Back to Journals » Psychology Research and Behavior Management » Volume 16
Factors Affecting Self-Harm- or Violence-Related Urgent Psychiatric Consultation During the COVID-19 Pandemic in Taiwan
Authors Yeh CC, Lee YT , Chien CY , Chen PC , Chen JH , Liu CH
Received 26 November 2022
Accepted for publication 19 April 2023
Published 8 May 2023 Volume 2023:16 Pages 1755—1762
DOI https://doi.org/10.2147/PRBM.S399242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Chung-Chen Yeh,1– 3,* Yu-Tung Lee,4,* Cheng-Yu Chien,5,6 Po-Cheng Chen,3,7 Jian-Hong Chen,3,8,9 Chun-Hao Liu3,10
1Department of Emergency Medicine, Keelung Chang Gung Memorial Hospital, Keelung City, Taiwan; 2Department of Emergency Medicine, Chang Gung Memorial Hospital at Linkou, Taoyuan City, Taiwan; 3College of Medicine, Chang Gung University, Taoyuan City, Taiwan; 4Department of Psychiatry, New Taipei Municipal Tucheng Hospital, New Taipei City, Taiwan; 5Graduate Institute of Management, Chang Gung University, Taoyuan City, Taiwan; 6Department of Emergency Medicine, Ton-Yen General Hospital, Hsinchu County, Taiwan; 7Department of Physical Medicine and Rehabilitation, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung City, Taiwan; 8Department of Psychiatry, Chang Gung Memorial Hospital at Keelung, Keelung City, Taiwan; 9National Taiwan Sport University, Taoyuan City, Taiwan; 10Department of Child & Adolescent Psychiatry, Chang Gung Memorial Hospital at Linkou, Taoyuan City, Taiwan
*These authors contributed equally to this work
Correspondence: Chun-Hao Liu, Department of Child & Adolescent Psychiatry, Chang Gung Memorial Hospital, Linkou, No. 5, Fu-Hsin St., Gueishan District, Taoyuan City, 333, Taiwan, Tel +886-3-3281200 ext 2439, Fax +886-3-3280267, Email [email protected]
Purpose: People’s health-care-seeking behaviors considerably changed during the COVID-19 pandemic. This study evaluated the changes in self-harm- and violence-related urgent psychiatric consultation (UPC) in the emergency department (ED) during different stages of the pandemic and at different levels of hospitals.
Patients and Methods: We recruited patients who received UPC during the baseline (2019), peak (2020), and slack (2021) periods of the same time window (calendar weeks 4– 18) during the COVID-19 pandemic. Demographic data such as age, sex, and referral type (by the police/emergency medical system) were also recorded.
Results: We found female gender and younger age associated with higher risk of self-harm-related UPCs, whereas patients visiting regional hospitals, male patients, and patients referred by the policy/emergency medical system, had a higher risk of violence-related UPCs. After adjustment, the different pandemic stages were not significantly associated with self-harm- or violence-related UPCs.
Conclusion: Patient’s demographic data, but not the pandemic itself, may be responsible for the changes in self-harm- and violence-related UPCs during the pandemic.
Keywords: COVID-19, emergency department, psychiatric consultation, self-harm, violence
Introduction
The COVID-19 pandemic has changed the lifestyle and health-care-seeking behaviors of people globally. Visits to the emergency department (ED), which is usually the first place where people with emergency conditions seek help, may reflect health-care-seeking behaviors. Many previous studies reported that ED visits markedly declined during the COVID-19 pandemic. A national survey conducted in the United States reported that the number of ED visits decreased by 42% during the early months of 2020 (pandemic period), as compared with the early months of 2019.1 A similar phenomenon was noted in Taiwan. A retrospective study conducted in Northern Taiwan revealed a 15.1% reduction in the total ED visits during the pandemic in 2020.2 Our previous studies also revealed that nonemergency diagnoses (eg, congestive heart failure and constipation) were more affected by the pandemic than emergency diagnoses (eg, myocardial infarction and gastrointestinal bleeding).3,4 Although the reasons for this may be complex, the fear of being infected is a possible explanation.5
Psychiatric diagnoses, including suicide or violence, are also common causes for ED visits and almost always warrant psychiatric consultation. The health-care-seeking behaviors of ED visitors were also affected during the pandemic. Although some studies reported that psychiatric ED visits were less affected,6 most large-scale surveys reported significant declines in the number of psychiatric ED visits during the pandemic. A Canadian study revealed a 37% decline in ED visits for mental health and substance use disorders during the pandemic,7 and a US study similarly reported an approximately 26% decline in psychiatric ED visits in 2020 relative to the visits in 2019.8 A large survey reported that the number of ED visits for mental health condition, suicide, and intimate partner violence significantly decreased after the stay-at-home order was announced.9 Although the psychiatric emergency admission rates decreased during the pandemic, a Spanish study reported a significant increase in the percentage of patients requiring acute psychiatric hospitalization during the same period.10 Changes in health-care-seeking behaviors during the pandemic may have resulted from multiple causes, including population vulnerability, exposure to media, economic status, and unemployment, all of which may have caused anxiety and stress symptoms.11 Data from urgent psychiatric consultations (UPCs) in EDs may help understand how people with mental health conditions changed their health-care-seeking behaviors during the pandemic and may explain the associated covariates.
Our previous study found that the number of UPCs at medical centers decreased during the pandemic.12 After COVID-19 pandemic, the proportion of self-harm-related UPCs increased, but that of violence-related UPCs decreased.12 Sex differences were also a significant factor affecting this phenomenon.12 In addition to patients’ demographic backgrounds, other factors such as the level of hospitals or referral patterns may have affected patients’ health-care-seeking behaviors.13,14 However, analyses of the effects and interactions between possible covariates, including patients’ characteristics, referral patterns, and levels of hospitals, are lacking. Accordingly, our study analyzed the factors affecting UPC patterns, particularly those for self-harm and violence, during the pandemic.
Materials and Methods
Study Design
This is a retrospective observational study and was conducted at two study sites – a tertiary referral medical center (general hospital, approximately 3500 beds) and a secondary regional hospital (general hospital, approximately 1000 beds). The hospital level was certified by the Taiwan Ministry of Health and Welfare, and the medical center had an emergency psychiatric protection room. Both the study sites were located in Northern Taiwan near to the epidemic center, and were emergency hospitals. The EDs of both the study sites were kept open for all patients during the pandemic, and 24×7 maintenance of acute consultations and psychiatric management were ensured. This study was conducted in accordance with the tenets of the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of Chang Gung Memorial Hospital (No. 202101591B0).
Study Period
The calendar weeks 4–18 of 2020 were defined as the peak period of the epidemic. This period began with the first COVID-19 case identified in Taiwan, and ended 6 weeks prior to the end of local restrictions and was considered the study period, as in our previous research, to avoid overlaps with another epidemic peak in 2021.4 Moreover, the calendar weeks 4–18 of 2019 were considered the baseline period, whereas the calendar weeks 4–18 of 2021 were considered the slack period. No community COVID-19 transmission was noted in Taiwan during the slack period.
Data Collection
The numbers of UPCs and total ED visits during the baseline, peak, and slack periods were recorded. Our study enrolled all adult patients who successfully completed their UPCs and were referred for psychiatric consultations according to the electronic medical records during the aforementioned study periods. Patients’ demographic data, including their age, sex, and referral type (by the police/emergency medical service [EMS]), were recorded in the electronic medical system. The primary outcomes included self-harm (self-harm behaviors, suicidal ideation, and suicide attempts) or violence (physical aggression and aggression toward objects) during the baseline, peak, and slack period. An additional file shows this database in more detail (see Additional file). Two trained emergency nurses read the consultation notes and decided if a patient’s chief complaint during the visit was related to self-harm or violence.
Statistical Analysis
The numbers of UPCs at the two study sites during the peak (2020) and slack (2021) periods were compared with those during the baseline (2019) period. Categorical variables, such as sex and referral type, were analyzed using the Pearson chi-square test, and are presented as numbers and percentages. Continuous variables, such as age, were analyzed using the independent t-test and are presented as means and standard deviations. Furthermore, multiple logistic regression models were used to identify the variables associated with the clinical presentation at ED (eg, self-harm or violence). Covariate factors (levels of hospital, pandemic period, referral type, age, and sex) are reported using the adjusted odds ratio (aOR) with 95% confidence interval. Two-tailed p < 0.05 was considered statistically significant. All data were analyzed using SPSS Statistics for Windows, version 26.0 (SPSS Inc., Chicago, IL, USA).
Results
For the regional hospital, 153 UPCs of 22,226 ED visits (0.69%) were found during the baseline period (2019), as well as 121 UPCs of 17,150 ED visits (0.71%) during the peak period (2020), and 105 UPCs of 17,780 ED visits (0.59%) during the slack period (2021) (Table 1). For the medical center, 323 UPCs of 50,938 ED visits (0.63%) were found during the baseline period (2019), as well as 186 UPCs of 33,939 ED visits (0.55%) during the peak period (2020), and 268 UPCs of 38,488 ED visits (0.7%) during the slack period (2021).
 |
Table 1 UPCs and Total ED Visits of the Medical Center and Regional Hospital During the Pandemic |
Demographic Data
In the medical center, 45.2%, 34.9%, and 38.4% of male patients and 38.7%, 41.9% and 51.9% of patients with police/EMS referrals received UPCs during the baseline, peak, and slack periods, respectively (Table 2). Patients who received UPCs during the baseline, peak, and slack periods were aged 41.8±17.4, 39.2±18.5, and 35.6±17.2 years, respectively. According to the data, significantly fewer male patients (34.9% vs 45.2%, p < 0.05, compared to the baseline period) during the peak period, and younger patients (aged 35.6±17.2 years vs 41.8±17.4 years, p < 0.001) and more patients with police/EMS referral (51.9% vs 38.7%, p < 0.01) during the slack period (compared to the baseline period) received UPCs, as in our previous study.12
 |
Table 2 Demographic Data of ED Patients Received UPC in the Medical Center and Regional Hospital During Different Pandemic Periods |
In the regional hospital, 37.3%, 43.8%, and 42.9% of male patients and 43.1%, 42.1%, and 41% of patients with police/EMS referral received UPCs during the baseline, peak, and slack periods, respectively. Patients who received UPCs during the baseline, peak, and slack periods were aged 45.1±18.8, 41.1±17.8, and 44.3±18.9 years, respectively. No significant differences were noted in the aforementioned covariates between the baseline period and the peak or slack periods.
Covariates Affecting Self-Harm Related UPCs During the Pandemic
In the peak and the slack periods, male patients (aOR = 0.51 [0.378–0.688] and aOR = 0.543 [0.408–0.724], respectively) and older patients (aOR = 0.987 [0.978–0.995] and aOR = 0.982 [0.975–0.990]) had a lower risk for self-harm related UPCs (Table 3).
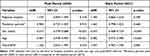 |
Table 3 Multiple Logistic Regression on Self-Harm During the COVID-19 Pandemic Compared to the Baseline Period (2019) |
Covariates Affecting Violence Related UPCs During the Pandemic
In the peak and slack periods, male patients (aOR = 2.326 [1.588–3.407] and aOR = 2.285 [1.583–3.299], respectively) and patients with police/EMS referrals (aOR = 2.824 [1.918–4.160] and aOR = 2.728 [1.874–3.972]) had a higher risk for violence-related UPCs (Table 4). Compared with the medical center, the regional hospital (aOR = 2.157 [1.472–3.162] and aOR = 2.148 [1.472–3.133]) referred more patients for violence-related UPCs during the peak and slack periods.
 |
Table 4 Multiple Logistic Regression on Violence During the COVID-19 Pandemic Compared to the Baseline Period (2019) |
Discussion
In the present study, we found during the pandemic, certain demographic covariates such as male sex and younger age associated with lower risk for self-harm-related UPCs. On the other hand, male sex associated with higher risk for violence-related UPCs, but age was not significantly associated with the risk. Moreover, regional hospital and patients with police/EMS referral associated with higher risk for violence-related UPCs, but not for self-harm-related UPCs.
The demographic characteristics of patients seeking an ED visit, including age and sex, were more important than the levels of hospitals and the pandemic periods in terms of their association with self-harm-related ED visits. Referral by the police/EMS was not associated with a significantly higher risk of self-harm behaviors, as reported in a previous study in the same medical center in northern Taiwan.12 According to most reports, although the suicide rate was higher among male patients and older patients,15 female patients and young patients were at higher risk of self-harm behaviors.16 Another survey revealed that suicide attempts were more common in female patients than male patients visiting Taiwanese EDs.17 Our previous studies revealed an increased proportion of female patients and lower average age of patients received UPC after the pandemic.12 The COVID-19 pandemic may have different effects on populations with different socio-demographic backgrounds. For example, compared with male patients, female patients expressed greater concerns regarding COVID-19-related impact.18 Female and younger patients also experienced higher psychological distress during the pandemic compared to its baseline.19 Other online surveys also revealed similar results across different countries.20–22 In New Zealand, female and young people suffered from higher psychological distress than male and people in old age during the COVID-19 pandemic.23 Similar to our study, a Spanish study revealed female people had higher risk of suicidal behavior in emergency department visit.24 A Japanese survey found young female (less than age 40) had the largest increase of the number of suicide deaths in 2020 compared to baseline (2017–2019).25 Moreover, female health-care workers experienced more depression, anxiety, insomnia, and psychological distress than their male counterparts.26 These findings demonstrated that the mental health issues of the vulnerable populations, such as younger or female patients, should be taken seriously considered during the pandemic.
Fountoulakis et al established a conceptual model to explain how the COVID-19 pandemic affects people’s mental health.27 Family responsibilities, younger age, and financial difficulty may increase the risk of clinical depression, whereas daily life management, conspiracy theories, and religiosity were reported as protective factors.27 Their findings explain how social adversity can affect people’s mental health during the pandemic, and possible intervention approaches were provided in the study.
Our study found that referral by the police/EMS referral increased the likelihood of violence-related UPCs, but not self-harm-related UPCs. However, this effect was not clearly observed in our previous study.12 Contrary to the decrease in violence-related UPCs at medical center during the pandemic, regional hospital was associated with a higher risk of violence-related UPCs. This phenomenon might contribute to the fear of getting infected in a crowded setting, such as a medical center, but might also contribute to the population where our study sites are located. To the best of our knowledge, no previous study has focused on the changes in violence patterns among psychiatric patients during the pandemic. How the pandemic affects psychiatric violence behaviors requires further investigation.
Most published studies focused on the change of domestic violence28 or intimate partner violence (IPV)9 during the pandemic. The shelter-in-place order may have played a role in the increased number of domestic violence cases. A US survey found a 11% increase in domestic crimes during the shelter-in-place order, however, the overall crime rate decreased by 20%.28 The pandemic not only increased the risk of domestic violence, but also affected the victims’ help-seeking behaviors. Although other mental health condition-related ED visits (including those for suicide attempts or overdose) increased during the pandemic, the total count of ED visits for IPV decreased.9 This phenomenon should be interpreted with caution because it may imply a low incidence of IPV; however, it is possible that the fear of getting infected and the limited availability of medical resources kept the victims from seeking help.
This study has some limitations. First, the data were obtained from two levels of hospitals; thus, the results cannot be simply generalized to all hospital facilities. Second, we only collected data from 2019 to 2021; thus, we cannot interpret the changes in the trends. Third, the data was collected from the ED electronical medical record system; thus, many important covariates such as patients’ psychiatric histories or household income details were not included in our study. A population-based, long-term study including more details such as patients’ psychiatric histories and detailed demographic data are warranted in the future.
Conclusions
Our study revealed that female and younger patients were at higher risk of self-harm compared to male and older patients, whereas patients who visited regional hospital (compared to medical center), male patients (compared to female), and patients with police/EMS referrals (compared to other referral sources) were at higher risk of violence. The pandemic period (compared to baseline period), however, not significantly associated with self-harm or violence. Our study raises the concerns regarding the mental health of vulnerable populations, such as those including young female individuals, which should be further investigated considering the pandemic.
Abbreviations
aOR, Adjusted odds ratio; CI, Confidence interval; ED, Emergency department; EMS, Emergency medical service; IPV, Intimate partner violence; UPC, Urgent psychiatric consultation.
Data Sharing Statement
The authors agree to make our data available upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Chang Gung Memorial Hospital Institutional Review Board (No. 202101591B0C601). The study protocol has been performed in accordance with the Declaration of Helsinki. Consent to participate is not applicable. The need for informed consent was waived by the Chang Gung Memorial Hospital Institutional Review Board (No. 202101591B0C601). The Institutional Review Board reviewed and determined that it is expedited review according to personal information, data, documents, or specimens collected from legal biological databases without hyperlink or identifiable information can be used for research, but cannot be involved in the interests of individuals or groups.
Acknowledgments
This manuscript was edited by Wallace Academic Editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi:10.15585/mmwr.mm6923e1
2. Lai YW, Hsu C-T, Lee Y-T, et al. Analysis of COVID-19 pandemic impact on the presenting complaints of the emergency department visits. Medicine. 2021;100(51):e28406. doi:10.1097/MD.0000000000028406
3. Kuo T, Liu CH, Chien CY, et al. Impact of COVID-19 by pandemic wave among patients with gastroenterology symptoms in the emergency departments at a medical center in Taiwan. Int J Environ Res Public Health. 2022;19(12):7516.
4. Yeh CC, Chien C-Y, Lee T-Y, et al. Effect of the COVID-19 pandemic on emergency department visits of patients with an emergent or urgent diagnosis. Int J Gen Med. 2022;15:4657–4664. doi:10.2147/IJGM.S362615
5. Kostopoulou E, Gkentzi D, Papasotiriou M, et al. The impact of COVID-19 on paediatric emergency department visits. A one-year retrospective study. Pediatr Res. 2022;91(5):1257–1262. doi:10.1038/s41390-021-01815-w
6. Heppner Z, Shreffler J, Polites A, et al. COVID-19 and emergency department volume: the patients return but have different characteristics. Am J Emerg Med. 2021;45:385–388. doi:10.1016/j.ajem.2020.09.009
7. Saunders NR, Toulany A, Deb B, et al. Acute mental health service use following onset of the COVID-19 pandemic in Ontario, Canada: a trend analysis. CMAJ Open. 2021;9(4):E988–E997. doi:10.9778/cmajo.20210100
8. Goldenberg MN, Parwani V. Psychiatric emergency department volume during Covid-19 pandemic. Am J Emerg Med. 2021;41:233–234. doi:10.1016/j.ajem.2020.05.088
9. Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(4):372–379. doi:10.1001/jamapsychiatry.2020.4402
10. Gómez-Ramiro M, Fico G, Anmella G, et al. Changing trends in psychiatric emergency service admissions during the COVID-19 outbreak: report from a worldwide epicentre. J Affect Disord. 2021;282:26–32. doi:10.1016/j.jad.2020.12.057
11. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
12. Liu C-H, Chen P-C, Chen J-H, et al. Changes in self-harm- and violence-related urgent psychiatric consultation in the emergency department during the different stages of the COVID-19 pandemic. BMC Psychiatry. 2022;22(1):384. doi:10.1186/s12888-022-04029-4
13. Simpson SA, Loh RM, Cabrera M, et al. The impact of the COVID-19 pandemic on psychiatric emergency service volume and hospital admissions. J Acad Consult Liaison Psychiatry. 2021;62(6):588–594. doi:10.1016/j.jaclp.2021.05.005
14. Rømer TB, Christensen RHB, Blomberg SN, et al. Psychiatric admissions, referrals, and suicidal behavior before and during the COVID-19 pandemic in Denmark: a time-trend study. Acta Psychiatr Scand. 2021;144(6):553–562. doi:10.1111/acps.13369
15. Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–1381. doi:10.1016/S0140-6736(09)60372-X
16. Gillies D, Christou MA, Dixon AC, et al. Prevalence and characteristics of self-harm in adolescents: meta-analyses of community-based studies 1990–2015. J Am Acad Child Adolesc Psychiatry. 2018;57(10):733–741. doi:10.1016/j.jaac.2018.06.018
17. Lin CJ, Lu H-C, Sun F-J, et al. The characteristics, management, and aftercare of patients with suicide attempts who attended the emergency department of a general hospital in northern Taiwan. J Chin Med Assoc. 2014;77(6):317–324. doi:10.1016/j.jcma.2014.02.014
18. Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266:113364. doi:10.1016/j.socscimed.2020.113364
19. McGinty EE, Presskreischer R, Han H, et al. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi:10.1001/jama.2020.9740
20. Park CL, Russell BS, Fendrich M, et al. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35(8):2296–2303. doi:10.1007/s11606-020-05898-9
21. Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. 2020;66(5):504–511. doi:10.1177/0020764020927051
22. Elsayed M, Schönfeldt-Lecuona C, Welte XA, et al. Psychological distress, fear and coping strategies during the second and third waves of the COVID-19 pandemic in Southern Germany. Front Psychiatry. 2022;13:860683. doi:10.3389/fpsyt.2022.860683
23. Every-Palmer S, Jenkins M, Gendall P, et al. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: a cross-sectional study. PLoS One. 2020;15(11):e0241658. doi:10.1371/journal.pone.0241658
24. Irigoyen-Otiñano M, Nicolau-Subires E, González-Pinto A, et al. Characteristics of patients treated for suicidal behavior during the pandemic in a psychiatric emergency department in a Spanish province. Revista De Psiquiatría Y Salud Mental. 2022. doi:10.1016/j.rpsm.2022.03.004
25. Ueda M, Nordström R, Matsubayashi T. Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health. 2022;44(3):541–548. doi:10.1093/pubmed/fdab113
26. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976
27. Fountoulakis KN, Apostolidou MK, Atsiova MB, et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. 2021;279:624–629. doi:10.1016/j.jad.2020.10.061
28. Evans DP, Hawk SR, Ripkey CE. Domestic violence in Atlanta, Georgia before and during COVID-19. Violence Gend. 2021;8(3):140–147. doi:10.1089/vio.2020.0061
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
