Back to Journals » Journal of Pain Research » Volume 10
Factors affecting patients’ comfort during fiberoptic bronchoscopy and endobronchial ultrasound
Authors Yıldırım F, Özkaya Ş , Yurdakul AS
Received 25 July 2016
Accepted for publication 28 December 2016
Published 29 March 2017 Volume 2017:10 Pages 775—781
DOI https://doi.org/10.2147/JPR.S118047
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Fatma Yıldırım,1 Şevket Özkaya,2 Ahmet Selim Yurdakul1
1Department of Pulmonary Medicine, Faculty of Medicine, Gazi University, Ankara, Turkey; 2Department of Pulmonary Medicine, Faculty of Medicine, Bahcesehir University, Istanbul, Turkey
Objective: This study investigated the factors that can affect the comfort of patients who underwent diagnostic fiberoptic bronchoscopy (FOB) and diagnostic endobronchial ultrasonography (EBUS) for the first time and the effect of the patients’ anxiety level on their comfort during the procedure.
Materials and methods: We recorded the demographics of the patients, the medications they used previously, the anesthesia applied during the procedure, the experience of the operator, the insertion technique of the bronchoscope, the types of the bronchoscopic interventions during the procedure, the duration of the procedure, and the anxiety levels of the patients before the session. Patients’ discomfort level before and after the procedure and anxiety levels before the procedure were evaluated using a visual analog scale (VAS), and willingness for repeating FOB and EBUS was assessed using a questionnaire.
Results: We found that longer examination time, higher anxiety level before the procedure, the nasal insertion of bronchoscope, and higher number of interventions are related to the increased discomfort during FOB and EBUS. Patients’ willingness for repeating FOB and EBUS increased as the level of discomfort decreased during the procedure.
Conclusion: The patient’s anxiety level should be determined using a questionnaire before the FOB and EBUS procedures, and the operator should adjust their procedure according to the patients’ anxiety level.
Keywords: patient comfort, fiberoptic bronchoscopy, endobronchial ultrasound, patient anxiety, preprocedure questionnaire, patient willingness
Introduction
Fiberoptic bronchoscopy (FOB) and endobronchial ultrasonography (EBUS) are among the widely used procedures for diagnosis and treatment of various lung diseases. The majority of patients who underwent FOB and EBUS complain of discomforts during the process due to asphyxia, cough, nausea, and feeling of choking.1,2 Patients often remember the process as a negative experience due to their unpleasant feelings during procedure and they even refuse to repeat the procedure.3 To minimize patient discomfort during the process and increase the effectiveness of the process, some preparations are made before the FOB and EBUS. Although there are general guidelines and recommendations for premedication, there is no exact protocol for this. The sedative and analgesic premedications can increase patient satisfaction, and they seem to provide the benefit of reducing the patients’ discomfort during the procedure.4,5 Previous studies have shown that the anxiety levels of the patients before the procedure and the experience of the operator carrying out the process affect the patients’ comfort during FOB.6,7 In this study, we sought to clarify the factors that affect the comfort of patients who underwent diagnostic FOB and EBUS for the first time, and also examine the effect of the patients’ anxiety level before the procedure on their discomfort level during the procedure.
Materials and methods
We included a total of 250 patients (174 males and 76 females) who underwent diagnostic FOB and EBUS for the first time at the Faculty of Medicine, Department of Pulmonary Medicine, Gazi University, between April 2011 and April 2012. Our study was approved by the ethics committee of Gazi University Medical Faculty. The application methods of procedures, the reasons of the procedures, and possible complications were explained to all patients before the procedures. All patients or their relatives gave written informed consent that included the information about the acceptance of the procedure.
We excluded the patients who underwent FOB or EBUS previously, patients with tracheostomy, patients who did not give written informed consent to participate in the study, and the patients who did not want to answer the questionnaire after the procedure.
During the procedure, the arterial blood pressure, heart rate, and rhythm of all patients were monitored. Transcutaneous oxygen saturations of patients were followed up by pulse oximetry. Supplemental oxygen was given to all patients, and 95% oxygen saturation (SaO2) was achieved for all patients.
Anesthesia of the posterior oropharynx and both nares of the patients was achieved using 10% lidocaine. A total of 5 mL of 2% lidocaine was given in the form of nebulization before the procedures. In addition, for the anesthesia of the vocal cord and the tracheobronchial tree, 2% lidocaine was used. Midazolam was administered intravenously between 0.05 and 0.1 mg/kg doses. Midazolam doses were set according to patients’ sedation level.
All operations were performed while the patients were in supine position. FOB procedures were performed by transnasal or transoral routes. All EBUS procedures were performed by the transoral route. Some of the FOB procedures were performed by less-experienced operators, and some of them were performed by experienced operators. However, less-experienced operators had been trained theoretically and practically about the FOB from the beginning of their education. All the EBUS procedures were performed by experienced operators. An operator who has been performing the FOB and EBUS for 5 years was defined as experienced.
A questionnaire was distributed to all patients before the procedures. Patients rated their anxiety level before the procedure on this questionnaire. After the procedure, 2 hours later, patients rated their discomfort level during the procedure on the same questionnaire, and they also answered the question related to their willingness for repetition of procedures in the future.
We used a visual analog scale (VAS)6,7 to evaluate the patients’ anxiety and discomfort levels within the questionnaire. The VAS consisted of a 100 mm long horizontal straight line defined by anchors with verbal labels, the left end point (0 mm) indicating no discomfort and the right end point (100 mm) indicating overwhelming discomfort as well as anxiety. We determined the VAS score (1 mm = 1) by measuring the distance from the left end point to the mark made by the patient (Table 1). We evaluated the patients who answered 1 or 2 to question 3 to be willing for repetition of procedure in the future. The patients who answered 3 or 4 to question 3 were evaluated as unwilling. According to the patients’ anxiety levels, patients were separated into two groups: the low anxiety group (less than the median of the VAS score) and the high anxiety group (the median of the VAS score or greater).
  | Table 1 Survey form |
Since some of our patients were illiterate, we preferred to use a VAS. The patients easily marked their anxiety and discomfort levels on the chart when the question was read by the operator.
Statistics
All statistical analyses were performed using SPSS for Windows (Version 17.0, SPSS Inc). A pilot study was carried out that included 45 patients. Based on these data, it was estimated that 250 patients were needed to have a power of 95% confidence interval. In addition, descriptive statistical methods (mean, standard deviation, median, frequency) and Student’s t-test were used to compare percentage of groups’ discomfort during the procedure and differences between the groups. The univariate χ2 test was used to compare qualitative data. The results were evaluated with 95% confidence interval and were considered significant at p < 0.05. The factors affecting the patients’ discomfort during the procedures as a result of univariate analysis were then reevaluated using multiple regression analysis to identify independent factors.
Results
In the study group, 174 (69.6%) patients were males and 76 (30.4%) were females. Their mean age was 56.5±13.7 years. A total of 214 (85.6%) patients underwent FOB and 36 (14.4%) underwent EBUS. The mean age was 56.2±13.9 years, the mean operation time was 24.4±10.5 minutes, and the mean preoperative anxiety score was 52.7±33.4 VAS of the FOB group. The mean age of the EBUS group was 57.9±12.2 years, the mean operation time was 30.0±10.7 minutes, and the mean preoperative anxiety score was 38.3±32.8 VAS (Table 2).
  | Table 2 General characteristics of the groups Abbreviations: FOB, fiberoptic bronchoscopy; EBUS, endobronchial ultrasonography; VAS, visual analog scale; TBNA, transbronchial needle aspiration. |
Although 48 (22.4%) patients in the FOB group stated no discomfort during the procedure, 166 (77.6%) stated a feeling of at least one of the following symptoms: coughing, nausea, choking, or others. In the EBUS group, 13 (36.1%) patients stated no discomfort during the procedure, 23 (63.9%) stated at least one symptom during the procedure (Table 3).
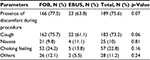  | Table 3 Rates of discomfort during the procedures Abbreviations: FOB, fiberoptic bronchoscopy; EBUS, endobronchial ultrasonography. |
A median discomfort level of the FOB group during the procedure was 40 VAS. We divided the FOB group’s patients into two groups: the low-discomfort group (<40 VAS) and the high-discomfort group (≥40 VAS). In the FOB group, female patients, patients with high preoperative anxiety, patients with longer procedure time, patients who received antihypertensive drugs due to preoperative hypertension, patients who received midazolam, patients with COPD, hospitalized patients, and the patients who were applied bronchial lavage, bronchoalveolar lavage (BAL), and transbronchial biopsy during the procedure had higher level of discomfort during the procedure (p < 0.05). However, the operator’s experience was not a factor that affected the patients’ discomfort during the procedure (p > 0.05; Table 4).
  | Table 4 Factors affecting the level of discomfort during FOB Abbreviations: FOB, fiberoptic bronchoscopy; VAS, visual analog scale; TBNA, transbronchial needle aspiration. |
In patients who underwent EBUS, the median discomfort level was 27.5 VAS during the procedure. The patients were also divided into two groups: the low-discomfort group (<27.5 VAS) and the high-discomfort group (≥27.5 VAS; Table 5). In the EBUS group, the patients with high preoperative anxiety level and longer operation time had significantly higher discomfort during the procedure (p<0.05). While the mean discomfort level of the patients who underwent procedure as outpatients was 39.0±27.9 VAS, the mean discomfort level of hospitalized patients was 46.8+29.8 VAS in the FOB group. This difference was statistically significant (p=0.04).
In the FOB group, 149 (69.6%) patients stated positive feelings related to repetition of FOB in the future, whereas 65 (30.3%) reported negative feelings. In the EBUS group, 31 (86.1%) patients reported positive feelings for repetition of EBUS in the future, and five (13.8%) reported negative feelings (Table 6).
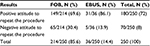  | Table 6 Willingness to repeat the procedure Abbreviations: FOB, fiberoptic bronchoscopy; EBUS, endobronchial ultrasonography. |
We found that duration of the procedure and insertion site are factors independently affecting the patients’ discomfort level during procedure in the study group at the end of the multivariate analysis. The patients’ discomfort level was more when the procedure time was longer and the insertion site was the nasal route (Table 7).
When we separately evaluated the FOB and EBUS groups, sex, preoperative anxiety level, and insertion site were found to be the independent factors increasing the patients’ discomfort level during the procedure in the FOB group. The discomfort level increased in female patients, in patients with high preoperative anxiety level, and in patients whose insertion site was the nasal route (Table 8).
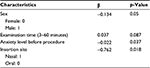  | Table 8 Multivariate analysis of factors affecting patient discomfort during FOB Abbreviations: FOB, fiberoptic bronchoscopy; β: regression beta coefficient. |
Evaluation of the 149 (69.6%) patients with positive feelings for repetition of procedure in the FOB group showed that 90 (60.4%) patients were in the low-discomfort group and 59 (39.6%) were in the high-discomfort group.
In the EBUS group, 32 (88.8%) patients had positive feelings for repetition of procedure, of whom 18 (56%) patients were in the low-discomfort group and 12 (44%) patients were in the high-discomfort group.
Discussion
In this prospective study, we found that duration of the procedure and anxiety of the patients before the procedure are the major factors affecting the patients’ comfort during both FOB and EBUS. Moreover, nasal insertion and female gender are the additional factors affecting the comfort of patients undergoing FOB.
FOB and EBUS are invasive diagnostic methods in various pulmonary diseases. Patients can express their FOB or EBUS experience as a distressing and uncomfortable procedure. Most of the patients disagree to repeat the FOB or EBUS procedure because of their negative past experience. Nakaoka et al1 stated that 30% of their patients underwent two or more FOB procedures, but 22.5% of the patients who underwent FOB did not want to undergo FOB again. So, the first FOB or EBUS procedure that the patients underwent has a great significance to get a comfortable and well-remembered procedure.
Previous studies showed that the lower the degree of discomfort of patients during the FOB procedure, the higher their consent was for repetition of procedure.3,6,8 Therefore, factors that can affect the patients’ comfort during the procedure and their discomfort associated with the procedure should be investigated.
In the study of Hirose et al,7 the patients had reported the following discomfort feelings: choking (90.7%), coughing (86.0%), sore throat (33.3%), chest pain (32.6%), and pain during swallowing (62.8%) during FOB. Coughing was the main discomfort feeling during the procedure for FOB and EBUS groups in our study. While this rate was found to be 75.7% in the FOB group, it was 61.1% in the EBUS group. High incidence of coughing can be associated with the use of antitussive drugs in the FOB group. In the study of Stolz et al,9 no meaningful difference was found between the coughing scores of the operator and the patients’ discomfort level during the procedure. They concluded that the administration of nebulized lidocaine during FOB had no effect on the patients’ discomfort due to the administration of hydrocodone to all patients and the antitussive effect of hydrocodone.9 Steinfort and Irving prospectively investigated the patients’ discomfort under conscious sedation during EBUS-transbronchial needle aspiration (TBNA).10 Coughing had been found the most common complaint (71%) in their study. In our study, coughing was found in 61.1% of the patients in the EBUS group.
The median discomfort level of the patients was 40 VAS in the FOB group and 27.5 VAS in the EBUS group. The higher level of discomfort in the FOB group was considered to be due to the higher number of interventions (Bronchial lavage, punch biopsy, transbronchial biopsy, and others) in the FOB group, and fewer interventions (Bronchial lavage and EBUS-TBNA) were performed during EBUS.
Our study found that the experience of operator had no effect on the patients’ discomfort level in the FOB group. This can be due to the training (theoretical and practical) of less-experienced operators on FOB since the start of their education and the availability of experienced operators in the bronchoscopy unit when the less-experienced operator performs the procedure. Similar to our study, Hirose et al7 found no correlation between the operator’s experience and patient satisfaction.
Although we did not investigate in our study, previous studies showed that the time that was spent by the operator to explain the nature of the procedure including how it will be applied and how sampling will be done to the patients was more important than the operator’s experience on the patients’ discomforts and their satisfaction.7,11 However, Uzbeck et al,12 in their prospective study, investigated the patients’ preoperative anxiety levels according to the standard and detailed disclosure to the patients before the FOB and they investigated its effect on patient satisfaction. They found that the patients’ preoperative anxiety levels had been increased two times when the patients are preoperatively informed in detail about the procedure and its complications. They concluded that informing the patients in detail before the FOB had no positive effect on patients’ satisfaction.12
We found that the mean preoperative anxiety level of the FOB group was 52.7±3.4 VAS, whereas the preoperative mean anxiety level of the EBUS group was 38.3±32.8 VAS. Preoperative anxiety levels of patients were significantly higher in the high-discomfort groups in both the FOB and EBUS groups. Mitsumune et al6 also found a similar result in their study. Preoperative anxiety level of the high-discomfort group was found to be significantly higher in their study. They also reported that the patients’ discomfort levels were increased when the procedures were performed by the less-experienced operator in the high-anxiety group. They found that patients’ discomfort levels were parallel to preoperative anxiety levels. Their study also reported that the high-discomfort group received less care from experienced operators and that caused to increase the patients’ preoperative anxiety level.6
Our study found no meaningful effects of the patients’ additional diseases and the drugs previously used on the discomfort levels of patients in the FOB and EBUS groups. A study by Hirose et al7 also found no meaningful correlation between the patients’ health conditions and their discomfort during the procedure. Lechtzin et al in their study stated that the patients’ comfort during the procedure and their overall health condition were independent predictive factors for the repetition of the procedure. They showed that the patients’ overall health conditions positively affected the toleration of the patients.11 Our study found that patients who underwent procedures as outpatients tolerated the procedure better; on the other hand, hospitalized patients felt more discomfort during the procedures. This was attributed to higher preoperative anxiety level of the patients due to their other medical diseases.
Our study found that the procedure time was significantly longer in the high-discomfort group in the FOB group. In a study by Steinfort et al,10 they investigated patients’ comfort during EBUS-TBNA. Mean procedure time was found to be 31.0±8.0 minutes, and 98% of the patients stated that they would repeat the procedure in their study. In our study, the mean procedure time of the high-discomfort group in the EBUS group was 30.0±10.7 minutes, and 31 (86.1%) of all cases had positive feelings for repetition of the EBUS. In Hirose et al’s7 study, procedure time had no effect on the discomfort level of the patients during the procedure.
In a study by Choi et al, the effect of insertion via the nasal and oral routes on the patients’ satisfaction was investigated during FOB. Patients in the nasal insertion group stated to have higher discomfort during the application of anesthesia and during insertion. In addition, the nasal insertion group had a higher level of coughing and shortness of breath. The authors did not find any differences between the groups in willingness for the repetition of procedure.13 In our study, we found that nasal route in the FOB group was an independent risk factor increasing the patient’s discomfort level. This was attributed to the fewer number of patients who received FOB via oral route in the FOB group.
Hirose et al7 reported that male patients felt less discomfort during FOB in their study, and they were more willing for the repetition of procedure. Likewise, Poi et al14 and Putinati et al3 stated that female patients were more anxious and had more discomfort during the procedure.7 Similar to the previous studies, we also found that female patients had higher discomfort level in the FOB group. This was attributed to female patients being more anxious preoperatively. No differences were found between the males’ and females’ discomfort levels in the EBUS group in our study.
In our study, willingness for the repetition of procedure was 69.6% in the FOB group and 86.1% in the EBUS group, respectively. Lechtzin et al15 reported that 71% of their patients definitely agreed to repeat the procedure, 22% could have to repeat the procedure, and 7% definitely disagreed to repeat the procedure in their study. Higher number of patients had positive feelings for the repetition of procedure in the EBUS group. This was attributed to the fewer number of interventions and the lack of irritating interventions such as transbronchial biopsy, bronchoalveolar lavage, and punch biopsy during EBUS.
One of the limitations of our study was the lack of a scale to evaluate the patients’ overall health conditions instead of examining them for the presence of additional diseases. Another limitation was the lack of evaluation of the operator-dependent factors. Despite the evaluation of the operator’s experience, the operator’s skill, the ability to relieve the patients’ anxiety, and the time which the operator spent to inform the patients preoperatively about procedure were not evaluated in our study.
Conclusion
The use of a questionnaire including the measurement of patients’ anxiety level will help to identify the patients who will have more discomfort during FOB and EBUS before procedure. According to patients’ anxiety level, the operator can prefer the oral route or can shorten the procedure time with less intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
Nakaoka Y, Ohata M, Iida M. Anesthesia for diagnostic bronchoscopy. Kikanshigaku. 1990;12:254–261. | ||
Diette GB, White P Jr, Terry P, Jenckes M, Wise RA, Rubin HR. Quality assessment through patient self-report of symptoms prefiberoptic and postfiberoptic bronchoscopy. Chest. 1998;114(5):1446–1453. | ||
Putinati S, Ballerin L, Corbetta L, Trevisani L, Potena A. Patient satisfaction with conscious sedation for bronchoscopy. Chest. 1999;115(5):1437–1440. | ||
Williams T, Brooks T, Ward C. The role of atropine premedication in fiberoptic bronchoscopy using intravenous midazolam sedation. Chest. 1998;113(5):1394–1398. | ||
Utz JP, Prakash UBS. Indications and contraindications to bronchoscopy. In: Prakash UBS, editor. Bronchoscopy. 1st ed. New York: Raven Press; 1994:81–89. | ||
Mitsumune T, Senoh E, Adachi M. Prediction of patient discomfort during fiberoptic bronchoscopy. Respirology. 2005;10(1):92–96. | ||
Hirose T, Okuda K, Ishida H, et al. Patient satisfaction with sedation for flexible bronchoscopy. Respirology. 2008;13(5):722–727. | ||
Maltais F, Laberge F, Laviolette M. A randomized, double-blind, placebo-controlled study of lorazepam as premedication for bronchoscopy. Chest. 1996;109(5):1195–1198. | ||
Stolz D, Chhajed PN, Leuppi JD, et al. Cough suppression during flexible bronchoscopy using combined sedation with midazolam and hydrocodone: a randomised, double-blind, placebo-controlled trial. Thorax. 2004;59(9):773–776. | ||
Steinfort DP, Irving LB. Patient satisfaction during endobronchial ultrasound-guided transbronchial needle aspiration performed under conscious sedation. Respir Care. 2010;55(6):702–706. | ||
Lechtzin N, Rubin HR, Jenckes M, et al. Predictors of pain control in patients undergoing flexible bronchoscopy. Am J Respir Crit Care Med. 2000;162(2 pt 1):440–445. | ||
Uzbeck M, Quinn C, Saleem I, Cotter P, Gilmartin JJ, O’Keeffe ST. Randomised controlled trial of the effect of standard and detailed risk disclosure prior to bronchoscopy on peri-procedure anxiety and satisfaction. Thorax. 2009;64(3):224–227. | ||
Choi CM, Yoon HI, Lee SM, et al. Oral insertion of a flexible bronchoscope is associated with less discomfort than nasal insertion for Korean patients. Int J Tuberc Lung Dis. 2005;9(3):344–348. | ||
Poi PJ, Chuah SY, Srinivas P, Liam CK. Common fears of patients undergoing bronchoscopy. Eur Respir J. 1998;11(5):1147–1149. | ||
Lechtzin N, Rubin HR, White P Jr, et al. Patient satisfaction with bronchoscopy. Am J Respir Crit Care Med. 2002;166(10):1326–1331. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


