Back to Journals » International Journal of Women's Health » Volume 15
Factors Affecting the Outcomes of First in vitro Fertilization and Embryo Transfer: A Retrospective Investigation
Authors Muhaidat N , Karam AM , Nabhan MS , Dabbah T, Odeh B, Eid M, Almahallawi NJ , Alshrouf MA
Received 19 July 2023
Accepted for publication 22 September 2023
Published 11 October 2023 Volume 2023:15 Pages 1537—1545
DOI https://doi.org/10.2147/IJWH.S431468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Nadia Muhaidat,1 Abdulrahman M Karam,2 Mohammed Saad Nabhan,1 Tala Dabbah,2 Bilal Odeh,2 Mira Eid,2 Nadia Jamal Almahallawi,3 Mohammad Ali Alshrouf2
1Department of Obstetrics & Gynaecology, School of Medicine, The University of Jordan, Amman, 11942, Jordan; 2The School of Medicine, The University of Jordan, Amman, 11942, Jordan; 3Department of Family Medicine, School of Medicine, The University of Jordan, Amman, 11942, Jordan
Correspondence: Nadia Muhaidat, Department of Obstetrics & Gynaecology, School of Medicine, The University of Jordan, Amman, 11942, Jordan, Tel +962798385775, Email [email protected]
Background: The outcome of embryo transfer (ET) is multifactorial. A variety of patient-related, procedural-related, and operator-related factors are known to play a role. This study aims to evaluate the outcomes of ET and determine the factors that affect the outcome.
Methods: The study involved a retrospective design involving 300 first in vitro fertilization and embryo transfer (IVF-ET) cycles between 2011 and 2021. The outcome included 155 unsuccessful cycles and 145 successful IVF-ET leading to pregnancy. The outcomes were examined for different variables, including age, weight, height, body mass index, cause of infertility, number of embryos fertilized during the cycle, day of ET, whether the embryo was frozen, presence of blood or mucus during the procedure, the use of a stylet, tenaculum, uterine sound/dilator, and catheter type. Logistic regression was used to analyze factors affecting the outcomes of ET.
Results: The mean age was 27.84 ± 3.77 years. Patients who had blood during the procedure (32.9% vs 17.2%, p = 0.002), mucus (31% vs 20.7%, p = 0.049), or used the tenaculum (16.8% vs 6.9%, p = 0.012) were more likely to have unsuccessful IVF-ET. Logistic regression to adjust for related factors revealed that the presence of blood (AOR = 2.21, 95% CI 1.04 to 4.66, p = 0.038) during the ET had a higher likelihood of an unsuccessful outcome.
Conclusion: This study showed that the presence of blood during the ET cycle influenced clinical pregnancy. This highlights the importance of performing the procedure under atraumatic conditions.
Level of Evidence: Level III; retrospective comparative study.
Plain Language Summary: Infertility is considered an important public health problem in terms of high expenses, treatment complications, and failure. Addressing the factors that impact embryo transfer outcomes may help in guiding counseling and management. Therefore, the aim of this study was to evaluate the results of IVF-ET and assess several patient-related and procedural-related factors that impact those results. It included retrospectively 300 cycles from 2011 to 2021. The presence of blood after embryo transfer was shown to be the major predictor of an unsuccessful cycle. Moreover, although the usage of additional instruments was not significantly associated with a higher risk of failed embryo transfer cycles, the operators should use these instruments with caution in order to avoid any trauma that might result in bleeding.
Keywords: IVF, assisted reproductive technique, infertility, pregnancy, predictive factors
Introduction
Infertility is a global public health burden that affects every aspect of human life. It is estimated to affect 15% of reproductive-age couples globally.1 As a response, the use of assisted reproductive technology is becoming more common.2 Regardless of the availability and advancement of infertility treatments, the implantation rate is still relatively low.3 The success of implantation depends on several factors, including a viable embryo, a receptive uterus, and the embryo transfer technique.3 One of the most important yet simplest step of this process is embryo transfer (ET). However, despite its simplicity, ET can adversely affect the outcome if not carried out meticulously.
Recognizing the other factors that influence the outcome of embryo transfer might assist in counseling and guide the management. These factors include the difficulty of embryo transfer, the appearance of blood or mucus, embryo retention, high uterine contraction frequency, the catheter type, catheter loading and placement techniques, ultrasound quality, and operator-related factors.4,5 In order to standardize ET technique, the American Society of Reproductive Medicine (ASRM) guideline recommends using ultrasound guidance and a soft catheter during the procedure, as well as advocates for early ambulation after the procedure.6 However, minimal attention has been paid to the embryo transfer technique, as embryo transfer is sometimes seen as an insignificant contributor to the outcome of an IVF cycle; furthermore, physicians are usually unwilling to update their routines or methods for performing embryo transfer.4
Infertility is perceived as a traumatizing experience as patients are confronted with a wide range of treatment options, indications, complications, failures, and expenses. This is evidenced by worse mental health status levels in couples undergoing IVF-ET compared to fertile couples.7 Therefore, this study attempts to assess the outcome of IVF-ET and to identify the factors that influence those outcomes in a tertiary care hospital. This will benefit infertility care providers and patients, which will aid us in optimizing the outcomes and alleviating their concerns. According to our search, there is a paucity of studies that investigate the factors that impact IVF-ET outcomes, making our study the first in our region to shed light on this topic.
Materials and Methods
This study was a retrospective cohort analysis of 300 IVF cycles performed at single 600-bed tertiary care teaching hospital. It investigated the factors and circumstances surrounding the procedure of embryo transfer that may affect the success of cycles measured by achieving a clinical pregnancy.
Study Aim
This study aimed to analyze factors related to the procedure of embryo transfer in IVF cycles where good quality embryos have been produced and assess their impact on the success of the cycle as measured by achieving a clinical pregnancy.
Study Sample
Out of 1,503 cycles performed from 2011 to 2021, at a tertiary care teaching hospital, 300 cycles were included in this study. The data collection process was carried out manually, using the patient records kept at the IVF unit at the institute. Inclusion criteria were: primary infertility, female partner age of 35 years or less, and a first attempt at fresh or frozen thawed embryo transfers that had at least one grade 1 embryo. The exclusion criteria were: repeat cycles, no grade 1 embryos, women that had previous uterine surgery or manipulation, and women above the age of 35 years. The primary outcome was considered successful if the outcome was a clinical pregnancy.
The resulting embryos are examined and classified to choose the highest quality embryos for the embryo transfer. In our study, we only included cases that had at least one grade 1 embryo in the ET, to ensure that embryo quality had no bearing on the outcome. A grade 1 embryo suggests the highest quality embryo, which is determined by the embryologists, is one in which all of the blastomeres are the same size and there is no cytoplasmic fragmentation in the embryo. All IVF procedures were performed by a professional and experienced IVF specialist with at least ten years of experience in IVF procedures using the same standard protocol. Only grade 1 was included to exclude the quality difference between the cases and to be able to study the other confounding factors without the effect of the embryo quality.
Data Collection
Of 1,503 total patient files, 300 patients were included in our study (supplementary material). The data collection process was carried out manually, using the physical records kept at the IVF unit. The cases were chosen using predetermined inclusion and exclusion criteria; all of the cases included had primary fertility issues and a maternal age of less than 35. Both fresh and frozen thawed embryo transfers were included if they had at least one grade 1 embryo, granting it was the first attempt. Any cases where the woman had had previous uterine surgery or manipulation were excluded. Repetitive cycles, cycles with no grade 1 embryos, and cases where data was missing from the records were also excluded.
Ovarian Stimulation
All patients received advice and detailed explanations of the procedure from medical specialists before giving their informed consent to undergo IVF-ET. Patients underwent controlled ovarian hyperstimulation (duration ranged from 9 to 12 days depending on the response to stimulation) with either gonadotropin-releasing hormone (GnRH) agonist (0.1 mg subcutaneously) and with human menopausal gonadotropin (hMG) preparations (150–450 IU intramuscularly) or in some case follicle-stimulating hormone (FSH) (150–450 IU intramuscularly) or, based on patient profile including the age and weight, ovarian reserve, and response to stimulation. Human chorionic gonadotropin (HCG) (10,000 IU intramuscularly) trigger was used to achieve final maturation of the oocytes. IVF specialists used ultrasonography to perform serial monitoring for controlled ovarian stimulation with hormones. Oocyte retrieval was carried out under sedation using ultrasound-guided aspiration of the follicles, 36 h after injection of HCG. Further in-depth details on procedures of both protocols are described in this article.8 A detailed medication plan was presented to each of the patients, and given their strong desire to achieve pregnancy, they were strongly motivated to adhere to the prescribed medication regimen.
ET Technique
Embryo transfers were carried out on days 2–5, all in the same setting by experienced gynecologists. The patient is situated in the lithotomy position and a stepwise approach was implicated based on difficulty. Cervix is exposed using a bivalve speculum. The outer sheath catheter is then inserted into the cervical canal under abdominal ultrasound guidance, ideally without any additional instruments or aids used. In the majority of cases, a curved cook catheter was used. If unable to pass the catheter through the cervical canal due to resistance or excessive angulation, the additional steps to overcome this difficulty were in the following order: use of a stylet; use of tenaculum; use of uterine sound or dilator. Once access through the cervix into the uterine cavity is achieved, the embryos are loaded into the inner catheter and transferred into the uterine cavity through the outer sheath. Following the process of embryo transfer, the catheter and sheath are examined under the microscope to confirm that none of the embryos are retained on the catheter or outer sheath. After the transfer, the catheter and sheath are examined for any mucus or blood, and findings are recorded accordingly.
Statistical Analysis
SPSS version 28.0 (Chicago, IL, USA) was used in our analysis. The continuous data was described using variability analysis in the form of means ± standard deviation. The sociodemographic factors were calculated and provided as frequencies (percentages) using standard descriptive statistical parameters. Fischer’s exact test with OR (95% CI) was used to determine the association between categorical study factors and the outcome of ET. We performed an independent sample t-test to analyze the mean difference between the demographics of patients and the outcome of ET, and we presented data in mean ± standard deviation.
Variables that showed univariate analysis with a p<0.1 were included in the logistic regression model in order to control for possible confounding factors, which were summarized using AOR (95% CI). Statistical significance was defined as a p-value of less than 0.05.
Ethical Considerations
This study was approved by the institutional review board of the institute, as well as the scientific research committee of the medical faculty at University of Jordan (Approval No. 1020229249; 1 March 2022), under the stipulation that no form of identification was to be included at any point throughout the study and the privacy of patients was ensured.
Results
Patients’ Characteristics
The study included 300 women who underwent IVF-ET. The age ranged from 17 to 35 years, with a mean age of 27.84 ± 3.77 years. The mean weight was 70.41 ± 17.51 kg, and the mean height was 159.02 ± 10.78 cm, which is equivalent to a mean BMI of 30.22 ± 32.52. Table 1 demonstrates the patients’ demographics according to the IVF-ET outcome.
 |
Table 1 Demographics of Patients with Unsuccessful and Successful Embryo Transfer |
Factors Affecting Implantation
In total, 51.7% had an unsuccessful cycle and 48.3% had successful IVF-ET and resulted in a clinical pregnancy. The most common causes of seeking infertility treatment included male factors (54.3%), followed by unexplained infertility (18%), and combined factors (7%). Table 2 shows the causes of infertility and the outcome of embryo transfer.
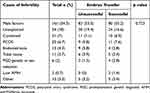 |
Table 2 Causes of Infertility and the Outcome of Embryo Transfer |
The overall mean number of embryos obtained during the cycle was 2.47 ± 0.84 (range, 1 to 6), with no significant mean difference between the unsuccessful and successful groups (p = 0.474). The day of transfer was 2.83 ± 0.56 of the cycle (range, 2 to 5), with no significant mean difference between the unsuccessful and successful groups (p = 0.391). The vast majority (89.3%) of the embryos transferred were fresh embryos, and only 10.7% were frozen embryos.
During the procedure of embryo transfer, in 25.3% of the cases, blood was noticed and in 26.6% of the cases, mucus was found. Most of the cases did not require any instruments to be used. A stylet was used in 15% of the cases, a tenaculum was used in 12%, and uterine sound /dilator was used in 6.3%. The catheter used was a curved cook in 98.7% of the cases, Gyne flex (0.7%), double cook (0.3%), and Labotect catheter (0.3%).
As shown in Table 3, the univariate analysis showed that in the cases where blood was found during the procedure (OR = 2.35, 95% CI 1.36 to 4.06, p = 0.002), the presence of mucus (OR = 1.72, 95% CI 1.02 to 2.91, p = 0.049) or the use of tenaculum (OR = 2.72, 95% CI 1.26 to 5.87, p = 0.012) had a higher likelihood of unsuccessful IVF-ET. There was no significant association between the outcome of ET and whether the embryo was frozen, the use of a stylet, the use of uterine sound/dilator, or the catheter type.
 |
Table 3 Outcome of Embryo Transfer and Related Factors to Unsuccessful Embryo Transfer |
Predictive Factors of Pregnancy Failure After Embryo Transfers
Variables that with a level of significance p < 0.1 from the univariate analysis were included in the regression model in order to control for possible confounding factors, which included the presence of mucus or blood, the use of tenaculum, stylet, or uterine sound/dilator. The only significant predictor for unsuccessful IVF-ET was the presence of blood (AOR = 2.21, 95% CI 1.04 to 4.66, p = 0.038). The presence of mucus, the use of tenaculum, stylet, or uterine sound/dilator were not significant predictors in the regression model. Table 4 shows the regression model results for an unsuccessful IVF-ET prediction.
 |
Table 4 The Results of Regression Model for Embryo Transfer Failure |
Discussion
The aim of this study was to evaluate the procedure of embryo transfer and investigate the factors that influence its outcome at a tertiary care teaching hospital between 2011 and 2021. Our results found that less than half of the participants had successful IVF embryo transfer that resulted in clinical pregnancy. The most common instrument used was the stylet, followed by the tenaculum and uterine sound /dilator. Furthermore, the presence of blood during embryo transfer was associated with higher rates of unsuccessful cycles.
Maternal age is considered a major risk factor for early pregnancy loss.9 This is due to the fact that as females age, their oocyte quality declines.2 This is evident in the substantial loss of mitochondria in the oocytes, which may result in impaired chromosomal meiosis, hence increasing the probability of embryo aneuploidy.10 Several studies have shown that maternal age influences the outcome of embryo transfer.2,11,12 However, in our study, there was no significant association between maternal age and ET outcome. We hypothesize this finding is due to the small sample of our study, as it included 300 cycles only. Moreover, although the mean BMI for successful and unsuccessful embryo transfer groups was 28.78 and 31.54, respectively, it did not reach statistical significance. Similar results were found in different studies, such as in a study conducted by Xu et al on 22,413 IVF cycles.11 However, the effect of obesity on the outcome of assisted reproduction technology cannot be overlooked. High BMI is associated with higher doses of gonadotropins, risk of hyperstimulation syndrome, miscarriage, higher cancellation rates, and lower oocyte recovery.13–15 Furthermore, as shown in our sample, no significant relationship was established between the cause of infertility and ET outcome. One plausible explanation is our inclusion of cases only with 1 embryo grade 1.
The univariate analysis found that the presence of blood, mucus, or the use of tenaculum during the procedure had a higher probability of unsuccessful IVF-ET. When calculating the linear regression analysis to predict the impact of the possible cofounding factors, including the presence of blood, mucus, using tenaculum, stylet, or uterine sound/dilator. We found that the presence of blood during ET is an important predictor of the IVF-ET outcome. One reason behind our finding could be that the presence of blood on the transfer catheter indicates subclinical infection, such as bacterial vaginosis, which causes cervical friability.16 Other causes include traumatic contact with the cervix or the endometrium, resulting in bleeding.17 Our findings supported the results of prior studies.16,18,19 Thus, it is recommended to perform embryo transfer under atraumatic conditions without the presence of blood or mucus to increase the likelihood of implantation.20 However, several studies have shown that there is no relationship between the presence of blood on the transfer catheter and the chances of pregnancy.3,21,22 These conflicting findings may be a result of the lack of universally comparable definitions that permit in-depth comparisons.22
The presence of mucus on the transfer catheter is still a subject of controversy. Several studies have shown that mucus can significantly impact the outcome of assisted reproductive technology (ART) by causing mechanical obstruction of the catheter opening, resulting in embryo retention.17,23–25 In our study, however, the linear regression model showed that there was no significant association between the presence of mucus during embryo transfer and the success of IVF-ET. This observation aligns with what other studies have found.16,26 Moreover, the American Society for Reproductive Medicine (ASRM) has concluded that the appearance of mucus on the transfer catheter is not related to a reduced likelihood of clinical pregnancy or live birth.6 The study involved the transfer of 89.3% fresh embryos, with the remaining 10.7% consisting of frozen embryos. The findings of a recent study indicate that there is no discernible difference in cumulative live birth rates between fresh and frozen transferred embryos.27
It is widely known that the pregnancy rate after embryo transfer primarily relies on the clinical and embryonic characteristics; however, the procedure of embryo transfer should also be taken into account.28 This is supported by the study conducted by Morin et al, who found that the operator performing the transfer has a significant impact on the live birth rate even though embryonic factors are controlled by using euploid blastocyst transfer.29 Furthermore, it was shown that operator experience was not associated with a better outcome.29,30 In our study, the linear regression model demonstrated that use of additional instruments, including stylet, tenaculum, and sound/dilator, did not influence the outcome of ET. Although no significant association was seen, this finding is of paramount importance because it highlights that the procedure of ET is operator dependent. This means that physicians who are skilled and familiar with the use of these instruments and can perform the procedure under atraumatic conditions without bleeding, hence having a better chance of success with ET. Further studies are required to confirm this plausible explanation. It is important to consider non-invasive prenatal diagnosis (NIPT) during the first trimester of pregnancy. In a narrative review, NIPT was found to be a valuable tool for screening or even diagnosing chromosomal and monogenic diseases, reducing the need for invasive procedures.31 Moreover, a recent study has posited that the prospective integration of artificial intelligence into assisted reproduction technology processes might potentially serve as a valuable instrument for prognosticating the clinical outcome, utilizing known parameters, and facilitating the strategic formulation of treatment modalities for individuals experiencing infertility.32
The authors acknowledge that this study is not without limitations. First, our study is limited by its single-center retrospective design. Moreover, our sample size is relatively small compared to prior studies.3,16 This is due to the fact that there were many missing files which were excluded and during the first two years of the COVID-19 pandemic there where suspension of reproductive treatment and various degrees of lockdown and medical resource redistribution resulted in restricted access to and availability of such services in Jordan.33 Another limitation is the lack of universal definitions and standardized protocols that allow for reliable comparisons between studies in different institutions.22 However, we believe that our study demonstrated significant findings that will provide a reference basis for further large-scale multi-center prospective studies in order to deepen our understanding of how different factors can influence the procedure of IVF-ET. In addition, we recommend future studies to consider endometrial thickness which is often used as an ultrasonic marker for receptivity.
Conclusion
Our study provides preliminary evidence that the presence of blood after embryo transfer is a significant predictor for unsuccessful cycle. In addition, using additional instruments was not associated with an increased risk of a negative outcome of embryo transfer. However, we hypothesize this finding is due to the procedure of embryo transfer being operator dependent. Therefore, this study suggests that performing the procedure in an atraumatic setting without resulting in bleeding is crucial. We anticipate that our study may help infertility care professionals who are coping with similar challenges to improve care provision and clinical results for these patients.
Data Sharing Statement
The raw data from the present research that were utilized and analyzed are available online as a supplementary material, or you can contact the corresponding author.
Ethics Approval and Consent to Participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by Institutional Review Board of the University of Jordan (Approval No. 1020229249; 1 March 2022). Informed written consent was obtained from the patients.
Acknowledgments
The authors appreciate the support of all the IVF unit at Jordan University Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for conducting this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fertility problems and fertility care in Sub-Saharan Africa: the case of Kenya | springerLink. Available from: https://link.springer.com/chapter/10.1007/978-3-030-24864-2_4.
2. Wang M, Yang X, Li L, et al. Incidence and risk factors for early pregnancy loss in women with first pregnancy undergoing in vitro fertilization-embryo transfer. BMC Pregnancy Childbirth. 2022;22(1):575. doi:10.1186/s12884-022-04904-8
3. Kava-Braverman A, Martínez F, Rodríguez I, Álvarez M, Barri PN, Coroleu B. What is a difficult transfer? Analysis of 7,714 embryo transfers: the impact of maneuvers during embryo transfers on pregnancy rate and a proposal of objective assessment. Fertil Steril. 2017;107(3):657–663.e1. doi:10.1016/j.fertnstert.2016.11.020
4. Schoolcraft WB, Surrey ES, Gardner DK. Embryo transfer: techniques and variables affecting success. Fertil Steril. 2001;76(5):863–870. doi:10.1016/S0015-0282(01)02731-5
5. D’Angelo A, Panayotidis C, Alteri A, Mcheik S, Veleva Z. Evidence and consensus on technical aspects of embryo transfer. Hum Reprod Open. 2022;2022(4):hoac038. doi:10.1093/hropen/hoac038
6. Practice Committee of the American Society for Reproductive Medicine. Electronic address: [email protected], practice committee of the American Society for reproductive medicine. Performing the embryo transfer: a guideline. Fertil Steril. 2017;107(4):882–896. doi:10.1016/j.fertnstert.2017.01.025
7. Kong L, Shao Y, Xia J, et al. Quantitative and qualitative analyses of psychological experience and adjustment of in vitro fertilization-embryo transfer patients. Med Sci Monit Int Med J Exp Clin Res. 2019;25:8069–8077.
8. Depalo R, Jayakrishan K, Garruti G, et al. GnRH agonist versus GnRH antagonist in in vitro fertilization and embryo transfer (IVF/ET). Reprod Biol Endocrinol RBE. 2012;10(1):26. doi:10.1186/1477-7827-10-26
9. Zhang M, Yang B-Y, Sun Y, et al. Non-linear relationship of maternal age with risk of spontaneous abortion: a case-control study in the china birth cohort. Front Public Health. 2022;10:933654. doi:10.3389/fpubh.2022.933654
10. Soler A, Morales C, Mademont-Soler I, et al. Overview of chromosome abnormalities in first trimester miscarriages: a series of 1,011 consecutive chorionic villi sample karyotypes. Cytogenet Genome Res. 2017;152(2):81–89. doi:10.1159/000477707
11. Xu T, de Figueiredo Veiga A, Hammer KC, Paschalidis IC, Mahalingaiah S. Informative predictors of pregnancy after first IVF cycle using eIVF practice highway electronic health records. Sci Rep. 2022;12(1):839. doi:10.1038/s41598-022-04814-x
12. Tomás C, Tikkinen K, Tuomivaara L, Tapanainen JS, Martikainen H. The degree of difficulty of embryo transfer is an independent factor for predicting pregnancy. Hum Reprod Oxf Engl. 2002;17(10):2632–2635. doi:10.1093/humrep/17.10.2632
13. Yang J, He Y, Wu Y, Zhang D, Huang H. Association between abnormal body mass index and pregnancy outcomes in patients following frozen embryo transfer: a systematic review and meta-analysis. Reprod Biol Endocrinol RBE. 2021;19(1):140. doi:10.1186/s12958-021-00809-x
14. Maheshwari A, Stofberg L, Bhattacharya S. Effect of overweight and obesity on assisted reproductive technology--a systematic review. Hum Reprod Update. 2007;13(5):433–444. doi:10.1093/humupd/dmm017
15. Rittenberg V, Seshadri S, Sunkara SK, Sobaleva S, Oteng-Ntim E, El-Toukhy T. Effect of body mass index on IVF treatment outcome: an updated systematic review and meta-analysis. Reprod Biomed Online. 2011;23(4):421–439. doi:10.1016/j.rbmo.2011.06.018
16. Tiras B, Korucuoglu U, Polat M, Saltik A, Zeyneloglu HB, Yarali H. Effect of blood and mucus on the success rates of embryo transfers. Eur J Obstet Gynecol Reprod Biol. 2012;165(2):239–242. doi:10.1016/j.ejogrb.2012.07.032
17. Tıras B, Cenksoy PO. Practice of embryo transfer: recommendations during and after. Semin Reprod Med. 2014;32(4):291–296. doi:10.1055/s-0034-1375181
18. Spitzer D, Haidbauer R, Corn C, Stadler J, Wirleitner B, Zech NH. Effects of embryo transfer quality on pregnancy and live birth delivery rates. J Assist Reprod Genet. 2012;29(2):131–135. doi:10.1007/s10815-011-9680-z
19. Goudas VT, Hammitt DG, Damario MA, Session DR, Singh AP, Dumesic DA. Blood on the embryo transfer catheter is associated with decreased rates of embryo implantation and clinical pregnancy with the use of in vitro fertilization-embryo transfer. Fertil Steril. 1998;70(5):878–882. doi:10.1016/S0015-0282(98)00315-X
20. Schoolcraft WB. Importance of embryo transfer technique in maximizing assisted reproductive outcomes. Fertil Steril. 2016;105(4):855–860. doi:10.1016/j.fertnstert.2016.02.022
21. Plowden TC, Hill MJ, Miles SM, et al. Does the presence of blood in the catheter or the degree of difficulty of embryo transfer affect live birth? Reprod Sci. 2017;24(5):726–730. doi:10.1177/1933719116667607
22. Phillips JAS, Martins WP, Nastri CO, Raine-Fenning NJ. Difficult embryo transfers or blood on catheter and assisted reproductive outcomes: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;168(2):121–128. doi:10.1016/j.ejogrb.2012.12.030
23. De Placido G, Wilding M, Stina I, et al. The effect of ease of transfer and type of catheter used on pregnancy and implantation rates in an IVF program. J Assist Reprod Genet. 2002;19(1):14–18. doi:10.1023/A:1014054421789
24. Leeton J, Trounson A, Jessup D, Wood C. The technique for human embryo transfer. Fertil Steril. 1982;38(2):156–161. doi:10.1016/S0015-0282(16)46451-4
25. Visser DS, Fourie FL, Kruger HF. Multiple attempts at embryo transfer: effect on pregnancy outcome in an in vitro fertilization and embryo transfer program. J Assist Reprod Genet. 1993;10(1):37–43. doi:10.1007/BF01204438
26. Listijono DR, Boylan T, Cooke S, Kilani S, Chapman MG. An analysis of the impact of embryo transfer difficulty on live birth rates, using a standardised grading system. Hum Fertil Camb Engl. 2013;16(3):211–214. doi:10.3109/14647273.2013.804956
27. Gullo G, Basile G, Cucinella G, et al. Fresh vs. frozen embryo transfer in assisted reproductive techniques: a single center retrospective cohort study and ethical-legal implications. Eur Rev Med Pharmacol Sci. 2023;27(14):6809–6823. doi:10.26355/eurrev_202307_33152
28. Yao Z, Vansteelandt S, Van der Elst J, Coetsier T, Dhont M, De Sutter P. The efficacy of the embryo transfer catheter in IVF and ICSI is operator-dependent: a randomized clinical trial. Hum Reprod. 2009;24(4):880–887. doi:10.1093/humrep/den453
29. Morin SJ, Franasiak JM, Juneau CR, Scott RT. LIve birth rate following embryo transfer is significantly influenced by the physician performing the transfer: data from 2707 euploid blastocyst transfers by 11 physicians. Fertil Steril. 2016;106(3):e25. doi:10.1016/j.fertnstert.2016.07.083
30. Cirillo F, Patrizio P, Baccini M, et al. The human factor: does the operator performing the embryo transfer significantly impact the cycle outcome? Hum Reprod Oxf Engl. 2020;35(2):275–282. doi:10.1093/humrep/dez290
31. Gullo G, Scaglione M, Buzzaccarini G, et al. Cell-free fetal DNA and non-invasive prenatal diagnosis of chromosomopathies and pediatric monogenic diseases: a critical appraisal and medicolegal remarks. J Pers Med. 2022;13(1):1. doi:10.3390/jpm13010001
32. Medenica S, Zivanovic D, Batkoska L, et al. The future is coming: artificial intelligence in the treatment of infertility could improve assisted reproduction outcomes-the value of regulatory frameworks. Diagn Basel Switz. 2022;12:2979.
33. Muhaidat N, Alshrouf MA, Karam AM, Elfalah M. Infertility management disruption during the COVID-19 outbreak in a middle-income country: patients’ choices, attitudes, and concerns. Patient Prefer Adherence. 2021;15:2279–2288. doi:10.2147/PPA.S327055
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
