Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Factors Associated with HIV Risk and Vulnerability Among Injecting Drug Users in Afghanistan: A Narrative Review
Authors Rasikh AS
Received 18 March 2022
Accepted for publication 30 June 2022
Published 23 July 2022 Volume 2022:14 Pages 331—339
DOI https://doi.org/10.2147/HIV.S366970
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Ahmad Shekaib Rasikh1,2
1Department of Infectious Diseases, Kabul University of Medical Sciences, Kabul, Afghanistan; 2KIT Health (Royal Tropical Institute), Vrije Universiteit Amsterdam, Amsterdam, Netherlands
Correspondence: Ahmad Shekaib Rasikh, Tel +93791906514, Email [email protected]
Abstract: The number of human immunodeficiency virus (HIV) cases in Afghanistan is increasing mainly associated with injecting drug use (IDU). This study aimed to explore the risk and vulnerability factors associated with HIV infection among injecting drug users (IDUs) in Afghanistan in order to contribute to improving the response and reversing the concentrated HIV epidemic among this group. A narrative review of the literature was conducted to reach the objective. The modified social ecological model was used as conceptual framework for analysis of the HIV risk and vulnerability factors among IDUs at five levels. At the “individual level”, the injecting risk behaviors among IDUs such as sharing the injecting equipment and their sexual risk behaviors like unprotected sexual contact with multiple partners identified as immediate factors that put them at risk of HIV infection. At the “network level”, lack of HIV knowledge and low uptake of the harm reduction services were identified as the factors that increase their vulnerability. At the “community level”, massive drug production and easy access to illicit drugs, armed conflicts, massive internal and external migration, unemployment and poverty, high stigma and discrimination against IDUs, unsafe injecting locations such as under the bridges; and at the “public policy level”, punitive drug laws, and weak national political response to HIV and IDU were identified as determinants that add to the IDUs vulnerability to HIV. At the “stage of epidemic level”, the concentrated HIV epidemic among IDUs in the country poses a potential risk to uninfected IDUs and beyond. In conclusion, the IDUs in Afghanistan are highly at risk and vulnerable to HIV. An informed and multisectoral response is required to control the epidemic. A rapid expansion of the harm reduction interventions is urgently needed.
Keywords: Afghanistan, HIV, harm reduction, IDUs, risk, vulnerability
Introduction
Injecting drug use (IDU) is defined as the practice of injecting psychotropic or psychoactive substances through intravenous, intramuscular, or subcutaneous routes for non-medical purposes. These substances include, but are not limited to, opioids, amphetamine-type stimulants, cocaine, hypno-sedatives, and hallucinogens.1,2
IDU is a major global public health problem. According to the “World Drug Report 2021” by the United Nations Office on Drugs and Crime (UNODC) there are over 11 million injecting drug users (IDUs) worldwide of which 12.7% (about 1.4 million) are living with HIV. Approximately 10% of the new HIV infections worldwide is associated with IDU.3 According to a systematic review by Degenhardt et al in 2017 the evidence of IDU was documented in 179 out of 206 countries or territories in which the total population of IDUs was estimated 15.6 million with 17.8% HIV prevalence among them.4
IDUs are at increased risk of blood-borne infections including HIV and this risk is primarily attributed to sharing contaminated injecting equipment and their sexual risk behaviors like having multiple sexual partners.3,5 In addition, the determinants like drug production and trafficking, lack of knowledge, unemployment and poverty, population movement, unsafe injecting environments, social stigma and discrimination, punitive drug laws, and armed conflicts influence on the social structural production of HIV risk and vulnerability associated with IDU.6–8
The HIV risk is defined as the probability that a person may become infected with HIV due to their individual behaviors. While the HIV vulnerability results from a range of factors outside the control of individuals that reduce their ability to avoid the risk.9
The data about the number of HIV cases in Afghanistan is limited but it appears to be growing mainly driven by the IDU. According to the estimates by the United Nations program on HIV/AIDS (UNAIDS), the number of people living with HIV has increased from 4500 people in 2010 to 12,000 in 2020 (male to female ratio 2.6:1).10,11
Afghanistan remains the world’s largest producer of opium.12 According to the national drug use surveys, the total number of drug users in this country increased from 940,000 people in 2009 to 2.5 million in 2015.13,14 The dominant modes of drug consumption were reported smoking and ingesting; however, study shows that there is a growing tendency in transition to injecting among oral drug users and those with longer duration of use.15
The precise population of IDUs in Afghanistan is unknown. The first ever national drug use survey in 2005 estimated the number of IDUs in the country between 19,000 and 25,000 people.16 A study by Rasheed et al in 2019 estimated Afghanistan’s total number of IDUs 57,207 people indicating a significant increase.17
The first Integrated biological and behavioral surveillance (IBBS) in 2009 which studied IDUs in three cities of Afghanistan (Kabul, Herat, Mazar-i-Sharif) reported an average 7.4% HIV prevalence among them.18 The second and last round of the IBBS in 2012, which covered IDUs in five cities (Kabul, Herat, Mazar-i-Sharif, Jalalabad, and Charikar) reported the average HIV prevalence among them 4.4% ranging from 0.3% in Mazar-i-Sharif, 0.9% in Charikar, 1.0% in Jalalabad, 2.4% in Kabul, and 13.3% in Herat city (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
Research suggests that once HIV is established within the IDUs networks, the virus has the potential to spread among the general population through sexual contact.19 Understanding the factors that put the IDUs at risk and make them vulnerable to HIV will help the policy makers in devising appropriate interventions for reversing the epidemic and preventing spread of the virus to the general population. The purpose of this study is to explore the HIV risk factors among IDUs in Afghanistan and to identify the determinants making them vulnerable to the virus.
Methods
This paper is based on narrative overview of the literature on IDU and HIV in the world with focus on Afghanistan. A comprehensive search was conducted for finding the relevant literature. The electronic databases in the internet such as PubMed, Scopus, Web of Science, Trip database and Cochrane Library were searched to find peer reviewed articles. The gray literature was also reviewed using the Google and Google Scholar search engines. The websites of the concerned organizations like the UNODC, UNAIDS, WHO, The World Bank and the Ministry of Public Health of Afghanistan, were looked at for documents and survey reports. Only literature written in the English language was included. There was no limitation placed on the year of publication. The search terms (keywords) used during the search process either single or combined for finding the relevant literature are summarized in Box 1.
 |
Box 1 The Search Terms Used for Finding the Literature |
Conceptual Framework
The modified social ecological model (MSEM), developed by Baral et al in 2013 is used as framework of analysis of the HIV risk and vulnerability factors among IDUs. The MSEM is composed of five levels of risk for HIV infection among IDUs, namely the “individual level”, “network level”, “community level”, “public policy level”, and the level of “HIV epidemic stage” (Figure 1).20
 |
Figure 1 Modified social ecological model for HIV risk among IDUs. Note: Adapted from Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13(1):482. doi:10.1186/1471-2458-13-482.20 |
Results
The key elements of the five levels of risk at the conceptual framework (individual, network, community, public policy and stage of epidemic) levels in the context of Afghanistan will be discussed accordingly.
Individual Level
The individual level factors include the behaviors of individual IDUs that put them at risk of HIV infection. The main risk factors at this level include the IDUs injecting and sexual risk behaviors19,20 According to the IBBS 2012 on average 11% of all interviewed IDUs in five cities of Afghanistan had ever shared needles/syringes varied from 0.4% in Kabul to 33.2% in Herat city where the highest HIV prevalence was recorded among IDUs. Additionally, the use of non-sterile injecting equipment at least once in the past three months was reported 6.2% varied from 0.0% in Kabul to 24.5% in Herat city (Table 1) (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
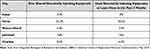 |
Table 1 Injecting Risk Behaviors Among IDUs in Five Cities of Afghanistan |
Additionally, a study by Todd et al in 2008 revealed that the receptive and distributive needle sharing among the IDUs in Kabul within the last six months were 28.2% and 28.7% respectively. The main reason for this practice was reported difficulty in obtaining new needles/syringes by the IDUs.21
The IBBS 2012 also revealed that on average 48% of the male IDUs have ever bought sex from a woman, varied from 29.3% in Kabul to 73.4% in Herat. 0.8% reported that they have ever had sex with a man and 16% had sex with a boy (Table 2) (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
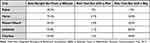 |
Table 2 Sexual Risk Behaviors Among IDUs in Five Cities of Afghanistan |
Additionally, a study by Todd et al in 2010 reported 27.6% condom use among the male IDUs in their prior sexual experience in four cities of Afghanistan (Kabul, Herat, Jalalabad and Mazar-i-Sharif). 58.1% had sexual experiences with the Female Sexual Workers (FSWs), while 25.7% had this experience with men or boys.22
Network Level
The network level factors predispose the IDUs to the risk of HIV through moderation of the individual level risk factors.19,20
According to the IBBS 2012 except for Herat city more than half of the IDUs in each city were illiterate. The majority (77%) of the IDUs had heard of HIV; however, only 20% had adequate knowledge about HIV prevention. There were misconceptions about HIV infection, for instance 55% of IDUs reported that a mosquito can transmit HIV and 35% believed that HIV can be acquired by sharing meal with HIV infected person (Table 3) (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
 |
Table 3 The HIV Transmission and Prevention Knowledge Among IDUs |
The standard Harm Reduction Services (HRS) proved to reduce the HIV transmission among the IDUs.23 The IBBS 2012 assessed the IDUs’ awareness about the HRS and also the rate of ever using these services in their lifetime. On average 53% of the IDUs in five cities reported that they are aware of the HRS varied from 80% in Mazar-i-Sharif to 2.2% in Charikar city. 74% of the IDUs who were aware of the HRS reported that they have used the HRS ranging from 0.4% in Charikar to 99% in Herat city (Table 4) (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
 |
Table 4 The Rates of Awareness and Ever Use of the HRS Among IDUs |
Furthermore, a study by Todd et al in 2009 indicated that the HRS available in Kabul are perceived to be insufficient for those in need of services, resulting in underutilization.25 Another study by Todd et al that have assessed utilization of addiction treatment among IDUs in Kabul revealed that majority (94%) of the IDUs felt urgent need for treatment, of whom, 56.3% reported inability to access treatment.24
Community Level
Illicit drug use including injecting is highly stigmatized in Afghan communities. The use of intoxicant drugs in the Afghan society is a cultural taboo and strongly disapproved. It is also a criminal act and punishable under law.26 The drug users face different kinds of social and legal discrimination. The stigma and criminalization associated with IDU leads to social marginalization of IDUs and limits their access to prevention and treatment services.26
About 85% of the world’s opium is produced in Afghanistan. Beside exporting a substantial amount of produced heroin and opium, about 10% is believed to be consumed inside the country. In 2015 the drug use prevalence rate was reported 7.3% of the adult population. The widespread and easy access to illicit drugs has led to increase in the number of drug users.12,14
Afghanistan has been suffering from more than four decades of protracted armed conflicts. It is believed that the conflicts affected and displaced populations are vulnerable to diseases including HIV.28,29
During the decades of armed conflicts approximately 8 million Afghan populations fled to foreign countries. As of 2005 about 5.7 million Afghans had returned home mainly from Pakistan and Iran where relatively higher HIV prevalence reported particularly among IDUs (20.8% among IDUs in Pakistan and 14.3% in Iran).30,39 In a study in Quetta, a city in Pakistan bordering with Afghanistan, 24% HIV prevalence was reported among a mixed group of Afghan and Pakistani IDUs. Compared to Pakistani IDUs, displaced Afghan IDUs exhibited lower level of knowledge about HIV transmission and were engaged in high-risk behaviors.31 The Afghanistan national drug use survey in 2009 revealed that almost one-third of drug users reported that they started using drug in Iran and one in ten began using in Pakistan.13
According to the IBBS 2012 on average 61% of all IDUs in five cities reported that they have lived outside Afghanistan in the past ten years varied from 93.3% in Herat city bordering with Iran to 42.4% in Charikar city (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
The association between unemployment, poverty and the risk of HIV among IDUs in Afghanistan has not been studied yet; however, studies in neighboring countries like Iran and Uzbekistan revealed that unemployed IDUs were more likely to practice risky injecting and sexual behaviors.30 According to the IBBS 2012, about 6% of IDUs reported that they are unemployed. On average 40% of those IDUs who reported having a monthly income said that they earned from 1000 to 5000 Afghani (approximately USD 15–60) (Integrated Biological & Behavioral Surveillance (IBBS) in Selected Cities of Afghanistan, Personal Communication, May, 2015).
Research suggests that the safety of the physical environment in which drug injecting takes place influences on the risk behaviors of IDUs; the risky behaviors are more common in unsafe environments such as visible areas with limited privacy and security.27,30 Studies in Iran, Bangladesh and Pakistan revealed that injecting outside the home increased the risk of contracting HIV associated with injecting and sexual risk behaviors.30 According to the 2008 mapping assessment of IDUs in three cities of Afghanistan, 32.1% of the IDUs reported that they inject at home and the majority (67.9%) reported that they inject outside home. The most frequent injecting locations outside home were reported parks (26.2%), sewers (21.0%), under the bridges (16.9%), graveyards (13.2%), alleys (11.3%), and the streets (4.3%). The IDUs who have been injecting outside home reported that they have established networks with other IDUs.32
Public Policy Level
The Government of Afghanistan was committed to international accords and declarations in fight against HIV/AIDS and had consistently renewed its commitments. At the national level, the government had adopted the millennium development goals (MDGs) including the MDG-6 aiming to prevent HIV among IDUs 50% by 2015. The government was also committed to provide universal access to anti-retroviral therapy (ART) and HIV prevention services for drug users.30,33
The establishment of the National AIDS Control Program (NACP) in 2003 was the first national response to HIV/AIDS in Afghanistan. The national HIV/AIDS policy was devised for guiding a multisectoral HIV response; however, it is lacking legal status and roles and responsibilities of the sectors involved. The HIV/AIDS coordination committee was established in 2007 to coordinate the HIV response and to advocate for enhancing HIV/AIDS services in the country; however, its legal status and the degree of autonomy is not defined.30,34
Although the harm reduction strategy was developed in 2005, it seems to have failed in the implementation phase as limited proportion of IDUs are covered by these services (only 25%). In 2012 Afghanistan was among the countries which 75–100% of its financial resources for response to HIV/AIDS came from external sources. Due to financial gaps the interventions which were proposed in the national strategic framework were not accomplished successfully.30
The impact of punitive drug laws on the risk of HIV among IDUs has not been studied in Afghanistan; but a study in Vietnam suggested that the punitive drug laws was associated with increased risk of HIV among IDUs linked with increased injecting risk behaviors.35
Afghanistan is an Islamic country. Based on the principles of the Islam religion illicit drug use is strictly forbidden. Similarly, the illicit drug use including injecting is illegal and punishable by law. Criminalization of drug use and punishment of drug users might encourage shifting to injecting instead of other routes such as smoking in order to keep their drug use status secret.30
HIV Epidemic Stage
The stage of the HIV epidemic within a network, community, and country determines the risk of HIV acquisition for the individuals in that network, community and country.20
Taking into account the assumption made in the MSEM20 and considering the above data, the uninfected IDUs are at high risk of contracting the virus due to the concentrated HIV epidemic among the IDUs networks.
Discussions
Injecting drug use has increasingly become an important cause of HIV transmission in the world including Afghanistan.17,36 Although the HIV prevalence among the general population in Afghanistan is still low (<0.1%), but the UNAIDS data indicates that the number of people living with HIV has been increasing mainly attributed to IDU.10,11 This study meant to explore the HIV risk and vulnerability factors among IDUs who are the most affected group in Afghanistan. Understanding these underlying factors would help the policy makers to tackle the HIV problem in the country effectively and better implement prevention interventions. In addition, it would also help in reducing the potential risk of the spread of the virus among the general population.
The MSEM which was used as the conceptual framework helped this study to analyze the HIV risk and vulnerability factors among IDUs in context of Afghanistan at different levels. The MSEM is based on the assumption that in addition to the individual level risks that are necessary for transmission of the virus, the higher order social and structural determinants (network, community, policy, stage of epidemic) represents vulnerability factors beyond the control of individual IDUs.20
Consistent with the findings of international literature, the main immediate risk factors at the individual level for HIV transmission among IDUs in Afghanistan identified the shared use of injecting equipment and unsafe sexual contact with multiple partners such as women, men, and boys. Considering the HIV transmission dynamics described by Strathdee et al,19 and also looking at the injecting and sexual risk behaviors of IDUs, the HIV epidemic among IDUs in Afghanistan has the potential to ultimately find its way among the general population which might complicate the situation and the response to HIV/AIDS in the country.7
There are several higher order social and structural determinants specific for Afghanistan context that make the IDUs in this country vulnerable to HIV. Inadequate knowledge about HIV transmission and ways of prevention among IDUs in Afghanistan is one of the main determining factors that add to their vulnerability to HIV as it has been proven anywhere else in the world. A research in Vietnam indicated that high injecting and sexual risk behaviours among people who inject drugs are associated with lack of HIV transmission and prevention knowledge.37 The role of harm reduction interventions as an international evidence-based best practice in reduction of HIV risk among IDUs has been proven. Only one quarter of the total estimated IDUs in Afghanistan are reported to have been covered by the harm reduction of services which further increases IDUs vulnerability.38
Afghanistan has remained the largest producer of opium in the world. Besides massive production and easy access to illicit drugs, the physical and psychological trauma of decades of armed conflicts appears to have contributed to dramatic increase in the number of drug users. In addition, the repatriation and deportation of large numbers of refugees mainly from Iran and Pakistan, where higher HIV prevalence was reported particularly among IDUs, is considered an important contributing factor in expansion of the HIV epidemic in Afghanistan.
The data suggests that parallel with significant rise in the overall population of drug users in the country, the number of IDUs has also increased raising concerns about establishment of a larger extent HIV epidemic among the IDUs.14 Lack of protection for the human rights of IDUs lead to social and legal stigma and discrimination against them, and lack of anti-discriminatory law further contribute to the marginalization of IDUs and thus increases their vulnerability to HIV. The harassment and detainment of the IDUs by police, and lack of access to the HRS are clear evidence of the violation of their human rights.
There is a research gap on the HIV among IDUs in Afghanistan. No nationwide study on the HIV among IDUs in this country has been conducted so far. A mapping and situation assessment of the key populations including IDUs was conducted in 2008 but covered only three cities. Similarly, the IBBS survey conducted in 2009 and 2012 studied the key populations in three cities and five cities respectively which did not provide national figures. Except for the southeast city of Jalalabad, there is no information available about IDUs and HIV in southern parts of the country where the majority of Afghanistan’s drug is produced. In addition, the two rounds of IBBS did not provide information about the association of social and structural determinants with the risk of HIV among IDUs. As a result, lack of information could hinder the response to HIV/AIDS in the country.
To respond to the HIV among IDUs effectively, it is crucial to target simultaneously the individual level risk factors and where possible the higher order social and structural determinants at the network, community and the public policy levels.
Conclusion
The reviewed literature indicates that there are several underlying factors putting IDUs in Afghanistan at risk and making them vulnerable to HIV. Their injecting risk behaviors such as shared use of non-sterile injecting equipment and their sexual risk behaviors like unprotected sexual intercourse with multiple partners are the factors that directly put them at risk. In addition, the higher order social and structural determinants like lack of HIV transmission and prevention awareness, low coverage and low uptake of the HRS, unsafe injecting locations, influx of refugees, stigma and discrimination, armed conflicts, poverty, enforcement of punitive drug laws, and a weak national political response are the factors that increase their vulnerability to HIV. The current response seems insufficient as the number of HIV cases has been increasing in the country. A multisectoral response is required to address the HIV epidemic among the IDUs effectively. Expansion of the harm reduction services as an international evidence-based best practice is urgently required to achieve this goal.
Acknowledgments
This paper is based on a thesis written and submitted to the KIT Health (Royal Tropical Institute) and Vrije Universiteit Amsterdam, Netherlands for the partial fulfilment of the requirement for the master studies of the author in international health.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Rasikh AS HIV risk and vulnerability among injecting drug users in Afghanistan; 2022. Available from: https://bibalex.org/baifa/en/resources/document/466470.
2. World Health Organization/UNAIDS. HIV and young people who inject drugs: a technical brief; 2015. Available from: https://www.unaids.org/sites/default/files/media_asset/2015_young_people_drugs_en.pdf.
3. UNODC. World drug report 2021; 2021. Available from: https://www.unodc.org/res/wdr2021/field/WDR21_Booklet_1.pdf.
4. Degenhardt L, Peacock A, Colledge S, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Heal. 2017;5(12):1192–1207. doi:10.1016/S2214-109X(17)30375-3
5. Todd CS, Abed AMS, Strathdee SA, et al. HIV, hepatitis C, and hepatitis B infections and Associated risk behavior in injection drug users, Kabul, Afghanistan. Emerg Infect Dis. 2007;13(9):1327–1331. doi:10.3201/eid1309.070036
6. UNODC. Afghanistan opium survey 2021; 2022. Available from: https://www.unodc.org/documents/crop.monitoring/Afghanistan/Afghanistan_Opium_Survey_2021.pdf.
7. Swain P, Das JK, Jha S, Sharnngadharan GK. Determinants of HIV positivity among injecting drug users in Delhi and Punjab. Indian J Sex Transm Dis AIDS. 2017;38(2):121–127. doi:10.4103/2589-0557.216990
8. Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. doi:10.1016/j.socscimed.2004.12.024
9. WHO/UNAIDS. Addressing societal causes of HIV risk and vulnerability: report on the global AIDS Epidemic; 2008. Available from: http://data.unaids.org/pub/GlobalReport/2008/jc1510_2008_global_report_pp63_94_en.pdf.
10. UNAIDS. Country factsheets: Afghanistan HIV and AIDS Estimates; 2020. Available from: https://www.unaids.org/en/regionscountries/countries/afghanistan.
11. UNAIDS/WHO/UNICEF. Afghanistan Country slides; 2021; Available from: https://www.aidsdatahub.org/resource/afghanistan-country-slides.
12. UNODC. Drug situation in Afghanistan 2021, latest findings and emerging threats; 2021. Available from: https://www.unodc.org/documents/data-and-analysis/Afghanistan/Afghanistan_brief_Nov_2021.pdf.
13. UNODC. Drug use in Afghanistan: 2009 survey; 2009. Available from: https://www.unodc.org/documents/data-and-analysis/statistics/Drugs/Drug%20use/Drug_use_in_Afghanistan_2009_survey.pdf.
14. Colombo Plan. Afghanistan national drug use survey 2015; 2015: Available from: https://colombo-plan.org/wp-content/uploads/2020/03/Afghanistan-National-Drug-Use-Survey-2015-compressed.pdf.
15. Hamzeh B, Najafi F, Heydarpour F, Moradinazar M, Moradinazar Z. The main factors affecting the tendency for “ injection drug use”. Int J High Risk Behav Addict. 2018;In Press. doi:10.5812/ijhrba.12646
16. UNODC. Afghanistan drug use survey 2005; 2005. Available from: https://www.unodc.org/pdf/afg/2005AfghanistanDrugUseSurvey.pdf.
17. Rasheed A, Sharifi H, Wesson P, et al. Mapping and population size estimates of people who inject drugs in Afghanistan in 2019: synthesis of multiple methods. PLoS One. 2022;506:1–23.
18. Johns Hopkins Bloomberg School of Public Health. Integrated Behavioral & Biological Surveillance (IBBS) in Afghanistan; findings of 2009 IBBS survey; 2010.
19. Strathdee SA, Hallett TB, Bobrova N, et al. HIV and risk environment for injecting drug users: the past, present, and future; 2010. Available from: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)60743-X/abstract.
20. Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13(1):482. doi:10.1186/1471-2458-13-482
21. Todd CS, Abed AMS, Scott PT, et al. Correlates of receptive and distributive needle sharing among injection drug users in Kabul, Afghanistan. Am J Drug Alcohol Abuse. 2008;34(1):91–100. doi:10.1080/00952990701764771
22. Todd CS, Nasir A, Stanekzai MR, et al. Prevalence and correlates of syphilis and condom use among male injection drug users in four Afghan cities. Sex Transm Dis. 2010;37(11):719–725. doi:10.1097/OLQ.0b013e3181e2c76a
23. Wodak A, Maher L. The effectiveness of harm reduction in preventing HIV among injecting drug users. N S W Public Health Bull. 2010;21(3–4):69–73. doi:10.1071/NB10007
24. Todd CS, Abed AMS, Scott PT, Safi N, Earhart KC, Strathdee SA. A cross-sectional assessment of utilization of addiction treatment among injection drug users in Kabul, Afghanistan. Subst Use Misuse. 2009b;44(3):416–430. doi:10.1080/10826080802347669
25. Todd CS, Stibich MA, Stanekzai MR, et al. A qualitative assessment of injection drug use and harm reduction programmes in Kabul, Afghanistan: 2006–2007. Int J Drug Policy. 2009a;20(2):111–120. doi:10.1016/j.drugpo.2007.11.022
26. Ministry of Public Health. Harm reduction practical guidelines 2008–2010; 2007. Available from: http://www.ilo.org/wcmsp5/groups/public/—ed_protect/—protrav/—ilo_aids/documents/legaldocument/wcms_174664.pdf.
27. Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82(1):125–156. doi:10.1111/j.0887-378x.2004.00304.x
28. UNHCR. HIV/AIDS among conflicts affected and displaced populations: dispelling myths and taking action; 2004. Available from: https://www.unhcr.org/afr/4162693e4.pdf.
29. Mock NB, Duale S, Brown LF, et al. Conflict and HIV: a framework for risk assessment to prevent HIV in conflict-affected settings in Africa. BioMed Cent. 2004;16:1–16.
30. Sharifi K Injecting drug use and HIV vulnerability in Afghanistan. 2012. Available from: https://books.google.com.af/books?id=xx1RtwAACAAJ.
31. Zafar T, Brahmbhatt H, Imam G, Hassan S, Strathdee SA. HIV knowledge and risk behaviors among Pakistani and Afghani Drug Users in Quetta, Pakistan. J Acquir Immune Defic Syndr. 2003;32(8):394–398. doi:10.1097/00126334-200304010-00008
32. The World Bank. Mapping and situation assessment of key populations at high risk of HIV in three cities of Afghanistan; 2008. Available from: https://openknowledge.worldbank.org/bitstream/handle/10986/17938/437330NWP0Box31gAfghanistanApril708.pdf?sequence=1.
33. Islamic Republic of Afghanistan. Afghanistan National Development Strategy 1387–1391 (2008–2013); 2007. 288. Available from: http://www.diplomatie.gouv.fr/en/IMG/pdf/Afghanistan_National_Development_Strategy_eng.pdf.
34. Rasoul MZ, Wodak A, Claeson M, Friedman J, Sayed GD Responding to HIV in Afghanistan. 2005;2167–2169. Available from: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(07).61911-4/abstract
35. Ahmed T, Long T, Huong P, Stewart D. Drug injecting and HIV risk among injecting drug users in Hai Phong, Vietnam: a qualitative analysis. BMC Public Health. 2015;15(1):32. doi:10.1186/s12889-015-1404-3
36. Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372(9651):1733–1745. doi:10.1016/S0140-6736(08)61311-2
37. Lim TW, Davis WW, Quan VM, et al. Association between HIV knowledge and risk behavior in persons who inject drugs in Thai Nguyen, Vietnam. Southeast Asian J Trop Med Public Health. 2014;45(6):1425–1436.
38. Todd CS, Safi N, Strathdee SA. Drug use and harm reduction in Afghanistan. Harm Reduct J. 2005;2:13. doi:10.1186/1477-7517-2-13
39. Rahimi J, Gholami J, Amin-Esmaeili M, et al. HIV prevalence among people who inject drugs (PWID) and related factors in Iran: a systematic review, meta-analysis and trend analysis. Addiction J. 2020;115(4). 605–622.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
