Back to Journals » Open Access Emergency Medicine » Volume 15
Factors Associated with Postintubation Hypotension Among Patients with Suspected Sepsis in Emergency Department
Authors Tangkulpanich P , Angkoontassaneeyarat C , Trainarongsakul T , Jenpanitpong C
Received 20 June 2023
Accepted for publication 1 November 2023
Published 14 November 2023 Volume 2023:15 Pages 427—436
DOI https://doi.org/10.2147/OAEM.S426822
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Panvilai Tangkulpanich, Chuenruthai Angkoontassaneeyarat, Thavinee Trainarongsakul, Chetsadakon Jenpanitpong
Department of Emergency Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Chetsadakon Jenpanitpong, Department of Emergency Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, Email [email protected]
Purpose: Postintubation hypotension (PIH) is a recognized complication that increases both in-hospital mortality and hospital length of stay. Sepsis is reportedly a factor associated with PIH. However, no study to date has examined which factors, including the intubation method, may be clinical predictors of PIH in patients with sepsis. This study aims to investigate factors associated with the occurrence of PIH in patients with suspected sepsis in emergency department.
Patients and Methods: This retrospective cross-sectional study was performed over a 5-year period (January 2013–December 2017) and involved patients with suspected sepsis who underwent endotracheal intubation in the emergency department of Ramathibodi Hospital. The patients were divided into those with and without PIH, and factors associated with the occurrence of PIH were analyzed. PIH was defined as any recorded systolic blood pressure of < 90 mmHg within 60 minutes of intubation.
Results: In total, 394 patients with suspected sepsis were included. PIH occurred in 106 patients (26.9%) and was associated with increased in-hospital mortality (43.00% in the PIH group vs 31.25% in the non-PIH group, P = 0.034). Multivariable logistic regression showed that the factors associated with PIH were an age of ≥ 61 years (adjusted odds ratio [aOR] 2.25; 95% confidence interval [CI] 1.14– 4.43; P = 0.019) and initial serum lactate concentration of > 4.4 mmol/L (aOR 2.00; 95% CI 1.16– 3.46; P = 0.013). Rapid sequence intubation and difference types of induction agents was unrelated to PIH.
Conclusion: Monitoring the development of PIH in patients with sepsis is essential because of its correlation with higher in-hospital mortality. This is particularly critical for older individuals and those with severe infections and high initial lactate concentrations.
Keywords: postintubation hypotension, sepsis, emergency department intubation
Introduction
Along with hypoxemia, arrhythmia, and cardiac arrest, postintubation hypotension (PIH) is among the most undesirable complications after emergency endotracheal intubation.1–5 A systematic review showed that in the emergency department (ED), the incidence of PIH ranged from 6.5% to 16.7% and reached 20% in critically ill patients.6 Postintubation hemodynamic decompensation increases both the in-hospital mortality and hospital length of stay.7,8
Sepsis is a life-threatening condition which is typically seen in the ED. Patients with sepsis manifest with a wide range of clinical severity, some patients presented with impaired oxygenation and ventilation which required emergency endotracheal intubation.9 Rapid sequence intubation (RSI) is an intubation technique widely used in the ED to facilitate high success rate of intubation. However, several studies have been reported numbers of immediate complication after RSI.10
Intravascular hypovolemia, increased intrathoracic pressure, and effects of anesthetic medications used in RSI are significant contributors to the development of PIH.11 Among the patients intubated by the RSI method, sepsis was a significant factor with increasing up to 9 folds of odd associated with the development of PIH. However, factors contributing to PIH in patients with suspected sepsis remain unclear.10 The objective of this study was to investigate the clinical factors associated with PIH, including RSI, in patients with suspected sepsis who undergoing intubation in the ED.
Materials and Methods
Study Design and Setting
This retrospective cross-sectional study was conducted at the ED of Ramathibodi Hospital, a university-affiliated super-tertiary care hospital in Bangkok, Thailand. The data were collected from the database and electronic medical record system of Ramathibodi Hospital from January 2013 to December 2017. This study was approved by the Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University (COA. MURA2017/564). The ethics committee waived the requirement for patient consent because of the nature of the study (medical record review). Patient data confidentiality was ensured, and the study complied with the Declaration of Helsinki.
Participants
Participants were patients with suspected or confirmed sepsis - defined as the presence (probable or documented) of infection together with systemic manifestations of infection with two of the four following clinical signs: body temperature of >38.3°C or <36.0°C, heart rate of >90 beats/minute, respiratory rate of >20 breaths/minute, alternating consciousness, and white blood cell count of >12,000/µL or <4000/µL or presence of >10% band forms.12
Patients who aged >15 years and underwent intubation in the ED were enrolled. Patients who were intubated before arrival at the ED and those who had developed cardiac arrest or systolic blood pressure (SBP) of <90 mmHg within 30 minutes before intubation were excluded.
Data Collection and Outcome Measures
Patients baseline characteristics including sex, age, body weight; comorbidities and current medications; pre-intubation laboratory assessments; patient disposition status and hospital length of stay were electronically extracted from the Ramathibodi Hospital database. Data including source of infection; time to receipt of antibiotics; amounts of intravenous fluid administration; indications and method of intubations; drugs and dosages used for facilitating intubation; hemodynamic parameters; as well as procedures or interventions before and after intubation were reviewed and collected from the electronic medical record system. A standardized data collection sheet and guidance were used for data acquisition. Regular meetings among the authors were conducted to identify and resolve any encounter problems during the data acquisition process.
Post-intubation hypotension (PIH) was defined as the occurrence of one of any following incidents within 60 minutes after intubation: SBP of <90 mmHg or a 20% decrease from the pre-intubation SBP, mean arterial pressure (MAP) of <65 mmHg, fluid resuscitation of >30 mL/kg or vasopressor administration.8
Statistical Analysis
Statistical analyses were performed with Stata software version 14.0 (StataCorp, College Station, TX, USA). Comparison of two independent proportions was used for the sample size calculation. The probability of the expected values (p) was 0.26 and 0.13, according to the prevalence of PIH among patients who underwent RSI and non-RSI as reported by Smischney et al.8 Therefore, the minimum sample size was determined to be 339 patients.
Categorical variables were presented as number and percentage (%), whereas numerical variables were presented as mean ± standard deviation (SD) or median and interquartile range (IQR), as appropriate. The chi-square test or exact probability test was used to compare independent categorical variables. Student’s t-test was used for parametric variables to compare two independent numerical variables, while the Wilcoxon rank-sum test was used for non-parametric variables.
The association of potential clinical factors with PIH was identified using exploratory modeling multivariable logistic regression, presented with adjusted odds ratio (aOR) and 95% confidence interval (95% CI). The selected clinical factors in this model consisted of the factors that had the significant association of PIH from the univariable analysis and from the literature review. All results were considered statistically significant at a P-value of <0.05.
There were 25 missing variables which 16 of them were missing <5%. The 3 variables with the most missing values were amount of intravenous fluid administered prior to intubation (44%), body weight (35%), and initial lactate level (24%). Multiple imputation using chained equations with 30 imputed datasets was performed to handle with the missing data.13,14
Results
In total, 394 patients with suspected sepsis who were intubated in the ED of Ramathibodi Hospital were enrolled (Figure 1). PIH occurred in 106 patients (26.90%) within 20 (5–38) minutes after intubation, most commonly from 0 to 5 minutes (26.42%) (Figure 2). The patients’ baseline characteristics are shown in Table 1. Most patients were male (55.58%), and their mean age was 70.83 ± 15.30 years. The mean age of patients in the PIH group was significantly higher than that in the non-PIH group (74.07 vs 69.64 years, respectively; P = 0.011). Likewise, when analyzed using the Youden index, the cut-off point was 61 years. The number of patients aged ≥61 years was significantly greater in the PIH than non-PIH group (86.79% vs 74.65%, respectively; P = 0.001).
 |
Table 1 Baseline Characteristics Between Patients with PIH and Non-PIH Groups |
 |
Figure 1 Study flow diagram. |
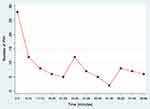 |
Figure 2 Incidence of PIH by time after intubation. Abbreviation: PIH, postintubation hypotension. |
Respiratory tract infection was the primary cause of sepsis (64.47%), and acute respiratory failure was the most common indication for intubation (85.53%). In the laboratory assessment, the PIH group had a higher median lactate concentration than the non-PIH group (4.6 vs 3.4 mmol/L, respectively; P = 0.014), while the other test results showed no statistically significant difference. There was also no difference between the two groups in the source of infection, comorbidities, antihypertensive medications, or treatments such as the time to antibiotic administration, amounts of intravenous fluids administered prior to intubation, and vasopressor drug use.
Table 2 shows the intubation process and outcome between the PIH and non-PIH groups. There was no significant difference in the pre-intubation hemodynamic parameters, including the mean MAP (P = 0.311) and the median shock index (P = 0.998). With respect to essential factors associated with intubation, the most common methods of choice were RSI (38.07%). Comparison between the PIH and non-PIH groups showed that neither RSI nor other intubation methods were associated with the incidence of PIH (P = 0.206).
 |
Table 2 Clinical Predictors Within Intubation Process and Outcomes Between PIH and non-PIH Groups |
The most commonly used medications for intubation were etomidate (35.03%) as an induction or sedative agent and succinylcholine (35.53%) for paralytic agent. The rate of midazolam use was significantly higher in the PIH than non-PIH group (21.7% vs 11.81%, respectively; P = 0.013), while other medications showed no difference. Moreover, 58.82% of drugs were correctly given at weight-based doses. Nevertheless, the reductions or increases in doses did not affect the likelihood of PIH (P = 0.092).
The overall mortality during hospitalization was 34.41% and was significantly higher in the PIH than non-PIH group (43.00% vs 31.25%, respectively; P = 0.034). However, the median hospitalization duration was not different between the two study groups (P = 0.632).
The variables associated with the occurrence of PIH were identified by the multivariable logistic regression analysis. Variables which were confirmed as potential clinical factors include age of ≥61 years with an adjusted OR of 2.25 (95% CI, 1.14–4.43) and initial lactate concentration of ≥4.4 mmol/L with an adjusted OR of 2.00 (95% CI, 1.16–3.46). However, use of midazolam was not statistically significantly increase the odds of occurrence of PIH (Table 3).
 |
Table 3 Univariable and Multivariable Logistic Regression Analyses of Clinically Significant Association for Postintubation Hypotension |
Discussion
In this retrospective observational study, we found that the incidence of PIH among suspected sepsis patients was 26.90% and the incidence mostly occur within 5 minutes after emergency intubation. We also found that an age of ≥61 years and initial lactate concentration of ≥4.4 mmol/L were the potential clinical factors associated with PIH, whereas pharmacological-facilitated intubation, adjustment for drug dosage, pre-intubation hemodynamic parameters, and interventions provided prior to intubation were not associated with PIH.
The incidence of PIH in this study was higher than that in other studies (11–20%).6–8,15 This may have resulted from the specific sepsis population being more likely to have hemodynamic instability than other diseases.16 Because PIH was associated with life-threatening complications such as post-intubation cardiac arrest, the incidence of overall mortality during hospitalization was also higher.8 Additionally, we also found that thirteen patients developed cardiac arrest after intubation (3.3%). Of these patients, seven had immediate cardiac arrest and six had pre-existing PIH.
In this study, an age of ≥61 years was a risk factor for PIH. This result is consistent with the finding reported by Hasegawa et al,15 which demonstrated that an age of ≥65 years had 2.6 folds of odds of PIH. Moreover, Smischney et al8 also found that every 10-year increase in age increased the incidence of PIH by 1.33 times. Concordance with previous study,17 higher lactate levels are not only associated with the severity of sepsis but also an increasing odds for PIH, accounting for a 2.00-times higher odds if the lactate level is >4.4 mmol/L.
Hypertension was the major comorbidity in our participants and was treated mainly by calcium channel blockers or beta blockers. Both antihypertensive agents cause slow pulse rates, and most medications in these categories are long-acting. As a result, they may obscure the tachycardia response during hypotension. Previous evidence showed that a shock index of >0.8 was associated with PIH.18,19 However, no statistical significance difference was found in this study. This may be resulted from the use of antihypertensive agents as well. We also investigated the relationship between the use of antihypertensive agents and PIH. However, we found no difference between the two groups in the present study, which was similar to the previous study reported by Heffner et al.7
According to the study, RSI was no association with PIH. This may be due to the higher rate of using etomidate as an induction agent among the study population, which has less effect on hemodynamic changes than other induction agents.19–22 Etomidate was mostly used in standard dosage (94.12% for PIH and 97.12% for non-PIH group) with an average of 0.30 ± 0.02 mg/Kg in both groups. We also found that PIH less occurred in patients receiving etomidate who were administered intravenous fluid aggressively (>30 mL/kg) prior to intubation. Expanded intravascular volume after aggressive fluid administration increases the cardiac output and leads to hemodynamic stability. Our finding is similar to that in a study of a pre-intubation protocol in which fluid resuscitation prevented hemodynamic collapse following intubation.23
Previous evidence reported that etomidate had a strong association with adrenal insufficiency (AI) and mortality in critically ill patients, especially patients with sepsis.24,25 A major concern in using etomidate as an induction agent is its inhibition of adrenal mitochondrial 11-β-hydroxylase activity which effects the production of cortisol. Consequently, a decline in catecholamine response of vascular and impairment of the renin-angiotensin-aldosterone system may occur.26 However, some evidence disproved that there was no association between etomidate and an increase in mortality.27,28 Thus, using etomidate as an induction agents for emergency intubation in the sepsis patients is controversial.29
This study had some limitations. First, this was a retrospective study conducted in monocentric institution, participants’ generalizability may be limited. Second, there are no specific studies had focused on patients with septicemia and the occurrence of PIH. This may affect to the sample size calculation of this study. Third, we defined sepsis using initially established criteria. Some of the patients were later found to have viral infections or other inflammatory responses; thus, our patients may not accurately represent the bacterial septicemia population. However, our definition is more practical considering the time to intubation in critically ill patients. We defined PIH within the extended range of 60 minutes after intubation. Many factors can affect the hemodynamic stability, such as the parameters of invasive mechanical ventilator, but there were not shown in this study because of recording limitations.
Finally, multiple variables were missing according to the nature of retrospective study. Thus, multiple imputation strategy was performed for handling with missing data; however, results should be cautiously interpreted. A prospective study involving a larger number of patients from multiple institutions may help to increase the predictive accuracy of the associated factors.
Conclusion
The incidence of PIH tended to be high among patients with sepsis undergoing endotracheal intubation, and the incidence was associated with in-hospital mortality. Monitoring for PIH should be undertaken, especially in elderly patients and those who have severe infections with high initial lactate levels.
Data Sharing Statement
The datasets analyzed in this study are not publicly available owing to privacy issues but are available from the corresponding author upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors have no financial or non-financial competing interests.
References
1. Dufour DG, Larose DL, Clement SC. Rapid sequence intubation in the emergency department. J Emerg Med. 1995;13(5):705–710. doi:10.1016/0736-4679(95)00089-S
2. Carley SD, Gwinnutt C, Butler J, Sammy I, Driscoll P. Rapid sequence induction in the emergency department: a strategy for failure. Emerg Med J. 2002;19(2):109–113. doi:10.1136/emj.19.2.109
3. Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34(9):2355–2361. doi:10.1097/01.CCM.0000233879.58720.87
4. Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008;34(10):1835–1842. doi:10.1007/s00134-008-1205-6
5. Theodosiou CA, Loeffler RE, Oglesby AJ, McKeown DW, Ray DC. Rapid sequence induction of anaesthesia in elderly patients in the emergency department. Resuscitation. 2011;82(7):881–885. doi:10.1016/j.resuscitation.2011.02.025
6. Green R, Hutton B, Lorette J, Bleskie D, McIntyre L, Fergusson D. Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. Cjem. 2014;16(1):69–79. doi:10.2310/8000.2013.131004
7. Heffner AC, Swords D, Kline JA, Jones AE. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(4):417.e9–13. doi:10.1016/j.jcrc.2011.08.011
8. Smischney NJ, Demirci O, Diedrich DA, et al. Incidence of and risk factors for post-intubation hypotension in the critically Ill. Med Sci Monit. 2016;22:346–355. doi:10.12659/MSM.895919
9. Srivilaithon W, Bumrungphanithaworn A, Daorattanachai K, et al. Clinical outcomes after a single induction dose of etomidate versus ketamine for emergency department sepsis intubation: a randomized controlled trial. Sci Rep. 2023;13(1):6362. doi:10.1038/s41598-023-33679-x
10. Lin CC, Chen KF, Shih CP, Seak CJ, Hsu KH. The prognostic factors of hypotension after rapid sequence intubation. Am J Emerg Med. 2008;26(8):845–851. doi:10.1016/j.ajem.2007.11.027
11. Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The physiologically difficult airway. West J Emerg Med. 2015;16(7):1109–1117. doi:10.5811/westjem.2015.8.27467
12. Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. doi:10.1097/CCM.0b013e31827e83af
13. Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64(5):402–406. doi:10.4097/kjae.2013.64.5.402
14. Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research-part 2: multiple imputation. Acad Emerg Med. 2007;14(7):669–678. doi:10.1197/j.aem.2006.11.038
15. Hasegawa K, Hagiwara Y, Imamura T, et al. Increased incidence of hypotension in elderly patients who underwent emergency airway management: an analysis of a multi-centre prospective observational study. Int J Emerg Med. 2013;6:12. doi:10.1186/1865-1380-6-12
16. Sakles JC, Laurin EG, Rantapaa AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31(3):325–332. doi:10.1016/S0196-0644(98)70342-7
17. Pansiritanachot W, Ruangsomboon O, Limsuwat C, Chakorn T. Independent risk factors of mortality in patients with sepsis receiving single-dose etomidate as an induction agent during rapid sequence intubation in a large tertiary emergency department in Thailand. BMC Emerg Med. 2022;22(1):94. doi:10.1186/s12873-022-00658-w
18. Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(6):587–593. doi:10.1016/j.jcrc.2012.04.022
19. Kim JM, Shin TG, Hwang SY, et al. Sedative dose and patient variable impacts on postintubation hypotension in emergency airway management. Am J Emerg Med. 2019;37(7):1248–1253. doi:10.1016/j.ajem.2018.09.015
20. Choi YF, Wong TW, Lau CC. Midazolam is more likely to cause hypotension than etomidate in emergency department rapid sequence intubation. Emerg Med J. 2004;21(6):700–702. doi:10.1136/emj.2002.004143
21. Shah SB, Chowdhury I, Bhargava AK, Sabbharwal B. Comparison of hemodynamic effects of intravenous etomidate versus propofol during induction and intubation using entropy guided hypnosis levels. J Anaesthesiol Clin Pharmacol. 2015;31(2):180–185. doi:10.4103/0970-9185.155145
22. Sharda SC, Bhatia MS. Etomidate compared to ketamine for induction during rapid sequence intubation: a systematic review and meta-analysis. Indian J Crit Care Med. 2022;26(1):108–113. doi:10.5005/jp-journals-10071-24086
23. Jaber S, Jung B, Corne P, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med. 2010;36(2):248–255. doi:10.1007/s00134-009-1717-8
24. Albert SG, Ariyan S, Rather A. The effect of etomidate on adrenal function in critical illness: a systematic review. Intensive Care Med. 2011;37(6):901–910. doi:10.1007/s00134-011-2160-1
25. Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis: a meta-analysis*. Crit Care Med. 2012;40(11):2945–2953. doi:10.1097/CCM.0b013e31825fec26
26. Thompson Bastin ML, Baker SN, Weant KA. Effects of etomidate on adrenal suppression: a review of intubated septic patients. Hosp Pharm. 2014;49(2):177–183. doi:10.1310/hpj4902-177
27. Gu WJ, Wang F, Tang L, Liu JC. Single-dose etomidate does not increase mortality in patients with sepsis: a systematic review and meta-analysis of randomized controlled trials and observational studies. Chest. 2015;147(2):335–346. doi:10.1378/chest.14-1012
28. Mohr NM, Pape SG, Runde D, Kaji AH, Walls RM, Brown CA. Etomidate use is associated with less hypotension than ketamine for emergency department sepsis intubations: a NEAR cohort study. Acad Emerg Med. 2020;27(11):1140–1149. doi:10.1111/acem.14070
29. Gagnon DJ, Seder DB. Etomidate in sepsis: understanding the dilemma. J Thorac Dis. 2015;7(10):1699–1701. doi:10.3978/j.issn.2072-1439.2015.10.21
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
