Back to Journals » Patient Preference and Adherence » Volume 17
Factors Associated with Therapeutic Adherence in Multiple Sclerosis in Spain
Authors Soria C , Prieto L, Lázaro E, Ubeda A
Received 19 December 2022
Accepted for publication 18 February 2023
Published 14 March 2023 Volume 2023:17 Pages 679—688
DOI https://doi.org/10.2147/PPA.S401962
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Cristina Soria,1– 3 Lola Prieto,2 Esther Lázaro,3 Amalia Ubeda2
1Psicología de la Salud, Suportias, Madrid, Spain; 2Facultad de Medicina, Universidad Francisco de Vitoria, Madrid, Spain; 3Facultad de Ciencias de la Salud, Universidad Internacional de Valencia, Valencia, Spain
Correspondence: Cristina Soria, Suportias. Av. Juan Carlos I, 13. Torre Garena, Madrid, 28806, Spain, Tel +34 910 511 662, Email [email protected]
Purpose: Adherence to disease-modifying therapies (DMTs) in multiple sclerosis (MS) is a complex and multidimensional phenomenon. Identifying the predictors of therapeutic adherence in MS will guide the design of interventions to improve health outcomes. Our aim was to assess the degree of adherence to pharmacological treatments, assess the relationship between patient-related factors and pharmacological adherence and to identify predictors of adherence to pharmacological treatments in patients with MS in Spain.
Patients and Methods: A cross-sectional nationwide study was carried out in Spain between December 2020 and September 2021. The web-based evaluation protocol consisted of a self-questionnaire survey designed ad hoc and the application of validated questionnaires to assess adherence, as well as beliefs about medication and quality of life. Predictor variables of adherence to MS treatment were assessed using multivariate analysis.
Results: A total of 152 patients with MS participated (mean age: 44 years; 64% were female; and 78% had relapsing-remitting MS). Seventy-three percent of the patients reported being adherent to their pharmacological treatment for MS. Forgetfulness was the most common cause of non-adherence. Necessity beliefs and concerns beliefs were not statistically associated with adherence. The adherent group shows statistically significant better levels of quality of life in the cognitive function subscale than the non-adherent participants (p=0.040). Role limitations-emotional, emotional well-being and overall quality of life were not significantly associated with adherence. Predictors with a statistical association with adherence to treatment were years of education (OR=0.79; 95% CI: 0.65– 0.96; p=0.020) and intravenous treatment (OR=3.17; 95% CI: 1.07– 9.45; p=0.038).
Conclusion: We found an adequate adherence to pharmacological treatment. Low education and intravenous treatment were significant predictors of adherence to DMTs.
Keywords: adherence, disease-modifying therapy, medication belief, quality of life
Introduction
Multiple sclerosis (MS) is a chronic disease of the central nervous system that affects 2.8 million people in the world.1 However, despite the fact that the health condition of people with MS seems to have improved over the last decade,2 the disease has a great impact on personal, social and healthcare factors due to its tendency to produce disability in young adults, its negative impact on work, care needs and treatment costs.3
Although there is no cure at the moment, the availability of disease-modifying therapies (DMTs) has increased in recent years. However, to achieve the full therapeutic value of these treatments in MS patients, adherence is essential.4
A systematic review in MS indicates that rates of adherence to pharmacological treatments range between 52% and 93%, depending on the measurement methods used in the studies, which are very heterogeneous (self-report, electronic monitoring or pharmacy-based claims).5
Specifically, a study carried out in Spain reports figures of 71% for adherence to DMTs in patients with MS.6 In MS, a lack of therapeutic adherence can influence the evolution of the disease (greater risk of relapse and higher level of disability), the quality of life of patients and their emotional well-being, as well as the associated healthcare cost (greater number of hospitalizations and emergency hospital visits).7,8
Together with the pharmacological treatments for MS, rehabilitation treatments and healthy habits play a fundamental role in the control of this pathology. Not smoking, engaging in moderate physical activity, eating a balanced diet, maintaining optimal levels of vitamin D, avoiding stress, not consuming toxic substances and following rehabilitation treatments are some of the general recommendations for people with MS.9,10 The definition of adherence therefore includes pharmacological treatments but also lifestyle changes.11
Adherence is a complex and multidimensional phenomenon. The World Health Organization (WHO) categorizes the predictors that influence therapeutic adherence into five dimensions: social and economic factors (eg, age or education) health care team and system-related factors (eg, patient–doctor relationship), condition-related factors (eg, level of disability), therapy-related factors (eg, duration of treatment) and patient-related factors (eg, beliefs about medication or psychological aspects).12 In MS, a variety of factors were associated with adherent patients, including age, cognition, depression, treatment satisfaction, duration of the disease, severity of disease, comorbidities, route of administration, perceived lack of efficacy and adverse effects of the drugs.5,13
The reasons for non-adherence in MS are complex but can be addressed through appropriate interventions by health professionals,14 especially those factors that can be modified, such as beliefs about medication. Only a few studies have jointly assessed these psychological predictors of non-adherence in the MS population. Therefore, identifying the predictors of therapeutic adherence in MS will act as guidance for the design of interventions in order to improve health outcomes and promote self-management of treatment and disease in patients with MS.
This study aims to 1) assess the degree of adherence to pharmacological treatments in MS patients; 2) assess the relationship between patient-related factors (patients’ beliefs and quality of life) and pharmacological adherence; and 3) identify predictors of adherence to pharmacological treatments in patients with MS in Spain.
Materials and Methods
Design
This is a cross-sectional and nationwide study to assess predictors of therapeutic adherence in MS in Spain. Data were collected using a self-questionnaire online. This study is reported following the STROBE guidelines15 and approved by the Francisco de Vitoria University Research Ethics Committee (31/2020). The research was conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained from all participants, and the data were collected anonymously.
Setting
The study was carried out in Spain between December 2020 and September 2021. The questionnaire underwent pilot testing previously to ensure that patients understood all questions and the usability of the online tool. The pilot survey was completed by 10 participants with MS from a patient association (AEFEM Henares) who met all the inclusion criteria. No modifications had to be made to the questionnaire after the pilot test.
This study included people with MS from 13 autonomous regions. Patients were included from patient associations which are members of the AEDEM-COCEMFE federation (Asociación Española de Esclerosis Múltiple, an entity that is made up of 47 MS patient associations nationwide) and from hospitals by healthcare professionals (neurologists, nurses, psychologists and general practitioners).
Participants
A total of 152 patients with MS met all the inclusion criteria, which comprised patients 18 years or older, diagnosed with MS and receiving DMT for at least 6 months before enrollment. Patients unable to complete the self-administered questionnaire online on their own or with help from a caregiver (severe cognitive impairment, major psychiatric disorders or functional reasons) were excluded.
To determine the sample size, we considered 55,000 MS patients in Spain (data from the Spanish Society of Neurology), and with a 95% confidence level, a sampling error of 8% and a generic proportion of 0.5, we calculated a sample size of 150 participants. A consecutive non-probabilistic sampling method was used. Patients were identified by healthcare professional collaborators consecutively by order of attendance to their habitual follow-up consultations in hospitals or associations.
Variables and Measurements
The study variables are depicted in Figure 1, which groups the predictors into the WHO dimensions.12 Self-reported adherence to DMT 6 months prior to the study was assessed using the standardized Morisky-Green test.16
 |
Figure 1 Study model. |
The web-based evaluation protocol consisted of a self-questionnaire survey designed ad hoc and the application of validated questionnaires.
The validated scales included the Morisky-Green questionnaire,16 the Beliefs about Medicines Questionnaire (BMQ)17 and four subscales (role limitations-emotional, emotional well-being, cognitive function and overall quality of life) from the Multiple Sclerosis Quality of Life-54 (MSQOL-54).18
Self-Questionnaire
A self-questionnaire web-based survey with 143 items was developed for this study arranged into seven areas: 1) Socio-demographic factors (13 items); 2) Condition-related factors and therapy-related factors (11 items); 3) Adherence to DMT (21 items); 4) Adherence to rehabilitation treatments (22 items); 5) Adherence to healthy habits (26 items), 6) Information access (12 items); and 7) Psychological and cognitive factors (38 items). Questionnaire items were completed through dichotomous closed questions, Likert-type scales or multiple responses.
Ad hoc items were developed by trained researchers based on the results obtained in two focus groups with patients and were reviewed by a multidisciplinary team which included a neurologist, a nurse, a neuropsychologist, a pharmacist and a patient association representative.
Morisky-Green Questionnaire
Adherence to DMTs was measured using the Morisky–Green questionnaire,16 validated in the Spanish population.19 The scale has been widely used in numerous studies and several chronic diseases and has adequate reliability and internal consistency (Cronbach's alpha = 0.61).16 The Morisky-Green questionnaire scale includes four items with yes/no answers. Patients were considered non-adherent to treatment if they answered “yes” to any of the questions.
Beliefs About Medicines Questionnaire (BMQ)
The Beliefs about Medicines Questionnaire was used to assess beliefs about DMTs.17 The validated version in Spanish was used.20 The 10-item questionnaire contains two subscales: Specific-Necessity Beliefs and Specific-Concerns Beliefs. Horne et al were the first to present data supporting the reliability and the criterion-related and discriminant validity in different chronic medical conditions.17 In the MS population, Cronbach’s Alpha was α = 0.84 for the BMQ Specific-Necessity Beliefs scale and α = 0.69 for the BMQ Specific-Concern Beliefs scale.21 Each subscale includes 5 items, scored on a 5-point Likert-scale from “1” (strongly disagree) to “5” (strongly agree). Item-scores were summed for both subscales and higher scores indicate greater beliefs.
Multiple Sclerosis Quality of Life-54 (MSQOL-54)
Four subscales from the Multiple Sclerosis Quality of Life-54 (MSQOL-54)18 were selected: role limitations-emotional, emotional well-being, cognitive function and overall quality of life. The MSQOL-54 is an MS-specific instrument to measure quality of life, adapted to the Spanish population.22 The 4 subscales selected from the MSQOL-54 show good internal consistency with Cronbach’s alphas ranging from 0.84 to 0.90.18 The total score for each dimension ranged from 0 to 100, where a higher value indicates better health-related quality of life.
Bias
To avoid selection bias, healthcare professionals from patient associations and hospitals were instructed to consecutively recruit the first eligible patient by order of attendance to their habitual follow-up consultations, from the start date of the study.
A password-protected website was developed for this study and a unique code was assigned to each healthcare professional collaborator, ensuring that participants met all inclusion criteria.
Statistical Methods
Information was collected via an online database, exported to Microsoft Excel (Microsoft Corporation, Redmond US) and analyzed using R 3.6 (R Foundation for Statistical Computing). First, we presented descriptive statistics (eg, means or frequencies) for socio-demographic and health information. Second, we carried out univariate logistic regressions between the adherence to MS treatment and the rest of variables. Any variables with p-values <0.20 were considered potential variables to be included in the multivariate model. Variables with variance <5% were excluded from the analysis. Additionally, the variables “satisfaction with the neurologist”, “presence of comorbidities” and “time since MS diagnosis (chronicity)” were initially considered for the multivariate analysis based on previous evidence.8,13,23
Third, we applied the best subsets regression method with the goodness of fit (R2) metric to identify the variables that best predict the adherence to MS treatment. One of the advantages of this method, compared to other common strategies such as stepwise regression, is the capacity to identify combinations of variables without eliminating any of them in the process.24 The homoscedasticity of the resulting multivariate model was assessed and we considered multicollinearity variance inflation factor values >5.
Results
Patient Characteristics
A total of 215 patients with MS completed the survey. Of these individuals, 152 had been treated with a DMT for at least 6 months and were included in the final analysis. Their demographic and clinical characteristics are depicted in Table 1.
 |
Table 1 Demographic and Clinical Characteristics (n=152) |
Overall, the mean age of participants was 44 years (SD± 9.6) and 64% were female. Most patients were married or had a partner (67%), did not live alone (90%) and had higher education (86%).
Participants included in the study had been diagnosed for a mean duration of 13.03 years and predominantly had relapsing-remitting MS (78%). The mean time on their current DMT was 5.9 years and approximately 80% of the patients had previously received another DMT.
Regarding rehabilitation treatments and healthy habits, 38.2% received physiotherapy treatment for MS, 17.8% psychological therapy and only 6.6% neuropsychological treatment. 81% of the patients included in the study do not smoke, more than 45% of the patients do physical activity between 3 and 7 days a week, 75% eat a balanced diet and 62.5% take vitamin D.
Adherence
According to the Morisky-Green questionnaire, 73% of the patients reported being adherent to their pharmacological treatment for MS. Forgetfulness (80.5%) was the most common cause of non-adherence in our study. Regarding the type of DMT: 88.4% patients receiving intravenous treatment were adherent (p=0.003), 69.8% of the patients with self-injectable treatment were adherent (p=0.485) and 62.5% of the patients were adherent to their oral treatment (p=0.014).
Patient-Related Factors and Pharmacological Adherence
In our sample, necessity beliefs and concerns beliefs were not statistically associated with adherence. Results of the specific BMQ are presented in Table 2.
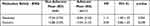 |
Table 2 Univariate Analyses Between BMQ Scores and Patient Adherence |
Table 3 presents the results of the selected subscales from the MSQOL-54, which assess quality of life, comparing adherent and non-adherent patients. The adherent group shows statistically significant better levels of quality of life in the cognitive function subscale than the non-adherent participants (p=0.040). Role limitations-emotional, emotional well-being and overall quality of life were not significantly associated with adherence, although a tendency to a higher score in the group of adherents can be observed.
 |
Table 3 Univariate Analyses Between MSQOL-54 Subscale Scores and Patient Adherence |
Predictors of Adherence to Pharmacological Treatments
A univariate logistic regression analysis was performed to quantify the association between adherence to DMTs and adherence predictors. Factors of the 5 WHO dimensions were included and a total of seven predictors were significantly associated with adherence to MS treatment: 1) social and economic factors: age (OR=0.96) and years of education (OR=0.82); 2) therapy-related factors: intravenous treatment (OR=4.60), alternative therapies not used (OR= 2.45), vitamin D adherence (OR=3.29) and duration of treatment (OR=0.11); and 3) patient-related factors: cognitive function (OR=1.02). None of the health care system factors or condition-related factors were significantly associated with adherence. Table 4 presents the results of the univariate analysis.
 |
Table 4 Predictors of Adherence to DMTs: Results of a Univariate Analysis and Multivariate Analysis |
Only two predictors maintained a statistical association with adherence to treatment in the multivariate model: years of education (OR=0.79) and intravenous treatment (OR=3.17). The results of the multivariate analysis are shown in Table 4.
Discussion
Adherence to DMTs in MS is a complex and multidimensional phenomenon. In this study, we aimed to identify predictors influencing adherence to MS treatment in Spain.
Even though our study included a limited number of patients, it can be considered representative of the MS population since the patient characteristics of our sample, mean age (M=44, SD=9.6) and proportion of patients with relapsing-remitting MS (78%) were consistent with those from a recent Spanish study that reported data from 490 patients with MS.2
Although there is great variability in adherence rates observed in the literature depending on the measurement methods used in the studies, our data were in line with previous studies. The adherence reported in our sample was 73%, which is very similar to the 71% and 75% reported in studies carried out in Spain using the Morisky–Green test6,25 and several studies in other countries using self-reported questionnaires that described mean adherence rates of 74%.5
Beliefs about DMTs were one of the patient-related factors studied in this research. Our study was focused on understanding how patients’ beliefs about medication could affect adherence, specifically if the perceived necessity of medication for maintaining health (Specific-Necessity Beliefs) is associated with adherence, and if the concerns about the adverse consequences of medication, like dependence or harmful long-term effects (Specific-Concerns Beliefs) could affect adherence.17 We have not found any significative association between MS patients’ beliefs and therapeutic adherence. Three studies have analyzed adherence in relation to medication beliefs in MS using the BMQ, with similar findings. Neter et al26 did not find significant differences between adherent and non-adherent patients in the necessity and concern beliefs. A German study by Pust et al21 also reported lack of significance in the BMQ Specific-Concern scale, and only non-adherent patients in first-line DMT treatment showed lower scores in the necessity beliefs. Thach and colleagues27 reported that perceived necessity and perceived concern were not associated with adherence to DMTs in the multivariate analysis. These findings are consistent with our data. Interestingly, BMQ necessity and concern scores were somewhat higher in our sample than in Thach’s US population, perhaps indicating a more conscious attitude towards medication (patient perceptions of medication benefits and risks), which may be related to our method of recruiting the patients (about 80% belong to a MS patient association). Horne et al28 conducted a meta-analysis of 94 studies using the BMQ in a wide range of long-term pathological conditions. In most of them, a higher adherence was associated with stronger perceptions of necessity and fewer concerns about treatment. This study is the first to be conducted in Spain which looks at medication beliefs in the MS population, therefore more research is needed to validate these data.
The other patient-related factor explored in this study in relation to adherence was quality of life. In our study we found that cognitive function, role limitations-emotional, emotional well-being and overall quality of life presented a tendency to a higher score in the group of adherents, but only cognitive function was statistically significant. This finding is consistent with another Spanish study that reported higher scores in the adherent group for each of the four dimensions of the MSQOL-54 questionnaire for injectable treatments and oral treatments.29 Our results are also in line with other studies6,30 which indicate that cognitive impairment is significantly associated with non-adherence. One of the possible consequences of cognitive impairment for adherence is the increase in forgetfulness. Interestingly, forgetfulness is the most common cause of poor adherence in our study and is also indicated in many studies.5,13,23
To our knowledge, there are no studies in our country which address the five dimensions in the WHO model of medication adherence. In other regions, some studies identified several key factors associated with adherence, such as age, gender, disability, depression, cognition or treatment satisfaction.5,13,14,31 In our study, only years of education and the route of administration were significantly associated with adherence to DMTs in the multivariate model.
Regarding the education level, our study shows that the odds of adherence decreased with years of education (OR=0.79; p=0.020), so we found higher adherence among patients with a lower education. In line with our results, a multicenter study conducted with n=2566 MS patients reported that completion of university education was a predictor of non-adherence.23 In a Norwegian study on follow-up of new diagnosis MS patients, high education was also a risk factor for stopping DMTs.32 However, these results are not consistent with those reported in other chronic conditions12; therefore, more studies with the MS population are needed to explain these data. Considering higher education level as a predictor of poor adherence, these persons are probably more informed regarding their disease and treatment and are more independent to make decisions. Healthcare professionals should be aware of this fact, since it seems contrary to general beliefs in other chronic pathologies, and patients with a higher education level may be at a greater risk of non-adherence.
Regarding the administration route, the positive association between intravenous treatment and adherence has been shown in previous studies. In accordance with our findings, a study in Spain6 reported that patients with intravenous treatments are more adherent than those with subcutaneous and oral administrations. Another study in Latin America33 also concluded that the adherence of patients to infusion therapies was higher compared to oral and injectable drugs. A possible explanation for these findings is that intravenous treatments are administered in a hospital by a healthcare professional, while oral and subcutaneous treatments are self-administered at home by the patient and forgetfulness is a major risk of non-adherence.
Suggestions to Improve Adherence
Adherence is essential to optimize the efficacy of treatments in MS patients.7 It is important that clinicians who are in regular contact with patients evaluate and provide support to patients at risk of non-adherence.8
As our study indicates, patients with a higher education level may be at a greater risk of non-adherence. Since this can be counterintuitive, healthcare professionals should pay special attention to this predictor to reinforce adherence in this patient profile.
As far as possible, when selecting a DMT, besides considering the safety and tolerability of the treatment, it is necessary to take into account the impact of the drug on patient needs and lifestyle.8 It is important to involve the patient in the decision-making process for selecting the route of administration. To this end, healthcare providers should be trained in communication skills and psychological competences to support patients.13
In the case of oral and injectable treatments, increasing follow-up of patients who self-administer their treatment could improve adherence rates. Additionally, to avoid forgetfulness, it may be useful to perform a cognitive assessment, send reminders or incorporate the caregivers in the treatment plan.8
Intervention in therapeutic adherence requires a multidisciplinary and individualized approach for each patient. It is essential that healthcare professionals have adequate training in therapeutic adherence in order to identify patients with a higher risk of non-adherence and select the most appropriate intervention strategy based on the causes of non-adherence.
Limitations
This study has some limitations, which mainly include the relatively small study size and restrictions inherent to patients’ reported data. The Morisky–Green test, despite being the most widely used method to assess adherence in the MS population, has the disadvantage that as a self-report, it tends to overestimate adherence.34 Another limitation is the potential recall bias, as patients answered questions regarding aspects some months ago. In addition, we only used four subscales from the MSQOL-54, so the study lacked other potentially relevant data regarding quality of life. Lastly, it is possible that patients who voluntarily agreed to participate in this survey have a more active role in their disease and treatment management, which may affect the results obtained.
Conclusion
In summary, our study assessed the non-adherence factors of the five dimensions in the WHO model in Spain. Most of the participants in the study reported adequate adherence to their pharmacological treatment. Regarding adherence factors, in the multivariate analysis, none of the patient-related factors (medication beliefs, quality of life) were significantly associated with pharmacological adherence. In this study, only low education and intravenous treatment were significant predictors of adherence to DMTs. More research is needed in order to confirm our findings in the MS population in Spain and evaluate the role of several psychological and quality of life variables in adherence to DMTs.
Acknowledgments
We would like to express our thanks to the AEDEM-COCEMFE federation, their associations members, patients and caregivers for their help completing the questionnaire. We would also like to particularly thank the healthcare professionals of the patient associations and hospitals who participated in the recruitment. We wish to express our thanks to the Unidad de Consultoría y Salud from Francisco de Vitoria University for their help with the recruitment. Lastly, we are very grateful to Suportias for their technical and organizational support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Multiple Sclerosis International Federation. Atlas of MS – 3rd Edition; 2020. Available from: https://www.msif.org/wp-content/uploads/2020/10/Atlas-Epidemiology-report-Sept-2020-Final-ES.pdf.
2. Campos-Lucas FJ, Fernández-Fernández Ó, Monge-Martín D, Moral-Torres E, Carrascal-Rueda P, Caballero-Martínez F. The evolution of multiple sclerosis in Spain over the last decade from the patient’s perspective. Mult Scler Relat Disord. 2021;57:103355. doi:10.1016/j.msard.2021.103355
3. Merino A, Ara JR, Fernández O, Pascual L, Torres E, Rodríguez-Antigüedad A. Consenso para el tratamiento de la esclerosis múltiple 2016. Sociedad Española de Neurología. Neurología. 2016;32. doi:10.1016/j.nrl.2016.02.026
4. Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011;5:73–84. doi:10.2147/PPA.S15702
5. Washington F, Langdon D. Factors affecting adherence to disease-modifying therapies in multiple sclerosis: systematic review. J Neurol. 2022;269(4):1861–1872. doi:10.1007/s00415-021-10850-w
6. Morillo Verdugo R, Ramírez Herráiz E, Fernández-Del Olmo R, Roig Bonet M, Valdivia García M. Adherence to disease-modifying treatments in patients with multiple sclerosis in Spain. Patient Prefer Adherence. 2019;13:261–272. doi:10.2147/PPA.S187983
7. Burks J, Marshall TS, Ye X. Adherence to disease-modifying therapies and its impact on relapse, health resource utilization, and costs among patients with multiple sclerosis. Clinicoecon Outcomes Res. 2017;9:251–260. doi:10.2147/CEOR.S130334
8. Remington G, Rodriguez Y, Logan D, Williamson C, Treadaway K. Facilitating Medication Adherence in Patients with Multiple Sclerosis. Int J MS Care. 2013;15(1):36–45. doi:10.7224/1537-2073.2011-038
9. Hempel S, Graham GD, Fu N, et al. A systematic review of modifiable risk factors in the progression of multiple sclerosis. Mult Scler. 2017;23(4):525–533. doi:10.1177/1352458517690270
10. Barnard E, Brown CR, Weiland TJ, Jelinek GA, Marck CH. Understanding barriers, enablers, and long-term adherence to a health behavior intervention in people with multiple sclerosis. Disabil Rehabil. 2020;42(6):822–832. doi:10.1080/09638288.2018.1510550
11. Heesen C, Bruce J, Gearing R, et al. Adherence to behavioural interventions in multiple sclerosis: follow-up meeting report (AD@MS-2). Mult Scler J Exp Transl Clin. 2015;1:2055217315585333. doi:10.1177/2055217315585333
12. World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003. Available from: https://apps.who.int/iris/handle/10665/42682.
13. Kołtuniuk A, Chojdak-łukasiewicz J. Adherence to therapy in patients with multiple sclerosis-review. Int J Environ Res Public Health. 2022;19(4):2203. doi:10.3390/ijerph19042203
14. Erbay Ö, Usta Yeşilbalkan Ö, Yüceyar N. Factors affecting the adherence to disease-modifying therapy in patients with multiple sclerosis. J Neurosci Nurs. 2018;50(5):291–297. doi:10.1097/JNN.0000000000000395
15. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies*. Bull World Health Organ. 2007;85(11):867–872. doi:10.2471/BLT.07.045120
16. Morisky D, Green L, Levine D. Concurrent and predictive-validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi:10.1097/00005650-198601000-00007
17. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
18. Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4(3):187–206. doi:10.1007/BF02260859
19. Val Jiménez A, Amorós Ballestero G, Martínez Visa P, Fernández Ferré ML, León Sanromà M. Estudio descriptivo del cumplimiento del tratamiento farmacológico antihipertensivo y validación del test de Morisky y Green [Descriptive study of patient compliance in pharmacologic antihypertensive treatment and validation of the Morisky and Green test]. Aten Primaria. 1992;10(5):767–770. Spanish.
20. Beléndez-Vázquez MB, Mijares AH, Horne R, Weinman J. Evaluación de las creencias sobre el tratamiento: validez y fiabilidad de la versión española del “Beliefs about Medicines Questionnaire.”. Int j Clin Health Psychol. 2007;7(3):767–779.
21. Pust GEA, Untiedt B, Weierstall-Pust R, et al. Medication beliefs in first-line and second-line treated multiple sclerosis patients. Mult Scler Relat Disord. 2020;42:102144. doi:10.1016/j.msard.2020.102144
22. Aymerich M, Guillamón I, Perkal H, et al. Adaptación al español del cuestionario específico MSQOL-54 para pacientes con esclerosis múltiple [Spanish adaptation of the disease-specific questionnaire MSQOL-54 in multiple sclerosis patients]. Neurologia. 2006;21(4):181–187. Spanish.
23. Devonshire V, Lapierre Y, Macdonell R, et al. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur J Neurol. 2011;18(1):69–77. doi:10.1111/j.1468-1331.2010.03110.x
24. Chowdhury MZI, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health. 2020;8(1):e000262. doi:10.1136/fmch-2019-000262
25. Saiz A, Mora S, Blanco J. Cumplimiento terapéutico con terapias modificadoras de la enfermedad de primera línea en pacientes con esclerosis múltiple. Estudio COMPLIANCE. Neurología. 2015;30(4):214–222. doi:10.1016/j.nrl.2013.12.008
26. Neter E, Glass-Marmor L, Wolkowitz A, Lavi I, Miller A. Beliefs about medication as predictors of medication adherence in a prospective cohort study among persons with multiple sclerosis. BMC Neurol. 2021;21:136. doi:10.1186/s12883-021-02149-0
27. Thach AV, Brown CM, Herrera V, et al. Associations between treatment satisfaction, medication beliefs, and adherence to disease-modifying therapies in patients with multiple sclerosis. Int J MS Care. 2018;20(6):251–259. doi:10.7224/1537-2073.2017-031
28. Horne R, Chapman SCE, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS One. 2013;8(12):e80633. doi:10.1371/journal.pone.0080633
29. Sánchez Martínez I, Cerdán Sánchez M, López Román J, et al. Possible influence of the route of treatment administration on treatment adherence in patients with multiple sclerosis. Clin Ther. 2020;42(5):e87–e99. doi:10.1016/j.clinthera.2020.03.005
30. McKay KA, Tremlett H, Patten SB, et al. Determinants of non-adherence to disease-modifying therapies in multiple sclerosis: a cross-Canada prospective study. Mult Scler. 2017;23(4):588–596. doi:10.1177/1352458516657440
31. Li P, Ladage VP, Berger J, et al. Disease-modifying therapy adherence and associated factors in a national sample of medicare patients with multiple sclerosis. Value Health. 2020;23(3):328–334. doi:10.1016/j.jval.2019.10.011
32. Grytten N, Aarseth JH, Espeset K, et al. Stoppers and non-starters of disease-modifying treatment in multiple sclerosis. Acta Neurol Scand. 2013;127(2):133–140. doi:10.1111/j.1600-0404.2012.01708.x
33. Alonso R, Rojas JI, Ramos J, et al. Evaluation of adherence to treatment in patients with multiple sclerosis from Latin America. Mult Scler Relat Disord. 2022;63:103915. doi:10.1016/j.msard.2022.103915
34. Fernández O, Agüera E, Agüera J, et al. Adherence to interferon β-1b treatment in patients with multiple sclerosis in Spain. PLoS One. 2012;7(5):e35600. doi:10.1371/journal.pone.0035600
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
