNT of 3 (95% CI: 2 to 7).14
Early administration of systemic corticosteroids also leads to better outcome compared to delayed administration. Reduction of admission (OR 0.4; 95% CI: 0.2 to 0.7) and length of active treatment by 0.7 hours (95% CI: −1.3 to −0.8) were reported in children with moderate to severe asthma exacerbation who received corticosteroids in the ED within 75 minutes after triage compared with those with delayed administration.15 Similarly, children with asthma exacerbation receiving systemic corticosteroids in the ED within 60 minutes from triage had decreased length of stay by 25 minutes when compared with those receiving corticosteroids after 60 minutes (95% CI: 15 to 35, P < 0.0001).16 Systemic corticosteroids can be administered as early as the time of triage by triage nurses. This resulted in reduction of time for clinical improvement by 24 minutes (95% CI: 1 to 50, P = 0.04) and admission rate (OR 0.56; 95% CI: 0.36 to 0.87) when compared to those waiting to be treated by the ED physicians.17
Not receiving systemic corticosteroids was correlated with higher rate of repeat visits (P = 0.020) within a year from the first visit, in a study involving adult participants with diagnosis of asthma.18 Similar to this study, delayed or no prescription of systemic corticosteroids to children with asthma exacerbation were associated with revisits within 72 hours. However, we did not explore more factors associated with delayed or no prescription of corticosteroids, whereas another study found that factors associated with delayed corticosteroids administration in children with moderate to severe exacerbation were age younger than 2 years old (OR 0.16; 95% CI: 0.07 to 0.35), and children arriving during ED crowding (OR 0.79; 95% CI: 0.67 to 0.94).19
Limitations
This study has some limitations. Firstly, although factors associated with revisits in our study were related to children with asthma, the study was initially designed to collect data from children with dyspnea from lower respiratory tract diseases in general. More details related to asthma such as history of controller adherence, technique, and medical prescription other than systemic corticosteroids upon discharge from the ED were not completely collected and these factors could be associated with revisits in this group of patients.
Secondly, we evaluated the prescription of systemic corticosteroids in patients with known history of asthma or current controller use. However, we did not include children who were at risk for asthma, or those that had never been officially diagnosed, or prescribed a controller before visiting the ED into this group; even though administration or no administration of systemic corticosteroids to these children might also affect their revisit status.
Thirdly, we did not formally classify patients with history of asthma or current controller use into mild, moderate, or severe attack in the record forms. According to GINA guidelines, those with moderate to severe attacks should receive systemic corticosteroids within one hour.20 Without severity classification, this might affect the results of “time for steroids administration”, and might also affect the revisits.
Lastly, the study was retrospective in nature; therefore, some data in the medical records might be missing and incomplete. In addition, the study was conducted in a single ED; hence, information of patients’ revisits at other hospitals could not be retrieved. These missing data might also affect the data on number of revisits.
Thus, further study is required to specifically evaluate factors associated with revisits in children with the diagnosis of acute asthma exacerbation, as well as factors related to delayed or no prescription of systemic corticosteroids to improve quality of care and process of safety netting in the ED.
Conclusion
History of asthma or current controller use was associated with unscheduled ED revisits in children with acute dyspnea from lower respiratory tract disorders. Among this group of children, no administration of systemic corticosteroids, or administration only after discharge from the ED was significantly associated with revisits. Therefore, systemic corticosteroids should be prescribed for children with history of asthma or controller use (especially within one hour for those with moderate to severe attack according to the GINA guidelines) to avoid future revisits.
Acknowledgments
The authors thank Ms. Kingkarn Waiyanak, for searching and retrieving articles, Ms. Jirawan Jayuphan for data analysis, Ms. Karakkada Arayapithak for her help with editing the manuscript, the Epidemiology Unit for help with statistical analysis, and the Faculty of Medicine for general support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. de Vos-Kerkhof E, Geurts DHF, Steyerberg EW, Lakhanpaul M, Moll HA, Oostenbrink R. Characteristics of revisits of children at risk for serious infections in pediatric emergency care. Eur J Pediatr. 2018;177:617–624. doi:10.1007/s00431-018-3095-0
2. Kilicaslan O, Sönmez FT, Gunes H, Temizkan RC, Kocabay K, Saritas A. Short term unscheduled revisits to paediatric emergency department - a six year data. J Clin Diagn Res. 2017;11:SC12–SC15. doi:10.7860/JCDR/2017/25098.9484
3. Goh GL, Huang P, Kong MC, Chew SP, Ganapathy S. Unplanned reattendances at the paediatric emergency department within 72 hours: a one-year experience in KKH. Singapore Med J. 2016;57:307–313. doi:10.11622/smedj.2016105
4. Van den Bruel A, Haj-Hassan T, Thompson M, Buntinx F, Mant D. Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review. Lancet. 2010;375:834–845. doi:10.1016/S0140-6736(09)62000-6
5. Hutchinson CL, Mccloughen A, Curtis K. Incidence, characteristics and outcomes of patients that return to emergency departments. An integrative review. Australas Emerg Care. 2019;22:47–68. doi:10.1016/j.auec.2018.12.003
6. Freedman SB, Thull-freedman JD, Rumantir M, Atenafu EG, Stephens D. Emergency department revisits in children with gastroenteritis. J Pediatr Gastroenterol Nutr. 2013;57:612–618. doi:10.1097/MPG.0b013e3182a1dd93
7. Akenroye AT, Thurm CW, Neuman MI, et al. Prevalence and predictors of return visits to pediatric emergency departments. J Hosp Med. 2014;9:779–787. doi:10.1002/jhm.2273
8. Wilson PM, Florin TA, Huang G, Fenchel M, Mittiga MR. Is tachycardia at discharge from the pediatric emergency department a cause for concern? A nonconcurrent cohort study. Ann Emerg Med. 2017;70:268–76.e2. doi:10.1016/j.annemergmed.2016.12.010
9. Cozzi G, Ghirardo S, Fiorese I, et al. Risk of hospitalisation after early-revisit in the emergency department. J Paediatr Child Health. 2017;53:850–854. doi:10.1111/jpc.13561
10. Almond S, Mant D, Thompson M. Diagnostic safety-netting. Br J Gen Pract. 2009;59:872–874. doi:10.3399/bjgp09X472971
11. Jones CH, Neill S, Lakhanpaul M, Roland D, Singlehurst-Mooney H, Thompson M. Information needs of parents for acute childhood illness: determining “what, how, where and when” of safety netting using a qualitative exploration with parents and clinicians. BMJ Open. 2014;4:e003874. doi:10.1136/bmjopen-2013-003874
12. Castro-Rodriguez JA, Beckhaus AA, Forno E. Efficacy of oral corticosteroids in the treatment of acute wheezing episodes in asthmatic preschoolers: systematic review with meta-analysis. Pediatr Pulmonol. 2016;51(8):868–876. doi:10.1002/ppul.23429
13. Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. 2007;CD000195. doi:10.1002/14651858.CD000195.pub2
14. Smith M, Iqbal S, Elliott TM, Everard M, Rowe BH. Corticosteroids for hospitalised children with acute asthma. Cochrane Database Syst Rev. 2003;2003(2):CD002886.
15. Bhogal SK, McGillivray D, Bourbeau J, Benedetti A, Bartlett S, Ducharme FM. Early administration of systemic corticosteroids reduces hospital admission rates for children with moderate and severe asthma exacerbation. Ann Emerg Med. 2012;60(1):84–91.e3. doi:10.1016/j.annemergmed.2011.12.027
16. Davis SR, Burke G, Hogan E, Smith SR. Corticosteroid timing and length of stay for children with asthma in the Emergency Department. J Asthma. 2012;49(8):862–867. doi:10.3109/02770903.2012.717656
17. Zemek R, Plint A, Osmond MH, et al. Triage nurse initiation of corticosteroids in pediatric asthma is associated with improved emergency department efficiency. Pediatrics. 2012;129(4):671–680. doi:10.1542/peds.2011-2347
18. Wong AJW, Chan JJ, Koh MS, Lian SWQ, Fook SMC, Ong MEH. Compliance with asthma guidelines and association with outcomes in the emergency department of a tertiary care teaching hospital. J Acute Med. 2018;8(3):119–126. doi:10.6705/j.jacme.201809_8(3).0005
19. Bekmezian A, Fee C, Bekmezian S, Maselli JH, Weber E. Emergency department crowding and younger age are associated with delayed corticosteroid administration to children with acute asthma. Pediatr Emerg Care. 2013;29(10):1075–1081. doi:10.1097/PEC.0b013e3182a5cbde
20. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2021. Available from: https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
