Back to Journals » Risk Management and Healthcare Policy » Volume 15
Factors Affecting Utilization of the E-Health “Seha” Interactive Application for Online Medical Consultation in Saudi Arabia
Authors Al-Kahtani NK , Aljabri D , Alrawiai S , Alsubaie S, Alasmari M, Aldukhi Z , Alkahtani HK
Received 15 November 2021
Accepted for publication 11 August 2022
Published 29 August 2022 Volume 2022:15 Pages 1607—1619
DOI https://doi.org/10.2147/RMHP.S349548
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Kent Rondeau
Nouf Khalid Al-Kahtani,1 Duaa Aljabri,1 Sumaiah Alrawiai,1 Shayma Alsubaie,1 Maram Alasmari,1 Zahra Aldukhi,1 Hend Khalid Alkahtani2
1Health Information Management and Technology, College of Public Health, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2Department of Information Systems, College of Computer and Information Science, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Correspondence: Nouf Khalid Al-Kahtani, Department of Health Information Management and Technology, College of Public Health, Imam Abdulrahman Bin Faisal University, Dammam, 31441, Saudi Arabia, Email [email protected]
Purpose: Telehealth, Internet interventions, or digital apps provide healthcare to isolated regions and can span borders. The purpose of this research was to assess the use of the Seha application, public perceptions toward the application, and factors that affect its utilization.
Methods: The cross-sectional method was used to analyze the quantitative data. Grounded Theory was used to analyze the qualitative data. This study was conducted from December 1, 2018, to January 31, 2019. A total of 419 participants were surveyed online, and semi-structured interviews were conducted for 20 participants. The participants were chosen based on convenience sampling techniques. The survey contained two sections. The first section consisted of demographic data and the second section included eight questions, each covering one main aspect. For the qualitative approach, participants were chosen using a theoretical sampling technique. Researchers acted as the primary data collection instrument.
Results: Out of the total, 88.5% of the participants did not use “Seha” application. Among users, the main perceived benefit from the application was the ability to contact a general practitioner anytime. Among non-users, the greatest barrier to use was the lack of awareness about it, while the ability to contact a general practitioner any time (25%) and reducing visits to the doctor (23%) were the top motivations. A conceptual framework was developed to define the different aspects affecting the use of the online medical consultation application. These aspects included awareness and education, technical issues, access, and consultation information.
Conclusion: Public awareness and education about the application, as well as the integration of its functions with other healthcare systems were the main recommendations suggested. Implementing these recommendations is encouraged to deliver value to e-health initiatives in Saudi Arabia.
Keywords: health care, telemedicine, mobile application, digital health, e-health
Introduction
E-health is increasingly becoming an area of interest for the interchange of medical informatics, patient and professional health-related education, public health, and business.1 E-health refers to the delivery of healthcare services and information electronically through a variety of technologies and Internet networks. Internationally, the use of e-health as an alternative to face-to-face consultations in a primary care setting has increased the quality of care.2 Currently, e-health consultation applications via email, videos, and online sites are being investigated as potential methods to improve patient access to healthcare services and save time for healthcare providers.3
In Saudi Arabia, The Ministry of Health (MoH) recently developed telemedicine services.4 Telemedicine can be defined as medicine in which the caregiver uses technology, such as a computer or a satellite, to provide care to patients remotely.5
The MoH developed a new e-health consultation application called “Seha” in 2018 to improve access to medical services, decrease medical expenses, and facilitate citizen satisfaction.6 Seha is a telemedicine service that allows citizens to communicate with healthcare providers remotely and at all times. Users have access to free medical conversations with healthcare specialists using online chat, voice, or video. E-health consultation applications can be an effective tool in healthcare delivery. The utilization of e-health increased significantly during the Covid-19 pandemic. Wind et al7 considered Covid-19 to be the turning point for e-health care, especially for the provision of online mental health care. However, the major barrier toward e-health has been identified as the healthcare professionals themselves, which prevents its utilization in routine practice.8 Despite research showing that a face-to-face meeting is not necessary for establishing therapeutic alliance, the myths surrounding telehealth show the opposite perception.9 According to studies, the adoption of telehealth has been slower than expected, when comparing it to estimates suggesting it takes around 16 years for implementation of any health care innovation.10 As another barrier to e-healthcare, current healthcare systems in most countries are not mature or fully developed, and therefore, lack the degree of integrity, confidentiality, user trust and privacy needed for the gross implementation of e-healthcare.11 Other barriers to the e-healthcare enterprise are the trust of patient over that enterprise and the healthcare services provided to them.12 Furthermore, intertwined with trust are the issues of data management, identity, authenticity, accountability, integrity, and confidentiality.11
In the last two decades, there have been many previous splendid but almost failed attempts to promote e-health in routine practice;13 however, the first year of the Covid-19 pandemic provided a great catalyst in this domain. The outbreak of Covid-19 in Saudi Arabia and other countries worldwide put unprecedented pressure on clinicians, information communication technology staff, and managers to overcome the barriers for acquisition of rapid e-health services.14 This is mainly because predictions regarding Covid-19 are yet largely unclear, and a long-term resolution of this issue in providing care to the heterogenous population of patients, among those that are isolated in hospitals, are in quarantine at home or are still actively working in the community is needed.15 Telehealth, Internet interventions or digital apps can be very helpful in providing healthcare to isolated regions and across borders.
A review of the literature demonstrated that there are different factors affecting the use of e-health consultation applications. The major gap identified via the literature review was that no previous studies have investigated the use of Seha in Saudi Arabia. Rather, all the previous studies identified the benefits, drawbacks, and barriers of e-health consultation applications in general or in countries other than Saudi Arabia. In addition, no studies have investigated the use of Seha application using a grounded theory approach.
In Saudi Arabia, the use of technology in the delivery of health care is expanding, but it remains low. Inadequate infrastructure; ignorance of the usefulness of these technologies; a scarcity of specialists; and a lack of an information management strategy, a national plan for medical data exchange, and a national regulator were identified as key roadblocks.16 A study’s conclusions underlined the relevance of telemedicine and contemporary applications employed throughout the outbreak. The data also revealed how telemedicine and e-Health may be utilized to improve clinical services. Policies adopted throughout the world to improve Covid-19 management have also been examined. Because telemedicine and e-Health are easy, safe, scalable, effective, and environmentally friendly, they may be utilized to deliver clinical care in times of health crisis.17 A questionnaire-based survey of 720 patients from diverse Saudi Arabian areas who visited outpatient telemedicine clinics found that half of the participants were extremely happy, with technological issues being the most prevalent disadvantage noted by patients. Concerned authorities, according to the study, must adopt focused action plans to alleviate the disadvantages patients experience when utilizing telemedicine.18
This study is significant because it provides valuable information regarding the potential factors affecting the utilization of Seha. Application developers and strategic planners can benefit from the findings of this study to improve Seha and other e-health consultation applications worldwide by meeting the users’ needs and promoting the adoption and usage of such applications.
Research Questions
Q1: To what extent is the Seha e-health application being used by Saudi individuals?
Q2: What are the factors affecting the utilization of this app?
Q3: What steps are being taken to enhance its usage?
Materials and Methods
A cross-sectional survey was conducted to study how and under what conditions individuals in Saudi Arabia utilize the Seha e-health application, as well as their attitudes regarding its use using a mixed technique approach. The study was conducted in the eastern region of Saudi Arabia from December 1, 2018, to January 31, 2019. In total, 419 participants were selected based on convenience sampling from all citizens who completed the online survey, and 20 participants recruited for interviews from the survey cohort. The participants comprised different genders and ages and had varying educational qualifications and social statuses. Some had chronic diseases, while others did not.
Quantitative data were collected using modified survey forms from previous studies (Cronbach’s alpha = 0.89). The survey contained two sections. The first section consisted of demographic data, such as gender, age, education level, etc., and the second section included eight questions, each covering one main aspect. Descriptive statistical analysis of the survey data was performed using IBM SPSS Statistics 25.0.
For the qualitative approach, researchers acted as the primary data collection instrument by conducting semi-structured interviews with 20 participants. The participants were chosen based on theoretical sampling techniques from the general Saudi population, which included both users and non-users, males and females, with differing age groups and education levels. Data collection ended when saturation was reached, which is the point where no new information emerged.
The interview was conducted individually and lasted between 10 minutes to 15 minutes. The following three questions guided the interviews: How and under what circumstances do people in Saudi Arabia use the Seha mobile application for medical consultation? What are the perceptions of the people in Saudi Arabia toward Seha? What barriers are most likely to keep them from using Seha?
Grounded theory analysis was performed. Data analysis was conducted in tandem with the data collection. The analysis included systematic reading, organizing, coding, and arranging of interview transcripts to discover the patterns or repetitive ideas and perceptions toward the Seha application from the participants’ responses. The researchers read the interview notes and identified potential categories in the data. Then, based on the categories that emerged, the researchers compared the interview data and analyzed the relationships among them. Finally, based on the analysis, the researchers built a theoretical model, which was continually refined based on the results. Data were reported in the descriptive narrative form to be more understandable and valuable.
Participants’ consent to participate in the study was secured through completed consent forms approved by the institutional review board (IRB) board committee in Imam Abdulrahman bin Faisal University. For participants under the age of 18, their consent to participate was obtained from their parents or guardians. The study was reviewed and approved by the IRB committee in Imam Abdulrahman bin Faisal University (IRB-UGS-2018-03-283) and complies with the Declaration of Helsinki.
Results
Quantitative Approach
Figure 1 shows that out of the total sample (n = 419), only 48 (11.46%) participants had experience with the Seha application. Table 1 shows that most participants were married (56.7%), female (84.5%), between the ages of 25 to 59 years (53%), had a high education level (74.0%), and were from the eastern region (82.6%). Most of the respondents did not suffer from chronic disease (81.1%), with approximately half of them being infrequent visitors of general practitioners (GPs) (52.9%). Participants who did not respond to question one regarding the status of their Seha usage were excluded.
 |
Table 1 Characteristics of Users and Non-Users |
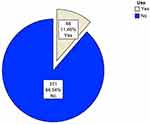 |
Figure 1 Usage of the Seha application. |
Figure 2 shows the possible barriers to the use of the Seha application among non-users (n = 371). Being unaware of the Seha application’s existence (65.77%) was the most prominent barrier, followed by preference to visit the doctor (7.55%), and inadequate knowledge of the Internet (7.55%). Few non-users considered privacy (4.04%), reliability of information (6.20%), the lack of opportunity to use the application (2.70%) to be additional barriers.
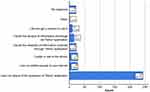 |
Figure 2 Barriers to using the “Seha” application. |
Figure 3 represents the possible means to make participants (n = 48) aware of the Seha application. The ones reported to be most favorable were social media (29.17%), Internet search (16.67%), and other patients or family members (16.67%).
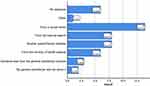 |
Figure 3 Means that helped users know about the Seha application. |
Figure 4 presents reported motivations to use Seha. Ability to contact GPs at any time (25.00%) and reducing visits to the doctor (22.92%) were top motivations. Asking for medication use (16.67%), ability to ask questions that might arise after visiting the doctor (14.58%), asking for a second opinion (10.42%), saving traveling time (6.25%), and asking about the cost and payment of treatment (4.17%) were other motivating factors.
 |
Figure 4 Motivation to use the Seha application. |
Figure 5 presents possible suggestions of information that can be provided through the Seha application regarding the user’s health condition. These include advice on how to resolve a problem without help (31.25%), visit a GP (22.92%), pick up a prescription from a pharmacy (18.75%), and go to the emergency department (16.67%). Approximately 8.33% of users were not contacted.
 |
Figure 5 Type of doctor’s advice. |
The users were asked their opinion regarding the Seha application’s ease of use by means of agreement or disagreement with the statement provided (the Seha application was easy to use). Most users neither agreed nor disagreed (29.17%), as shown in Figure 6. For the remaining users, 25.00% strongly agreed, 16.67% strongly disagreed, 14.58% agreed, and 10.42% disagreed with the statement. The comparison of users and non-user groups on the use of the Seha application were focused on parameters of age, gender, marital status, having children, education level, region, chronic disease, and frequency of visiting GPs.
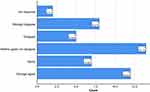 |
Figure 6 Users’ opinions on the Seha application. |
As shown in Table 2, most of the users were married females with children, who were between 25 and more than 59 years old with a high education level, lived in the eastern region, did not suffer from chronic disease, and frequently visited GPs. While most of the non-users were married female, who did not have children, above 25 years of age, with a high education level, lived in the eastern region, did not suffer from chronic disease, and were infrequent in visiting GPs.
 |
Table 2 Comparison of User and Non-User Groups |
Qualitative Approach
Circumstance for Using the Seha Application
The participants were asked about the status of their Seha interactive application for medical consultation usage. Analysis of the interview data showed that only six people reported that they used the application. Some examples of the responses obtained from these users include the following:
“Yes, I use the application.”
“Oh, yes I used it more than one time.”
Most of the interview participants were non-users (n= 14); eleven of them had heard about the application, while three had not. The following are examples of their responses:
“First time I hear about it.”
“I don’t use the phone.”
Data derived from the interviews suggested that different means helped users to know of the Seha application. For example, four of the interviewees reported that they heard about the application from social media. One heard about it from one of his family members and one from an Internet search. The following are examples of participant answers:
“I heard about it from Twitter.”
“Amm, I saw a video about Seha on Instagram.”
“Yes, I heard about it from my cousin.”
“I saw advertisement about Seha on a website.”
Analysis of the interview data revealed that there were different types of consultations provided to them when they used Seha. Three users were advised to visit the doctor; for example, one participant said:
“He advised me to go to the doctor because he would better diagnose my condition and prescribed a medication for me to buy from the pharmacy.”
Another user mentioned that he learned how to use the treatment; for example, he said:
“I had allergy of a treatment I used so I was taught a better way to use the medicine.”
Another user said she received instructions on how to relieve her pain. The following is an example:
“I used it when I was pregnant, and I had severe pain in the middle of the back. So, the doctor told me not to carry heavy things and to rest more.”
Perception Toward the Seha Application
The participants were asked about their perception of the Seha application. Data derived from the interview showed that participants observed some benefits that motivated them to use the Seha application, while others mentioned drawbacks that prevented them from using it.
Motivation to Use the E-Health “Seha” Application
Analysis of the interview data revealed many reasons motivate participants to use the Seha application. Two respondents reported that they used the application because it saved time and the effort of going to the hospital, including reducing the waiting time in hospitals. In addition, one respondent reported that access to the consultation service was very quick and easy, and one reported that the consultation service provides easier and better patient–physician communication. Moreover, one interviewee reported that avoiding visits to the doctor felt better and was more convenient. Another reported that he used the application because he wanted a second opinion from accredited and professional doctors. The following are examples of the participants’ answers:
“I’m a busy employee so, I using the application because I don’t have time to go to a hospital and the hospital is far away from my workplace.”
“Oh, it is an interesting application, it is solves waiting time problem in hospital.”
“When I want medical advice, it is very easy and quick to obtain advice by using Seha application.”
“It was easy and it was very easy because even my child can use it.”
“In my opinion, by using this application it is made easy to communicate with a doctor.”
“Honestly, I don’t like to see a doctor face to face and I feel uncomfortable.”
“I use the application because sometimes after a visit a doctor, I need second opinion and from a good doctor.”
Drawbacks to Using the Seha Application
Data from the interviews revealed that there are some drawbacks to the use of Seha. Four users of Seha had encountered problems, and two had not. One user said that the services were fast but without value. Another mentioned that the patient cannot depend on this application. Two users stated that the problems lie in the weak or absent communication, shortage of care providers, inaccurate diagnosis, and unsuitable treatments. The following are some examples of the respondent’s answers:
“The speed of the reply but it was useless.”
“They did not answer me.”
The patient cannot rely entirely on this application and cannot dispense with the doctor in specialized or general clinics, because the doctor in the clinics is looking for the patient’s case intensively and diagnose the patient correctly and give him the necessary treatment for his condition after analysis and clinical diagnosis.
There are many negatives. First, the numbers of consultations are three a month only. Second, the doctor takes a long time to respond, and with each new consultation the doctor is changed rather to have the same doctor from the first consultation so he can understand my health status.
Barriers to Using the Seha Application
Participants were also asked about barriers that prevent them from using the Seha application. Data from the interview showed that there were some barriers hindering the usage of the Seha application, such as a low response rate or no response to their calls (n = 2). The following are some examples of participants’ words:
“I downloaded but I tried to chat with the doctor, but no answer by a doctor.”
“I sent my medical problem but no response by a doctor.”
Furthermore, there seems to be a lack of awareness regarding the Seha application or its implementation (n = 5). One interviewee did not know how to use the mobile phone, and two stated that they prefer face-to-face visits. Two interviewees reported that no valuable information would be gained due to the fact that the medicine is evidence-based; thus, physical examination and investigation are needed to obtain useful information. Two interviewees did not get a chance to use the application. The following are examples of participants’ answers:
“I heard about this application, but I didn’t know it was implemented.”
“’Seha’ what is that!!”
“Sorry I don’t know how to use the phone.”
“I like to go to primary care center.”
“The doctor said to me ‘you should go to the hospital’ without giving any principal diagnosis.”
“I don’t use this application because the right diagnosis and right treatment need physical examination and lab tests.”
E-Health “Seha” Interactive Application Utilization for Online Medical Consultation as a Theoretical Abstraction
The study’s data was used to create a conceptual framework that revolves around the main variables that must be addressed for improved use of the e-health Seha interactive application. Figure 7 depicts the connection with several relevant factors abstracted. The goal of this abstraction is to detect and manage the effect of various domains. This abstraction can help policymakers and strategic planners discover places where they should invest or focus their efforts. It demonstrates a clear link between the data and criteria examined and the degree of Seha use for online medical consultations. Directional arrows are used to show these relationships. The following are the spectra of levels that can influence a policymaker’s decisions:
 |
Figure 7 Conceptual framework of different factors affecting “Seha” use. |
Awareness and Education Factors
The use of e-health medical consultations would be influenced by public awareness. People’s awareness of e-health medical consultations and associated services would boost their use of them. People who are educated about Seha’s features and the e-health medical consultation option would be more likely to use the app.
Technical Factors
Integrating the app with other e-health and medical apps would boost the number of people who utilize e-health medical consultations. Furthermore, combining e-health and medical consultation apps with a patient’s electronic health record at a hospital or primary care facility would expand the usage of e-health medical consultation.
Access Factors
Providing convenient, quick, and free access to e-health medical consultations would encourage more people to utilize the app. Allowing users unrestricted access to various sorts of medical consultation services from expert physicians would encourage more individuals to use the app.
Consultation Information Factors
People will use the Seha application for medical consultations if they believe they have been accurately diagnosed, and if the consultation material supplied to them is accurate and has resulted in a thorough understanding of their issue rather than a superficial diagnosis. Moreover, people would use the Seha application for medical consultation if the privacy and confidentiality of their information are protected.
Discussion
The present study investigated factors affecting the utilization of the Seha application in Saudi Arabia. A large sample of survey data combined with participant interview data allowed comprehensive insight into the Seha application. However, because the study was launched in the eastern region of the Kingdom of Saudi Arabia (KSA), most of the participants were from the eastern region, and therefore further studies should be conducted in other parts of Saudi Arabia.
MoH has launched a number of telemedicine initiatives to increase the quality of healthcare for all citizens, and one of these initiatives was the Seha application. The goal of this study was to identify factors affecting the utilization of Seha in Saudi Arabia. Barriers to the use of Seha among non-users as well as the benefits and drawbacks of using the application were investigated.
The study results showed that most of the study population (88.54%) had no experience with Seha. The most common barriers to the use of Seha were being unaware of its existence and participant preference of visiting the doctor. These are comparable to the findings of a study by Nijland et al19 on the barriers preventing the use of online consultation applications, wherein patients ignorance of the existence of these types of services was a primary barrier. Nijland et al19 also found that specific patient groups, such as those less educated, elderly, and chronic medicine users, were particularly eager to use e-consultation, but also saw several impediments to doing so. For example, older patients felt a greater lack of Internet abilities than younger patients, and less educated patients were less aware of the availability of e-consultation than more educated patients. Educating citizens on the benefit of the Seha application and promoting it could remove these barriers.
The study also investigated the benefits of Seha by asking users for their feedback, the type of advice provided through the application, and the ease of use. The benefits included being easy to use, the ability to contact doctors anytime, the reduced number of appointments, the ability to ask for medication, the ability to ask questions that might arise after visiting the doctor, seeking a second opinion, saving travel time, the ability to ask about the cost of treatment, and finally reducing the doctor’s workload by guiding the patients on whether to visit a GP, go to the emergency department, or handle their health problems by themselves. Comparisons of this study’s results with those of previous studies regarding online medical consultation indicated that online medical consultation has benefits. Some studies agreed that e-consultation provides benefits to users as well as to healthcare providers by giving the patient the ability to contact doctors anytime, reducing the physician workload, and allowing patients to seek a second opinion.19,20 In addition, researchers considered the ability to ask follow up questions after visiting the doctor and asking for medication to be benefits of e-consultation applications.19 According to the study results, participants had no experience with the Seha application. The most prominent barrier preventing the use of the Seha application was potential users being unaware of its existence. The application has many benefits for users. The most prominent benefits were the ability to contact doctors anytime and the minimization of visits to the doctor.
On the other hand, users of the Seha application reported some drawbacks. One reported drawback was that while the service was fast, it had no value to the user. In addition, the application was not reliable, as it could not dispense with face-to-face doctor consultations, and sometimes the GPs did not provide a principal diagnosis and directed the patients to visit the doctor. The number of GPs was small compared to the number of consultations, leading to a slow response from doctors to consultants. Furthermore, the GPs prescribed medications without a formal prescription, and only three consultations were allowed per month, which is a very low number. Some participants reported that the GPs took a long time to respond and sometimes did not respond at all. Furthermore, the GPs changed for each consultation rather than being standardized to enable them to have an in-depth understanding of the patient’s health status. Researchers also considered e-health applications to be quick tools for medical consultations that lead to a superficial understanding of the patient’s condition.21 Other studies also found similar barriers to e-healthcare, such as degree of integrity, confidentiality, user trust and privacy, data management, identity, authenticity, accountability etc.10–12
Our findings imply that, despite their increased use of e-health, individuals still need to talk to their physicians about their concerns about their condition. Furthermore, patients’ satisfaction with the Internet was connected to their reliance on e-health in this study, but not with their contentment with the services given by health care professionals. This might reflect people’s sustained confidence in the health care system. As a result, health care professionals must ensure that their patients have access to remote treatment and consultation. This will pave the way for the use of telemedicine. Telemedicine has evolved over the previous several decades to increase accessibility and quality of treatment for patients and health care practitioners, as well as to address health care access issues, particularly during the Covid-19 pandemic.
Conclusion
The MoH in Saudi Arabia launched the Seha application to increase the quality of healthcare services. This study investigated the factors affecting the usage of the Seha application by assessing the benefits, drawbacks, and barriers to its usage as well as providing recommendations that can enhance the Seha application for its users. However, the relevant authorities must develop appropriate and specific action plans to address the perceived drawbacks of telemedicine among patients. Multicenter exploratory research comparing the virtual outpatient clinic to existing telemedicine services provided by the MoH, KSA is also required.
Study Limitation
The main limitation of this study is its use of a cross-sectional study design and convenient sampling technique, which will limit the generalization of its results to all Saudi patients. However, because the study was launched in the eastern region of the KSA, most of the participants were from the eastern region, and therefore further studies can be conducted on other parts of Saudi Arabia.
Study Recommendations
The study resulted in several recommendations to enhance the use of the Seha application. The application should be promoted through the MoH website, advertisements in social media, and waiting room banners. Users should be educated on how to use the application and its benefits. There must be strong policies to ensure the confidentiality, privacy, and rights of the patient. The application should be integrated with the patient’s electronic health record or information with the primary care provider to ensure a consultation from a doctor who knows the user’s history. Connecting the application to hospitals will allow the user to follow up with their doctor after completing the application. The Seha application should be integrated with other MoH systems and applications, such as the Mawid application, which allows users to schedule appointments with medical professionals. Users should be able to obtain e-consultations at any time through the Seha application, regardless of their location. It is necessary to enable faster and more convenient access to the Seha application, and access to the application should be permitted through a website.
Data Sharing Statement
The data for this study are highly confidential and cannot be shared.
Acknowledgments
We are very thankful to all the associated personnel in any reference that contributed in/for the purpose of this research. We would also like to thank Enago (www.enago.com) for the English language review.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dang S, Golden AG, Cheung HS, Roos BA. Telemedicine applications in geriatrics. In: Brocklehurst’s Textbook of Geriatric. Gerontology and Geriatric Medicine. Elsevier Ltd; 2010:1064–1069.
2. Atherton H, Ziebland S. What do we need to consider when planning, implementing and researching the use of ernatives to face-to-face consultations in primary healthcare? Digit Health. 2016;2:2055207616675559. doi:10.1177/2055207616675559
3. Edwards HB, Marques E, Hollingworth W, et al. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open. 2017;7:e016901. doi:10.1136/bmjopen-2017-016901
4. National E-health Strategy: E-health. Kingdom of Saudi Arabia: ministry of Health. Available from: https://www.MoH.gov.sa/en/Ministry/nehs/Pages/Ehealth.aspx.
5. Definition of Telemedicine. In: merriam-Webster.com dictionary. Available from: https://wwwmerriam-webster.com/dictionary/telemedicine#:~:text=%3A%20medical%20care%20provided%20remotely%20to,chronic%20medical%20and%20mental%20disorders%20%E2%80%A6%E2%80%94.
6. MOH: e-Health Application Launched. Kingdom of Saudi Arabia: ministry of Health. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2017-12-14-007.aspx.
7. Wind TR, Rijkeboer M, Andersson G, Riper H. The COVID-19 pandemic: the ‘black swan’for mental health care and a turning point for e-health. Internet Interv. 2020;20:100317. doi:10.1016/j.invent.2020.100317
8. Topooco N, Riper H, Araya R, et al. Attitudes towards digital treatment for depression: a European stakeholder survey. Internet Interv. 2017;8:1–9. doi:10.1016/j.invent.2017.01.001
9. Berger T. The therapeutic alliance in internet interventions: a narrative review and suggestions for future research. Psychother Res. 2017;27:511–524. doi:10.1080/10503307.2015.1119908
10. Rogers H, Madathil KC, Agnisarman S, et al. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed E Health. 2017;23(9):707–717. doi:10.1089/tmj.2016.0248
11. Sahi MA, Abbas H, Saleem K, et al. Privacy preservation in e-healthcare environments: state of the art and future directions. IEEE Access. 2017;6:464–478. doi:10.1109/ACCESS.2017.2767561
12. Van Velsen L, Tabak M, Hermens H. Measuring patient trust in telemedicine services: development of a survey instrument and its validation for an anticoagulation web-service. Int J Med Inform. 2017;97:52–58. doi:10.1016/j.ijmedinf.2016.09.009
13. Mohr DC, Riper H, Schueller SM. A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry. 2018;75:113–114. doi:10.1001/jamapsychiatry.2017.3838
14. Krausz M, Westenberg JN, Vigo D, Spence RT, Ramsey D. Emergency response to COVID-19 in Canada: platform development and implementation for eHealth in crisis management. JMIR Public Health Surveill. 2020;6:e18995. doi:10.2196/18995
15. Pappot N, Taarnhøj GA, Pappot H. Telemedicine and e-health solutions for COVID-19: patients’ perspective. Telemed E Health. 2020;26:847–849. doi:10.1089/tmj.2020.0099
16. Ahmed NJ. Current practice of using technology in health-care delivery in Saudi Arabia: challenges and solutions. Asian J Pharm. 2021;15. doi:10.22377/ajp.v15i1.3935
17. Bokolo AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Health Technol. 2021;11:359–366. doi:10.1007/s12553-020-00516-4
18. Thirunavukkarasu A, Alotaibi NH, Al-Hazmi AH, et al. Patients’ perceptions and satisfaction with the outpatient telemedicine clinics during COVID-19 era in Saudi Arabia: a cross-sectional study. Healthcare. 2021;9:12. doi:10.3390/healthcare9121739
19. Nijland N, Van Gemert-Pijnen JE, Boer H, Steehouder MF, Seydel ER. Increasing the use of e-consultation in primary care: results of an online survey among non-users of e-consultation. Int J Med Inform. 2009;78:688–703. doi:10.1016/j.ijmedinf.2009.06.002
20. Umefjord G, Petersson G, Hamberg K. Reasons for consulting a doctor on the Internet: web survey of users of an Ask the Doctor service. J Med Internet Res. 2003;5:e26. doi:10.2196/jmir.5.4.e26
21. Nijland N, van Gemert-Pijnen J, Boer H, Steehouder M, Seydel ER. Evaluation of internet-based technology for supporting self-care: problems encountered by patients and caregivers when using self-care applications. J Med Internet Res. 2008;10:e13. doi:10.2196/jmir.957
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
