Back to Journals » International Journal of General Medicine » Volume 15
Factors Associated for COVID19 Severity Among Patients Treated at Selgalu Treatment Center Assosa in Ethiopia: A Case–Control Study
Received 8 December 2021
Accepted for publication 9 March 2022
Published 24 March 2022 Volume 2022:15 Pages 3303—3313
DOI https://doi.org/10.2147/IJGM.S351125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Dano Gutata,1 Zewdie Aderaw Alemu2
1Assosa General Hospital, Benishangul Gumuz Regional State Health Bureau, Asosa, Ethiopia; 2College of Health Sciences Public Health Department, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Zewdie Aderaw Alemu, College of health sciences Public health department, Debre Markos University, PO Box 269, Debre Markos, Amhara Regional State, Ethiopia, Tel +251 911550926, Email [email protected] Dano Gutata, Assosa General Hospital, Benishangul Gumuz Regional State Health Bureau, Asosa, Ethiopia, Tel +251917071159, Email [email protected]
Background: Most people infected with the SARS-CoV-2 virus experienced mild to moderate respiratory illness and recovered without requiring special treatment. However, some became seriously ill with conditions that require medical attention and intensive care unit (ICU) admission. Severity varies among individuals; this may be due to age differences and the presence of underlying disease conditions.
Objective: To identify factors associated with disease severity among COVID19 patients treated at Selgalu treatment center from November 1, 2020, to April 30, 2021.
Methods: A case–control study was implemented among patients admitted to Selgalu COVID19 treatment center in October 2021. A 210 (70 severe disease and 140 non-severe diseases), cases (disease severity), and controls (non-severe disease). Data entered to Epi data 4.6, exported to SPSS 25. A Chi-square test with a p-value of < 0.05 was used as a statistically significant difference between characteristics of disease severity and non-severity of disease. Multivariable binary logistic regression was used to determine variables associated with disease severity based on an adjusted odds ratio with 95% CI and p-value < 0.05.
Results: 210 (70 cases and 140 controls) selected charts in this study. Patients age category between 40– 59 [AOR: 5.30 (2.27– 12.34)], aged 60 or older [AOR: 3.85 (1.39– 10.64)], patients with fever [AOR: 3.98 (1.59– 9.96)], fatigue [AOR: 3.14 (1.50– 6.54)], and hypertensive patients [AOR: 3.68 (1.53– 8.82)] were significantly predictors for COVID19 disease severity after adjusting for other variables.
Conclusion: From this study, we conclude that being age 60 or older and 40– 59 age groups, having symptoms of fever, fatigue, and underlying comorbid illness hypertension. Were identified a significant predictor of severe COVID-19 disease; despite our limitation of study data highlights the important factors associated with disease severity with covid19 admitted to Selgalu treatment center.
Keywords: disease severity, multivariate, regression, Selgalu, Assosa
Introduction
In December 2019 Wuhan city of china reported the first severe acute respiratory syndrome infectious disease caused by the SARS-CoV-2 virus. Most people infected with the novel coronavirus experienced mild to moderate respiratory illness and recovered without requiring special treatment. However, some became seriously ill with conditions that require medical attention. Among people more likely to develop serious illnesses were older people and those with underlying medical conditions like cardiovascular disease, diabetes, chronic respiratory disease, or cancer. Although anybody can get sick with COVID-19 and become seriously ill or die at any age.1
Severity varies among individuals; this may be due to age differences and the presence of underlying disease conditions.2 Additionally co-infections that are noted when the patients presented for care or that develop during treatment also complicate treatment and recovery. While most patients with severe COVID-19 disease required intensive care unit (ICU) admission.3
Although the number of incident cases, severity of the disease, and fatality rate in Ethiopia are lower than the rest of the world. Ministry Of Health reported that patients need ICU beds increasing in the country and if it continues to spread by this level our health facilities have been exhausted and patients in need of ICU beds and mechanical ventilators were rising so fast that the problem may overwhelm the whole healthcare system.4 Moreover, it continues to be a bear a significant challenge to facilities due to the shortage of appropriate equipment and medications to manage severely ill and critical patients as the number of patients in need of the ICU has risen sharply.5
Identifying risk factors that predict COVID-19 severity is crucial in guiding clinical care, early recovery, and preventing further complications.6 Therefore, the findings of this research will be of great contribution in terms of preventing the spread of the virus that is still claiming thousands of lives around the world It also provides an input to improve the quality of care patients receive and prevent complications. Furthermore, researchers can use the results of this study as baseline data while conducting a similar study in the future.
Methodology
Study Area
The study was done from November 1, 2020, to April 30, 2021, at Selgalu COVID-19 treatment center in Assosa, Ethiopia. The treatment center was previously established for routine health center service and later on was exclusively dedicated to COVID-19 treatment by the regional health bureau. With a capacity of 4 ICU rooms and can accommodate us maximum of 100 patients.
Study Design
A health Institution-based unmatched case-control study design was done.
Study Population
COVID-19 Patients with confirmed RT-PCR who were admitted to Selgalu treatment center with a diagnosis of SARS-COV2 into Selgalu COVID-19 treatment center from November 1, 2020, to April 30, 2021.
- Case: COVID-19 Patients with confirmed RT-PCR treated to Selgalu treatment Centre and with the severe disease based on federal ministry of health Ethiopia admission criteria for COVID-19.
- Control: COVID-19 Patients with confirmed RT-PCR treated to Selgalu COVID-19 treatment Centre and with the non-severe disease.
Inclusion and Exclusion Criteria www.google.com
Records of patients consecutively admitted to the Selgalu COVID19 treatment Center from November 1, 2020, to April 30, 2021, based on Federal Ministry of Health Ethiopia admission criteria for COVID-19 disease.
Sample Size Determination
Patients treated consecutively to the Selgalu COVID19 treatment Center from November 1, 2020, to April 30, 2021, were collected and reviewed.
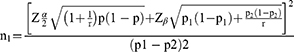
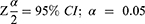
The sample size was used case-control study sampling, with one to two ratio of a case to control assumption. The proportion of death who were exposed for shortness of breath was 38.4% and the proportion of patients discharged alive and exposed for shortness of breath was 61.6% from a previous case-control study at Millennium covid19 care center, Addis Ababa, Ethiopia.7
n1 = Number of cases
P1= Percent of cases exposed for shortness of breath = 38.4%
P2= Percent of control with exposed for shortness of breath = 61.6%
10% added for missing data
Total sample size =210 with 70 severe disease and 140 non-severe disease study participants.
Sampling Technique
Cases were selected patients treated severely in the center during the study period
To select non-severe diseases simple random sampling technique was implemented
Study Variables
Dependent Variable
COVID-19 Severity (Non-severe, Severe,)
Independent Variables
Demographic variables:
- Age
- Sex
Being Symptomatic;
- Cough
- Fever
- Shortness of breath
- Chills
- Fatigue
- Sore throat
- Fast breathing
- Joint pain
- Back pain
- Headache
- Chest pain
- Loss of appetite
- Diarrhea, and others
Comorbidities (pre-existing underline chronic disease):
- Diabetes mellitus
- Hypertension
- Heart disease
- Lung disease
- Asthma
- HIV/AIDS
Baseline vital signs:
- Oxygen saturation level
- Body temperature
- Pulse rate
- Respiratory rate
- Blood pressure.
Standard Definition
Data Collection Procedure and Technique
A data collection tool was adopted from a standardized validated data tool based on variables of Patients’ Records. I contain demographic data, medical charts, clinical status, and outcome data with PCR confirmation for COVID-19. A 5% pretested data collection tool of selected patients record was prepared; training was given for three data collectors (BSc nurse) for two days. After data was collected, the principal investigator was rechecked the completeness and consistency before transferring it into computer software.
Data Processing and Analysis
Data were entered into Epi data software version 4.6 and transported to SPSS version 25.0 for analysis. Frequencies, proportions, and summary statistics were used to describe the study population with relevant variables and presented in tables Descriptive data was carried out for most variables using statistical measurements and displayed using tables, texts, and charts.
Chi-square was used to test the presence of a statistically significant difference, before analysis. To reduce the excessive number of variables and instability of the model, only variables with P-value < 0.25 in the Univariate binary logistic regression analysis were considered for inclusion in the multivariable binary logistic regression analysis to control for the effect of co-founder. The necessary assumption of logistic regression was checked using the Hosmer and Lemeshow goodness of fit test (chi-square=1.613, df=7, P-value =0.978). Results from multivariable logistic regression analysis were reported in the form of adjusted odds ratio (AOR) at 95% Confidence Intervals with 5% levels of significance. Variables with P-value < 0.05 in the multivariable final model were considered as independently associated with the outcome variable.
Ethical Considerations
The study received ethical approval from Selgalu COVID-19 treatment center review board (Reference number: SEL/104/13); the study did adversely not affect the rights and welfare of the subjects. The chart was reviewed using only Medical record numbers and Access to the collected data confidentiality issue maintained by the principal investigator.The study was conducted in compliance with the Declaration of Helsinki.
Results
Demographic Characteristics
A total of two hundred ten charts (70 severe diseases and 140 non-severe) were included in the study with a response rate of 100%. Almost two-thirds of the charts were 167 (79.5%) male. Close to half of them were 98 (46.7%) aged less than 40 years old. Among cases, the majority of 36 (17.1%) were aged between 40–59 years (Table 1).
 |
Table 1 Demographic Characteristics of Covid-19 Patients Treated at Selgalu Covid-19 Treatment Center in Assosa, 2021 (210) |
Underlying Pre-Existing Chronic Disease Characteristics
Patients’ charts showed that Sixty seven (31.9%) of the patients was a history of underlying pre-existing chronic disease. Among reported co-morbidity hypertension (HTN) forty (19%) was common. From this majority 24 (11.4%) of them were from the case and 16 (7.6%) are from controls followed by diabetes mellitus (DM) twenty-seven 27 (12.9%), among this 14 (6.7%) of them were from the case and 13 (6.2%) are from controls. The rest of the comorbidities with small number charts were Renal disease 6(2.9%) and HIV/AIDS 4(1.9%), respectively, and cardiovascular disease (CVD) 5(2.4%) (Table 2).
 |
Table 2 Comorbid Illness Characteristics of Covid-19 Patients Treated at Selgalu Covid-19 Treatment Center in Assosa, 2021 (210) |
Based on the chi-square test result, a significant difference in the disease severity was found among the different age groups, those with a history of preexisting co-morbid illness; hypertension, and diabetes mellitus. A significantly higher proportion of patients≥ 60 years had a severity of disease (10%, 9%). Similarly, patients with preexisting co-morbid illness significantly had a higher proportion of severe disease (18.6%, 13.3%). Similarly, patients with hypertension (11.35%, 7.7%), diabetes (6.7%, 6.2%) had severe disease.
Symptomatic Characteristics
The majority of the patients admitted at Selgalu 127 (60.5%) had no clinical symptoms 85 (40.5%) among the controls and 42 (20%) cases. Nearly half of symptomatic patients 55 (26.2%) were from of the case comparing 28 (13.3%) of controls (Table 3).
 |
Table 3 Presenting Symptom-Related Characteristics Among Patients Treated at Selgalu Covid-19 Treatment Center in Assosa, 2021 (210) |
Among symptomatic patients, 79 (37.6%) had shortness of breath, 76 (36.2%) fatigue, chills 50 (23.8%), fever 38 (18.1%), chest pain 34 (16.2%), and with small records diarrhea 5(2.4).
Baseline Vital Sign Characteristics Comparison Based on Disease Severity
The majority of patients’ vital sign including body temperature, pulse rate, and blood pressure, was in normal ranges. A significantly higher proportion of severe disease patients with oxygen saturation level less than 90% (33.3)% (severity), Vs 0% (non-severe), p-value=0.000) and respiratory rate 30 and above (30% (severity) Vs 6.7% (non-severe)) had severe disease Similarly, patients with higher blood pressure had severe disease compared with those had no severe disease (Table 4).
 |
Table 4 Baseline Vital Sign Characteristics Among Patients Treated at Selgalu Covid-19 Treatment Center in Assosa, 2021(n=210) |
Factors Associated with COVID-19 Severity
In the uni-variables binary logistic regression analysis, age of admitted patients, signs and symptoms (fever, cough, Shortness of breath, chills, fatigue, sore throat, headache), underlying disease condition (Hypertension, diabetes mellitus), vital sign systolic blood pressure (SBP), diastolic blood pressure (DBP), were found to be significantly associated with COVID-19 severity.
Variables with a P value less than 0.25 in the bivariate analysis were included in the multivariate logistic regression analysis to control the effect of confounding variables. The multivariate logistic analysis identified age groups, fever, fatigue, and hypertension were significantly associated with disease Severity at a 5% level of significance. In this study, patients with 60 and above age groups were about 4 times [AOR:3.85 (1.39–10.64)] and those in 40–59 age groups was more than 5 times higher to the odd of developing the severe disease [AOR:5.30 (2.27–12.34)] compared with other age groups, among patients with symptom the odds of developing Severe COVID-19 disease patients with fever was 4 times higher than[AOR:3.98 (1.59–9.96)] those who did not have such kind of symptoms and patient with history fatigue [AOR:3.14 (1.50–6.54)] was more than 3 times higher than the other symptoms, Likewise, on the preexisting underlying disease, the odds of coming into being severe COVID-19 patients with hypertension was nearly 4 times higher compared to patients with no hypertension history [AOR: 3.68 (1.53–8.82)] (Table 5).
Discussions
COVID19 remains a significant cause of hospitalization and death. This study tried to identify factors associated with COVID19 severity among patients admitted at Selgalu covid19 treatment center Assosa Ethiopia. In multivariate analysis, it was found that four factors remained independently significant association with covid19 severity including age, hypertension, fatigue, and fever.
A Danish Nationwide, Register-based Study showed that males are highly prone to severe disease as well as death than females related to covid19.9 Similar studies done in New York City also associated Male Sex, With COVID-19 Severity and Mortality.10 While another case-control study reveals gene variants Angiotensin-converting enzyme (ACE1, ACE2) are associated with COVID19 severity11 due to the fact that higher level of serum ACE2 activity compared to women. On the other hand, the raised level of immunoglobulin G in women is advantageous to reduce disease severity.12 However, in other studies while men and women have the same prevalence, men with COVID-19 are more at risk for worse outcomes and death.13 On the contrary the other study does not show gender differences regarding disease severity.14 This study also did not show a significant association on genders of patients, despite nearly to third of this observation were male. It could be due to the small number of cases observed at a treatment center.
Different scholars come to an end that the occurrence of COVID19 severity was linked to an older age.15,16 This study showed that COVID-19 severity was higher among patients with 40–59 age groups and being aged 60 or older than the other age groups category respectively. It is consistent with case-control studies conducted in our country17 and other country. Though nearly half of patients in this study were aged less than 40, a very small number of the case were observed among mentioned age category, This might be because immune systems grow weaker as we age and it is one of many adverse consequences of body ability to defend itself from disease, and being aged therefore often suspected to contribute to disease severity, which makes it more challenging for older adults to fight off disease severity. Older adults and others who are at high risk must be closely followed with priority given moreover caregivers should closely monitor to prevent complications and early recovery.
Different studies report symptoms have been associated with covid19 severity.20,21 The study conducted in our country.22 And Wuhan and shanghai china reveals majority of patients were symptomatic.18,23 This study found a high proportion (60.5%) of patients with no symptoms. In line with similar to a recent retrospective cohort study in northern Ethiopia, with 74% of cases having no clinical symptoms.24 And a similar study conducted in Addis Ababa.25 Though the majority of patients were asymptomatic, in this study fever and fatigue are significantly associated with covid19 severity.
Though Patients with SARS-CoV-2 infection can experience a range of clinical manifestations, from no symptoms to critical illness, Different studies concluded that symptoms such as SOB, chills, fever, myalgia, headache, and fatigue are significantly associated with the occurrence of covid19 disease severity.19,26 And study conducted in United States reveals fever is one of the typical symptoms associated with covid19 patients.27 Also study conducted in south Korea.28 This study indicate that patients with fever were more likely associated with disease severity as compared to other symptoms. In line with the study conducted in our country,22 others country.29,30 Again fatigue also associated with disease severity in this study which is consistent with the study that was conducted in Ethiopia,20 china18 and other countries.31 This indicates patients with symptoms are connected to develop a severe disease than those with no symptoms which is the cause of delayed recovery from the disease.21 Being with symptoms indicate that there is still a higher number of viruses in the patient’s bodies,32 which is similar to this study. Though the exact mechanisms for why some people develop symptoms are not known, it might be being aged and having severe underlying medical conditions decrease the body’s ability to defend disease so that they early show symptoms. Furthermore, it is possible to suggest that people with such symptoms needed to get treatment sooner, additionally fever, fatigue can be used as a pre indication of disease severity and used for necessary follow-up and care.
Among comorbidities, hypertension was the most frequent followed by diabetes, cardiac illness, renal disease, and HIV/AIDS despite association being only found among hypertensive patients. The study conducted in Lahore, Pakistan reveals a strong association of COVID-19 severity with the most endangered for the negative result is patients hypertensive and diabetic patients.33 And A prospective cohort study done in this country show that patients without preexisting comorbid illness recovered more quickly than other participants with at least one comorbidity,34 in this study even though diabetes mellitus significant in bivariate analysis, Unlike other studies.7,35 This study did not show a significant association between diabetes mellitus Covid19 severity. Such differences may be attributed to a majority of charts being younger age and predominantly lower prevalence of comorbid conditions.
However different scholars reported having hypertension significantly associated with covid19 severity as indicated in this study. Based on this study Hypertensive patients admitted at Selgalu treatment center had more likely associated with covid19 severity than patients who did not have hypertension history. The study was in line with a retrospective cohort study36 and case-control study.37 This result implies that chronic diseases like hypertension can compromise the immune system, making patients more vulnerable to serious complications. Therefore efficient treatment should be focusing on respiratory difficulties and underlying preexisting medical conditions.
Generally, the findings of the study have paramount implications for the management of COVID19 severity. It would provide helpful insights for program implementers into the potential risk factors of covid19 severity to take priority interventions to prevent Complications due to disease severity.
Finally, The study could not identify other known predictors of COVID-19 because of the small number of observations of severe cases treated at a treatment center. And the study was chart review, as such; poor record-keeping was one of the main challenges. Especially patient’s condition was not being recorded with the standard parameters during their Time at a treatment center. Important Socio demographics like marital status, education, income, and occupational status were not complete.
Conclusions
From this study, we conclude that age groups between 40–59, being aged 60 or older and symptoms like fever, fatigue and underlying comorbid illness hypertension were a significant predictor of COVID-19 disease severity; Despite our limitation of study data highlights the important factors associated with disease severity with covid19 admitted to Selgalu treatment center. Efficient treatment should be given for young adults and older age patients by focusing on respiratory difficulties and underlying preexisting medical conditions. Additionally fever, fatigue can be used as a pre indication of disease severity and used for necessary follow-up and care.
Abbreviations
COVID-19, Coronavirus disease 19; SARS-CoV-2, Severe acute respiratory syndrome COVID 19-2; SARI, Severe acute respiratory syndrome; RT-PCR, reverse transcriptase-polymerase chain reaction; BGRS, Benishangul Gumuz regional state; RHB, Regional health bureau; MOH, Ministry of health; EPHI, Ethiopian Public health institute; WHO, World Health Organization; PHEIC, Public health emergency of international concern; PHSM, public health, and social measures; ICU, Intensive care unit; ACE, Angiotensin-converting enzyme; OR, odds ratio; SPSS, Statistical Package for Social Sciences.
Acknowledgments
The authors thank the Selgalu COVID19 treatment center management and staff for their cooperation.
Author Contributions
All authors made a substantial contribution to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. World Health Organization. Coronavirus disease (COVID-19); 2021. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_1.
2. Fadl N, Ali E, Salem TZ. COVID‐19: risk factors associated with infectivity and severity. Scand J Immunol. 2021;93(6):e13039. doi:10.1111/sji.13039
3. Oliveira E, Parikh A, Lopez-Ruiz A, et al. ICU outcomes and survival in patients with severe COVID-19 in the largest health care system in central Florida. PLoS One. 2021;16(3):e0249038. doi:10.1371/journal.pone.0249038
4. COVID-19 outbreak status update press release [press release]. Addis Ababa, Ethiopia. 2021.
5. EPHI. National Public Health Emergency Operation Center (PHEOC), Ethiopia. Addis Ababa: EPHI; 2021.
6. Gallo Marin B, Aghagoli G, Lavine K, et al. Predictors of COVID‐19 severity: a literature review. Rev Med Virol. 2021;31(1):1–10. doi:10.1002/rmv.2146
7. Leulseged TW, Maru EH, Hassen IS, et al. Predictors of death in severe COVID-19 patients at millennium COVID-19 care center in Ethiopia: a case-control study. Pan African Med J. 2021;38:351.
8. World Health Organization. Clinical Management of COVID-19: Living Guidance. World Health Organization; 2021.
9. Kragholm K, Andersen MP, Gerds TA, et al. Association between male sex and outcomes of coronavirus disease 2019 (COVID-19)—A Danish Nationwide, register-based study. Clin Infect Dis. 2020;73:e4025–4030.
10. Rapp JL, Lieberman-Cribbin W, Tuminello S, Taioli E. Male sex, severe obesity, older age, and chronic kidney disease are associated with COVID-19 severity and mortality in New York City. Chest. 2021;159(1):112. doi:10.1016/j.chest.2020.08.2065
11. Gómez J, Albaiceta GM, García-Clemente M, et al. Angiotensin-converting enzyme (ACE1, ACE2) gene variants are associated with COVID19 severity depending on the hypertension status. MedRxiv. 2020;762:145102.
12. Zeng F, Dai C, Cai P, et al. A comparison study of SARS‐CoV‐2 IgG antibody between male and female COVID‐19 patients: a possible reason underlying different outcome between sex. J Med Virol. 2020;92(10):2050–2054. doi:10.1002/jmv.25989
13. Jin J-M, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi:10.3389/fpubh.2020.00152
14. Mukherjee S, Pahan K, Cavalli G, Ciceri F, Dagna L, Rovere-Querini P. Is COVID-19 gender-sensitive? J Neuroimmune Pharmacol. 2021;16:1–10. doi:10.1007/s11481-020-09966-z
15. Zhang G, Hu C, Luo L, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi:10.1016/j.jcv.2020.104364
16. Tahtasakal CA, Oncul A, Sevgi DY, et al. Could we predict the prognosis of the COVID‐19 disease? J Med Virol. 2021;93(4):2420–2430. doi:10.1002/jmv.26751
17. Leulseged TW, Abebe KG, Hassen IS, et al.COVID-19 disease severity and determinants among Ethiopian patients: a study of the millennium COVID-19 care center. medRxiv. 2020;1(1):e0262896.
18. Yang R, Gui X, Xiong Y. Comparison of clinical characteristics of patients with asymptomatic vs symptomatic coronavirus disease 2019 in Wuhan, China. JAMA Netw Open. 2020;3(5):e2010182–e. doi:10.1001/jamanetworkopen.2020.10182
19. Barek MA, Aziz MA, Islam MS. Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: a meta-analysis with 55 studies and 10014 cases. Heliyon. 2020;6(12):e05684. doi:10.1016/j.heliyon.2020.e05684
20. Abdela SG, Abegaz SH, Demsiss W, Tamirat KS, van Henten S, van Griensven J. Clinical profile and treatment of COVID-19 patients: experiences from an Ethiopian treatment center. Am J Trop Med Hyg. 2021;104(2):532. doi:10.4269/ajtmh.20-1356
21. Leulseged TW, Alemahu DG, Hassen IS, et al. Determinants of developing symptomatic disease in Ethiopian COVID-19 patients. medRxiv. 2020 doi:10.1101/2020.10.09.20209734.
22. Leulseged TW, Hassen IS, Maru EH, et al. Characteristics and outcome profile of hospitalized African COVID-19 patients: the Ethiopian context. medRxiv. 2020;16:e0259454.
23. Mei X, Zhang Y, Zhu H, et al. Observations about symptomatic and asymptomatic infections of 494 patients with COVID-19 in Shanghai, China. Am J Infect Control. 2020;48(9):1045–1050. doi:10.1016/j.ajic.2020.06.221
24. Abraha HE, Gessesse Z, Gebrecherkos T, et al. Clinical features and risk factors associated with morbidity and mortality among patients with COVID-19 in northern Ethiopia. Int J Infect Dis. 2021;105:776–783. doi:10.1016/j.ijid.2021.03.037
25. Seid G, Seid H, Wondmagegn D, et al. Clinical Profile and Treatment of COVID-19 Patients: Experiences from an Ethiopian Treatment Center. The American Society of Tropical Medicine and Hygiene; 2021.
26. Shikha Garg M, Lindsay kim M, Michael Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with laboratory-confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020. US Department of Health and Human Services/Centers for Disease Control and Prevention; 2020. Report No.: No. 15.
27. Burke RM, Killerby ME, Newton S, et al. Symptom profiles of a convenience sample of patients with COVID-19—United States, January–April 2020. Morbid Mortal Wkly Rep. 2020;69(28):904. doi:10.15585/mmwr.mm6928a2
28. Chang MC, Park Y-K, Kim B-O, Park D. Risk factors for disease progression in COVID-19 patients. BMC Infect Dis. 2020;20(1):1–6. doi:10.1186/s12879-020-05144-x
29. Tian W, Jiang W, Yao J, et al. Predictors of mortality in hospitalized COVID‐19 patients: a systematic review and meta‐analysis. J Med Virol. 2020;92(10):1875–1883. doi:10.1002/jmv.26050
30. Wolff D, Nee S, Hickey NS, Marschollek M. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection. 2021;49(1):15–28. doi:10.1007/s15010-020-01509-1
31. Carfì A, Bernabei R, Landi F; Group ftGAC-P-ACS. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–605. doi:10.1001/jama.2020.12603
32. Leulseged TW, Hassen IS, Maru EH, et al. Determinants of time to convalescence among COVID-19 patients at millennium COVID19 care center in Ethiopia: a prospective cohort study. medRxiv. 2020. doi:10.1101/2020.10.07.20208413
33. Shoaib N, Noureen N, Munir R, et al. COVID-19 severity: studying the clinical and demographic risk factors for adverse outcomes. PLoS One. 2021;16(8):e0255999. doi:10.1371/journal.pone.0255999
34. Abrahim SA, Tessema M, Defar A, et al. Time to recovery and its predictors among adults hospitalized with COVID-19: a prospective cohort study in Ethiopia. PLoS One. 2020;15(12):e0244269. doi:10.1371/journal.pone.0244269
35. Sultan M, Kene D, Waganew W, et al. Clinical characteristics of COVID-19 related deaths in Ethiopia. Ethiop J Health Sci. 2021;31(2):223–228.
36. Xiong T-Y, Huang F-Y, Liu Q, et al. Hypertension is a risk factor for adverse outcomes in patients with coronavirus disease 2019: a cohort study. Ann Med. 2020;52(7):361–366. doi:10.1080/07853890.2020.1802059
37. Bhargava A, Fukushima EA, Levine M, et al. Predictors for severe COVID-19 infection. Clin Infect Dis. 2020;71(8):1962–1968. doi:10.1093/cid/ciaa674
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.