Back to Journals » Clinical Ophthalmology » Volume 16
Factors Affecting Compliance with Diabetic Retinopathy Screening: A Qualitative Study Comparing English and Spanish Speakers
Authors Hudson SM , Modjtahedi BS, Altman D, Jimenez JJ, Luong TQ , Fong DS
Received 15 October 2021
Accepted for publication 20 December 2021
Published 4 April 2022 Volume 2022:16 Pages 1009—1018
DOI https://doi.org/10.2147/OPTH.S342965
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sharon M Hudson,1,2 Bobeck S Modjtahedi,2– 4 Danielle Altman,2 Jennifer J Jimenez,2 Tiffany Q Luong,2 Donald S Fong2,3
1Keck School of Medicine of USC/Children’s Hospital Los Angeles, Los Angeles, CA, USA; 2Department of Research and Evaluation, Southern California Permanente Medical Group, Pasadena, CA, USA; 3Eye Monitoring Center, Kaiser Permanente Southern California, Baldwin Park, CA, USA; 4Department of Clinical Science, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, USA
Correspondence: Bobeck S Modjtahedi, Eye Monitoring Center, Kaiser Permanente Baldwin Park Medical Center, 1011 Baldwin Park Blvd, Baldwin Park, CA, 91706, USA, Email [email protected]
Purpose: The purpose of this study was to understand individual-, social-, and system-level factors that affect compliance with recommended diabetic retinopathy (DR)-evaluations, and how these factors vary between English and Spanish speakers.
Patients and Methods: We conducted a qualitative study using semi-structured interviews. Study subjects included Kaiser Permanente Southern California members with type II diabetes mellitus at least aged 26 years who spoke English or Spanish. Patients were divided into groups based on their adherence with DR evaluations. Our main outcome measure was the major themes expressed by patients that explained their compliance with DR evaluation.
Results: Fifty-one participants were enrolled: 30 English speakers (11 nonadherent, 19 adherent) and 21 Spanish speakers (8 nonadherent, 13 adherent). Adherent patients were more likely to have had experience with diabetes and identify as being responsible for their own care. Substantially more non-adherent patients suggested that beliefs and attitudes were the reasons people missed retinopathy appointments. More English-speaking participants tended to be self-directed in managing their healthcare, whereas more Spanish speakers relied on others for help. English speakers also noted better relationships with their physicians. Spanish speakers outlined problems with insurance coverage and costs as barriers.
Conclusion: These data suggest two specific intervention strategies that eye care providers could implement to improve adherence with diabetic retinopathy screening and follow up: incorporating a person with DR-related visual loss into the team of staff delivering diabetes support programs and communication campaigns including specific messaging to address fears related to vision loss.
Keywords: diabetes, diabetic retinopathy, screening, adherence, language
Introduction
Diabetes is a major public health concern which affects an estimated 463 million adults, with the North American and Caribbean region having the highest age-adjusted adult prevalence at 12.3%.1 The prevalence of diabetes globally and in the United States has been rapidly increasing.2 The number of patients in the United States with diabetes is anticipated to increase to 47.9 million by 2040 and to exceed 60 million by 2060.3 Diabetic retinopathy (DR) is an important cause of visual morbidity and the leading cause of blindness among working-age American adults.4
Early treatment of DR can reduce the risk of severe vision loss by 94%; however, compliance is poor with only 18–60% of diabetic patients receiving recommended exams.5–7 Most studies of screening non-compliance have utilized quantitative approaches and results frequently have been inconsistent due to differences in methodology.8 Qualitative research approaches may help fill important gaps in our knowledge of DR screening compliance.9 Exploring what themes emerge when patients express their experiences in their own words can open investigators’ perspectives to factors that may have otherwise gone neglected, and allows for better insight into culturally specific factors when performing root cause analysis.8–11
This study sought to characterize factors that influence compliance with recommended DR evaluations among English and Spanish speaking patients.
Research Design and Methods
Study Design and Sample
The study was conducted at Kaiser Permanente Southern California (KPSC), a large, integrated healthcare system that serves more than 4.6 million members. KPSC’s members are diverse and representative of the Southern California population.12 The study cohort was identified through KPSC’s electronic medical record. To be considered eligible patients had to be at least 26 years of age with preferred spoken language of English or Spanish, be diagnosed with type II diabetes at least one year prior to enrollment, and maintain KPSC membership continuously for at least one year. Patients who were unable to consent to medical decision making were excluded. Multistage purposeful sampling strategy was used to select patients for recruitment between November 2017 and December 2018. First, purposeful intensity sampling was used to categorize patients across strata: language (English or Spanish) and adherence to DR evaluation (adherent or non-adherent).13 Adherence to initial DR screening and follow-up appointments following a positive screening result were both considered. Second, patients were randomly sampled from each group for recruitment. Patients were defined as adherent to screening if they had received a retinal screening (fundus photography or clinical exam) in the past two years for those with no history of retinopathy, or the past year for those with a history of retinopathy. Patients were eligible for inclusion in analyses of follow-up care if they received a positive retinal screening result. Patients were defined as adherent to follow-up care if they had an eye exam conducted by an eye care provider within six months of the positive screening.
Recruitment targets were based on the expectation that 10–12 subjects per group would be adequate to achieve thematic saturation.14 Recruitment was stratified by language (English/Spanish) and adherence, resulting in initial estimates of 8 groups and an estimated sample size of 80 (2 languages x 2 types of adherence x 2 adherence status groups). Programmers applied the eligibility criteria and adherence definitions to identify a random sample of eligible members with equal numbers of adherent and non-adherent participants. Bilingual/bicultural team members contacted these individuals by telephone to invite them to participate, and for those interested, administered informed consent by phone. Participants were offered a $20 gift card as compensation. The study was conducted in accordance with the Declaration of Helsinki. The KPSC Institutional Review Board (IRB) approval was obtained for the study and all participants provided informed consent.
Instrument and Data Collection
The interview guide was developed based on the Theory of Planned Behavior and the Social Ecological Model. Participants were interviewed in their preferred language.15,16 Content areas addressed included knowledge and attitudes regarding diabetes and its complications (particularly DR), practical barriers to care, communication with medical providers about diabetes and eye care, patient perceptions of medical center- and system-level barriers or facilitators to screening and follow-up, intentions to engage in recommended diabetic eye care, and social support and norms related to medical care in general and eye care in particular. On average, interviews lasted 45 minutes. Study interviewers digitally recorded all interviews for transcription and analysis.
Data Analysis
A certified vendor translated Spanish interviews into English. The first Spanish transcripts were back-translated to establish accuracy of translation and meanings of cross-cultural concepts.17 For interviews conducted in English, every tenth transcript was compared to the recording to ensure full and accurate transcription. Two trained coders conducted consensus-based thematic analysis of the transcripts, identifying relevant themes and patterns using NVivo 11 for Windows software (QSR International). Each coder independently analyzed three randomly selected interviews, then met with the qualitative research lead to compare and discuss themes. Through three such coding cycles, the coders and qualitative research lead developed the codes to conduct thematic analysis of all interviews. They repeated this process with every fifth interview to ensure consistency in coding. Once all interviews were coded, within-group analysis explored major patterns and relationships between codes to identify themes shared within groups (eg, non-adherent patients). A secondary round of coding was conducted by the qualitative research lead (SH) to identify more specific themes. Cross-group analysis was done to explore major patterns between codes to identify themes that were shared across groups (eg, Spanish-speaking patients).18
Results
Of tens of thousands of eligible patients, 818 were randomly selected for recruitment. Of these, 27 (3.3%) patients were deemed ineligible (eg, patient had died, was no longer a member of the health plan, etc.),116 patients (14.2%) declined participation, 18 (1.9%) agreed to participate but accrual closed before they were enrolled, and 665 patients were never reached (after at least one attempt) before accrual closed. Analysis of initial interviews began while recruitment was still underway, and revealed that the barriers and themes identified for adherence with DR screening and adherence with DR follow-up did not differ; therefore, the two groups of patients were combined, resulting in four categories (2 languages x 2 adherence status groups). The study achieved thematic saturation after 72 patients were interviewed and 51 interviews were transcribed and coded. At this point, recruitment, interviewing, and additional coding stopped.
Of the 51 patients included in these analyses, 30 (58.8%) were male. One participant (1.9%) identified as Asian, 4 (7.8%) Black, 32 (62.7%) Hispanic/Latino, 13 (25.5%) White, and 1 (1.9%) mixed race/ethnicity. Baseline characteristics are listed in Table 1.
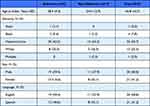 |
Table 1 Participant Characteristics, N=51 |
Knowledge Regarding Diabetic Retinopathy Screening and Results
The large majority of patients (88%) were aware that diabetes can affect the eyes and lead to vision loss; roughly half knew that regular DR screening can help prevent vision loss. A majority (57%) identified vision loss as the complication of diabetes that they most feared. Over one-third (37%) reported that they had learned about diabetic complications by seeing family members and friends experience them:
I have a friend with the kidney [complications] and his eyesight too, he can’t see, and he is younger than me. And my brother is also diabetic right now, he has the kidney [complications]. (non-adherent/Spanish)
This direct experience seeing DR and other complications of diabetes in people they were close to was more commonly reported by adherent patients (44% versus 26% of non-adherent patients) and Spanish speakers (43% versus 33% of English speakers).
Many patients were unfamiliar with the term “diabetic retinopathy,” and only 33% knew how frequently they were supposed to be screened. Three-quarters reported that the health system notifies them when they are due to be screened, and many noted they relied on these reminders. Many more adherent patients were aware of the screening schedule they were recommended to follow (44% versus 16% of non-adherent patients) and reported receiving their results by telephone (25% versus 5%). While most (71%) Spanish speakers reported that results and other information were delivered in Spanish, a few reported that information was provided in English and they did not always understand what their results were.
Relatively few patients in either of the language groups could describe what happens during DR screening or how it differs from other eye exams. One in five confused diabetic retinopathy and DR screening with other eye conditions: “[Diabetes] damages the retina, it can cause you a little bit of glaucoma or cataracts,” adherent/Spanish). Many described procedures for refraction or glaucoma evaluation when asked to explain the details of their last DR screening.
Non-adherent patients frequently cited practical reasons for missing DR screening or follow-up appointments, such as having to travel too far and/or having transportation problems (32%), cost (16%), or not being able to get an appointment at a convenient time (16%). One-quarter stated they had not received a reminder or simply forgot. A substantial proportion – almost all English speakers – did not prioritize the appointment because their visual acuity was good. Others (21%, mostly English speakers) evidenced a fatalistic attitude about their diabetes and their vision: “I don’t know there’s anything I can do now. I mean, those malformed veins in my eyes are there,” (non-adherent/English). Another respondent knew he was doing things that could result in uncontrolled diabetes and DR, and accepted possible complications rather than change his behavior: “This is why I don’t go to the appointments: because if I already know that eating hamburgers hurts me, I know that I am going to get sick,” (non-adherent/Spanish).
Relationship with Physician and Satisfaction with Care
Three-quarters or more of patients in both adherence and both language groups were generally satisfied with their diabetes care, and many offered strong praise for their providers. Adherent patients were more likely than non-adherent patients to report that they feel comfortable enough with their doctor to tell them everything (41% versus 11%); this was an aspect of what patients considered a more engaged and personal relationship with their doctor, and/or because they feel their care provider is exceptionally thorough (eg, “She even called me at home one night just to see how I was doing with it … and I just told her things that I would never tell anybody,” (adherent/English). Spanish speakers were less likely than English speakers tell their doctor everything (14% versus 40%), and were also less likely to note that their doctors do a good job listening to them (43% versus 67%). Those with limited English proficiency reported they preferred and sought out doctors who spoke their native language, although they still tended to be satisfied with non-Spanish speaking primary care providers (PCPs) because they found the interpretation services offered to be sufficient. However, they reported far more communication challenges with eye care providers, who they perceived as less willing or able to use interpretation or translation services. Patients with limited English proficiency often left eye care visits confused and reported waiting until their next appointment with their PCP to seek clarification on their ophthalmic findings and recommendations.
Perceived Self-Control and Self-Discipline
Nearly all patients reported that living with a chronic condition was a challenge related to difficulties with “control,” “discipline,” or “self-discipline.” They described the process of adapting to life with diabetes as a process that requires a high degree of self-discipline. These concepts directly related to their views on DR: the best way to prevent DR, they believed, was by controlling one’s diabetes through diet, weight control, exercise, and medication adherence. Patients viewed attending DR screening and treatment appointments as a specific task among the many that diabetic patients must manage.
Across adherence and language groups, many patients emphasized the importance of self-discipline in determining their success to adhere to DR screening. Non-adherent patients tended to focus on their lack of self-discipline as a barrier to compliance, while some adherent patients identified their strong sense of self-discipline as a driving factor in their ability to follow recommendations. One-quarter of patients expressed the attitude that it was their primary responsibility to be in charge of their diabetes and health (eg, “It’s on you … they just notify you when it’s time to come in and why you should come in, and it’s up to you to go in,” (adherent/English). Adherent patients were more likely to hold these attitudes (31% versus 16%), as were English speakers relative to Spanish speakers (30% versus 19%).
Prioritization and Perceived Risk
Many patients perceived DR screening to be a tedious task similar to other routine tasks necessary in the management of chronic disease. As such, these patients did not attach a sense of urgency to completing their DR screening because they were asymptomatic and felt that diabetic damage to the eye was a gradual process which allowed for delaying ophthalmic care. Patients with visual symptoms were more likely to have their eyes examined.
Competing priorities such as work or caretaking overshadowed preventive health tasks in all patient groups, although non-adherent patients reported greater difficulties prioritizing and utilizing preventive health services. For both language groups, low prioritization of preventive care appeared related to the fact that even advanced DR can be asymptomatic; patients expressed difficulty motivating themselves to come in for evaluation when they were asymptomatic. Spanish speakers were much less likely to identify making one’s DR diagnosis (and health more generally) a priority, with low perceived risk an important barrier for some people: 29% (versus 0 English speakers) said other people may miss DR screening and follow-up appointments for this reason (eg, “I don’t know why other people would not go, it doesn’t make sense … [it’s] because they don’t care about their health,” (adherent/Spanish).
Social Support
Both adherent and non-adherent patients noted the importance of social support in attending appointments, although the theme was more dominant among adherent patients. Informational support was critical for managing information about appointments (such as appointment times), while instrumental support was needed to make and attend appointments (including translation for non-English speaking patients). Social support was particularly important for patients with additional needs, such as those with limited mobility who required assistance with transportation or those with cognitive limitations who needed help keeping track of information.
Economic Factors
Many lower income Spanish- and English-speaking patients reported that their health insurance coverage was unstable, with fluctuations experienced in coverage and health insurance carriers. In these circumstances, these patients report that they could not afford DR screening and follow-up and associated costs: “I don’t go because, the insurance I have right now … the insurance doesn’t cover 100% of everything,” (non-adherent/Spanish).
Patients from both language groups endorsed emotional barriers due to limited financial resources. Some reported being overwhelmed with financial stressors, such as paying rent, which made it practically difficult to manage their health care because their priorities were divided between economic and medical needs. The emotional turmoil surrounding financial challenges further complicated the ability of patients to address their health care needs because they were psychologically drained, and providers were not always aware or sensitive to these challenges. As one patient reported, “They don’t understand much what you feel,” (adherent, Spanish). Another elaborated further:
[My doctor told me], ‘You’re working too much. Why don’t you work less?’ And I told him, I mean, well, if you share your check with me, I don’t mind. (adherent, English)
Discussion
DR is recognized as an important cause of visual morbidity and considerable effort has been extended into improving the low rates of compliance with screening recommendations.19–23 Despite these efforts, compliance with DR screening has not improved over the past decade.24 This study found that adherent patients were more likely to know about diabetic complications including vision loss because of family and friends who had experienced those complications themselves; this immediacy and relevance may have been important in motivating attendance. Non-adherent patients were more likely to cite low perceived risk and lack of symptoms as reasons people with diabetes might miss DR screening appointment, and were more likely to feel a personal responsibility for management of their diabetes. A systematic review published in 2018 identified some attitudes and beliefs that are barriers to DR screening adherence, including anxiety about the screening, but none of the factors that we identified was listed.25 This highlights the importance of taking a qualitative approach to studying DR screening adherence: quantitative measures can ask about known barriers and other factors, but only methodologies that allow for more open-ended explorations can reveal previously unreported barriers. Using a qualitative methodology also does not a guarantee revealing all possible barriers; results can vary based on the types of questions and probes asked. This is reflected by a 2021 review of the qualitative research literature addressing DR screening barriers and adherence that identified some of the broad categories of barriers found in the present study (eg, knowledge regarding DR, communication with providers), but also failed to mention factors such as having family or friends with diabetes-related vision loss.26
While a few previous studies have assessed whether the person with diabetes had family members who also had the disease, we are unaware of previous work examining the target patient’s exposure to diabetic complications through family and friends with diabetes.27 This suggests that interventions could benefit from increasing the salience and relevance of complications (and DR in particular). Future work might also seek to further examine and detail this finding. For example, would experience with other complications enhance DR screening adherence? Some patients in the current study described the members of diabetes education classes as becoming a support group for each other; if such classes were designed to include members with DR and/or other complications, would this improve adherence?
It is important for physicians to view challenges with DR screening compliance as part of the broader difficulties patients face in managing their diabetes care. Non-adherent patients were more likely to report tasks surrounding diabetes care as being overwhelming. Similarly, Liu et al’s qualitative study also discussed the emotional burden some patients felt as they tried to cope with a range of diabetes management tasks.28 Patients perceive DR-related care as another task in a long list of tedious responsibilities which results in patients feeling overwhelmed. As such, attempts to improve DR screening need to fit within the large structure alleviating the burdens patients feel about diabetes care. Lawrenson et al found that interventions targeting DR screening specifically were not significantly more effective than those focused more generally on diabetes care for improving adherence with screening guidelines.29
Linked to this broader context of general diabetes care tasks is the idea of self-control and self-discipline being necessary to successfully manage the litany of those behaviors. Self-discipline was seen by all language groups as necessary for managing retinopathy screening and care, with adherent patients reporting higher self-discipline. Egunsola et al's review documented evidence that among some individuals with diabetes, DR screening adherence is associated with feelings of guilt for not controlling their diabetes better.26 The respondents in Liu et al’s study reported similar themes, labeling themselves as “bad” or “naughty” if they did not complete all the behaviors they felt they should be doing.28 This is consistent with what behavioral economists refer to as present bias, or an overemphasis on benefits in the moment over longer term benefits of behavior. Those who exhibit present bias frequently describe themselves as having limited self-control.30 They are likely to give low priority to behaviors with limited short-term benefit. Many of the patients in this study displayed this aspect of present bias by placing a low priority on DR screening because DR was felt to be a slowly progressive disease and not an imminent danger to their vision. They were not concerned about DR because they were not currently experiencing visual symptoms. Lake et al's study of younger people with diabetes suggested that low perception of DR risk was a barrier to screening for young adults; our study suggests it continues to be a barrier for older adults as well.31 Low perceived risk is a relatively understudied barrier to DR screening adherence, receiving far less attention than than knowledge-related barriers and issues related to cost.27 Yet it is a factor highly amenable to change. Intervention strategies recommended to counter lower perceived risk and other aspects of present bias include reminders, setting goals and devising specific steps to achieve them (eg, behavioral coaching), and offering financial incentives to increase near-term benefits.30 Prompts and cues, as well as goal setting, have been found to be effective strategies to increase adherence to DR screening.29
Previous research has documented the need for improved communication between providers and patients to enhance adherence with DR screening recommendations.26 The current work confirms this and details important differences between the English- and Spanish-speaking groups, which largely lay in the realm of patient education and patient-provider communication: communication barriers were significant for limited English speakers, both for making appointments and for understanding exam results. The current study extends previous findings with additional details about patients’ perceptions regarding the comparatively poor communication they experienced with eye care providers relative to general practitioners. While education (and other measures of socioeconomic status) have also been associated with lower DR screening adherence,32–34 the fact that communication problems were not consistently experienced across all provider types suggests that communication-related adherence issues were likely not related to lower education: Non-English speakers described communication barriers when seeing their eye care providers which were not as pronounced as when they saw their PCPs, and over a quarter reported that results and other important information they received were not always understood because they were delivered in English. Spanish speakers were less likely to state that their doctors do a good job listening to them. Furthermore, while there were some financial barriers noted by some participants in this study, cost-related limits to access were not the principal barrier experienced by this group because all were insured members of Kaiser Permanente. This underscores that there may be uniquely challenging elements to medical translation within eye care services that need to be addressed to help improve the patient experience and increase adherence with DR screening. (For a summary of all major differences identified between the two language groups, see Table 2).
 |
Table 2 Differences Found Between English and Spanish Speakers |
Conclusion
Taken as a whole, these results suggest some practical strategies to improve adherence with DR screening and follow up recommendations (see Table 3 for a summary). The first type of approach involves interventions that provide exposure to individuals with DR-related vision loss; this can be done through diabetes-related support groups or peer navigator programs that many health systems already provide. Both the American Diabetes Association and the American Association of Diabetes Educators have identified the need for provide self-management support – in addition to education – to patients living with diabetes.35 Peer support interventions are effective in achieving clinically significant reductions in HbA1c; peer support provided by nonprofessionals – community health workers, medical assistants, or lay community health workers – can achieve substantial self-management effects.36 Diabetes-related peer support groups can ease the emotional and psychological burdens that people with diabetes frequently experience; participation in these groups can enhance patients’ self-awareness regarding their disease self-management, and may motivate improved self-management to an even greater extent than medical providers can.37–39 The current results suggest that support groups could enhance adherence with DR-related screening and follow-up recommendations by incorporating a team member who has experienced DR-related vision loss; this may be effective in providing exposure and connection to someone who has experienced this complication, and motivate patients’ in their DR-related self-management.
 |
Table 3 Suggested Changes to Routine Eye Care Practice to Enhance DR Screening and Follow-Up Adherence |
The second type of adherence strategy these results suggest involves health communication messages delivered through pamphlets, videos, fotonovelas, or whatever medium is most appropriate for the local population. The current results are consistent with a large body of research demonstrating that people with diabetes strongly fear losing their eyesight.40,41 Simply appealing to this fear and attempting to scare patients into following care recommendations is unlikely to be effective, however: unless people also feel confident that they can do something to prevent losing their eyesight, their response to the fear makes them likely to do the opposite of whatever action is recommended.42 In fact, the fatalism demonstrated by some patients in the current study echoes previous research finding that many patients believe these complications are inevitable, and many overestimate their risk for diabetic complications including blindness.41,43 These fears can inhibit self-management if they are not countered by eye care providers. To address the fear of blindness and the fatalism common among patients with diabetes, as well as our finding that non-adherent patients are likely to see themselves as lacking self-discipline for the difficult tasks of diabetes management, we suggest a communication strategy including three basic messages for patients with diabetes: 1) The bad news: Diabetic retinopathy can cause vision loss and blindness. Even if your vision seems fine, you could have diabetic eye disease and be at risk for future vision loss 2) The good news: There’s something easy you can do to reduce your risk of vision loss! Getting screened for diabetic retinopathy is probably the easiest part of managing your diabetes and can significantly reduce your risk of losing vision. 3) What do you gain? You keep your ability to work, to read, to drive, to play with your grandkids; you keep your independence. Whatever materials are developed to communicate these messages, they should be translated and tailored to different language/cultural groups in order to help overcome the communication barriers identified by non-English speaking patients. These materials could also incorporate photos and text to help patients distinguish DR screening from other types of eye exams.
There are some potential limitations to this study. The study may not be representative of all patients with diabetic retinopathy for several reasons. All participants volunteered to take the time to complete the interview; although the study reached thematic saturation for those interviewed, those who opted not to participate might have had different experiences and opinions. All participants were members of a health care system, and their perspectives may not fully reflect the experiences of uninsured individuals. All lived in Southern California, in largely urban or suburban rather than rural areas. Patients were considered non-adherent if they failed to attend screening visits or if they failed to attend follow-up visits after previously being diagnosed with DR. Although these groups may be expected to face different barriers to adherence, patients who were non-adherent to screening and non-adherent to follow up reported similar experiences in this study. These limitations are mitigated by this study’s relatively large sample size (for a qualitative study) and multi-level and theory driven approach, identifying individual-, social- and system-level factors that may influence the behavior of people with diabetes. Future work can apply this information in the development of comprehensive interventions that effectively target different patient groups.
Interventions aimed at improving patient knowledge of DR are necessary but incompletely address the gaps in diabetes care. Service delivery changes that overcome practical and psychosocial barriers patients face, such as enhanced translation services in eye care settings, after hour clinic availability, and/or enhanced care coordination and outreach may help improve patient compliance with screening.
Funding
This research was funded through a grant from Regeneron, Inc (Tarrytown, New York, USA) (grant number VGFTe-DR-1726).
Disclosure
Dr Bobeck S Modjtahedi reports grants from Genentech and grants from VoxelCloud outside the submitted work. Ms Tiffany Q Luong reports grants from Regeneron, during the conduct of the study, and grants from Allergan plc, outside the submitted work. Dr Donald S Fong reports grants from Regeneron, Inc, during the conduct of the study. The author reports no other conflicts of interest in this work.
References
1. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
2. Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. doi:10.1038/s41598-020-71908-9
3. Lin J, Thompson TJ, Cheng YJ, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr. 2018;16(1):9. doi:10.1186/s12963-018-0166-4
4. Centers for Disease Control and Prevention. The burden of vision loss; 2017. Available from: https://www.cdc.gov/visionhealth/risk/burden.htm.
5. Fathy C, Patel S, Sternberg P
6. Silva PS, Aiello LP. Telemedicine and eye examinations for diabetic retinopathy: a time to maximize real-world outcomes. JAMA Ophthalmol. 2015;133(5):525–526. doi:10.1001/jamaophthalmol.2015.0333
7. Bresnick G, Cuadros JA, Khan M, et al. Adherence to ophthalmology referral, treatment and follow-up after diabetic retinopathy screening in the primary care setting. BMJ Open Diabetes Res Care. 2020;8(1):e001154. doi:10.1136/bmjdrc-2019-001154
8. Hartnett ME, Key IJ, Loyacano NM, Horswell RL, Desalvo KB. Perceived barriers to diabetic eye care: qualitative study of patients and physicians. Arch Ophthalmol. 2005;123(3):387–391. doi:10.1001/archopht.123.3.387
9. Jones RK, Jefferis JM. Is qualitative research under-represented in ophthalmology journals? Eye. 2017;31(8):1117–1119. doi:10.1038/eye.2017.49
10. Anderson RM, Musch DC, Nwankwo RR, et al. Personalized follow-up increases return rate at urban eye disease screening clinics for African Americans with diabetes. Ethn Dis. 2003;13:40–46.
11. Greenhalgh T, Helman C, Chowdhury AM. Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. BMJ. 1998;316(7136):978–983. doi:10.1136/bmj.316.7136.978
12. Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37–41. doi:10.7812/tpp/12-031
13. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–544. doi:10.1007/s10488-013-0528-y
14. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. doi:10.1177/1525822X05279903
15. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
16. Moos R. Evaluating Treatment Environments: A Social Ecological Approach. New York, NY: Wiley-Interscience Series; 1974.
17. Lopez GI, Figueroa M, Connor SE, Maliski SL. Translation barriers in conducting qualitative research with Spanish speakers. Qual Health Res. 2008;18(12):1729–1737. doi:10.1177/1049732308325857
18. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook.
19. Maclennan PA, McGwin G
20. Paz SH, Varma R, Klein R, Wu J, Azen SP; Los Angeles Latino Eye Study G. Noncompliance with vision care guidelines in Latinos with type 2 diabetes mellitus: the Los Angeles Latino Eye Study. Ophthalmology. 2006;113(8):1372–1377. doi:10.1016/j.ophtha.2006.04.018
21. Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines. Ophthalmology. 2001;108(3):563–571. doi:10.1016/s0161-6420(00)00600-x
22. Bastos de Carvalho A, Ware SL, Lei F, Bush HM, Sprang R, Higgins EB. Implementation and sustainment of a statewide telemedicine diabetic retinopathy screening network for federally designated safety-net clinics. PLos One. 2020;15(11):e0241767. doi:10.1371/journal.pone.0241767
23. Liu J, Gibson E, Ramchal S, et al. Diabetic retinopathy screening with automated retinal image analysis in a primary care setting improves adherence to ophthalmic care. Ophthalmol Retina. 2021;5(1):71–77. doi:10.1016/j.oret.2020.06.016
24. Eppley SE, Mansberger SL, Ramanathan S, Lowry EA. Characteristics associated with adherence to annual dilated eye examinations among US patients with diagnosed diabetes. Ophthalmology. 2019;126(11):1492–1499. doi:10.1016/j.ophtha.2019.05.033
25. Kashim RM, Newton P, Ojo O. Diabetic retinopathy screening: a systematic review on patients’ non-attendance. Int J Environ Res Public Health. 2018;15(1):157. doi:10.3390/ijerph15010157
26. Egunsola O, Dowsett LE, Diaz R, Brent MH, Rac V, Clement FM. Diabetic retinopathy screening: a systematic review of qualitative literature. Can J Diabetes. 2021;45(8):725–733.e12. doi:10.1016/j.jcjd.2021.01.014
27. Piyasena M, Murthy GVS, Yip JLY, et al. Systematic review on barriers and enablers for access to diabetic retinopathy screening services in different income settings. PLos One. 2019;14(4):e0198979. doi:10.1371/journal.pone.0198979
28. Liu Y, Zupan NJ, Shiyanbola OO, et al. Factors influencing patient adherence with diabetic eye screening in rural communities: a qualitative study. PLos One. 2018;13(11):e0206742. doi:10.1371/journal.pone.0206742
29. Lawrenson JG, Graham-Rowe E, Lorencatto F, et al. Interventions to increase attendance for diabetic retinopathy screening. Cochrane Database Syst Rev. 2018;1:CD012054. doi:10.1002/14651858.CD012054.pub2
30. Williams AM, Liu PJ, Muir KW, Waxman EL. Behavioral economics and diabetic eye exams. Prev Med. 2018;112:76–87. doi:10.1016/j.ypmed.2018.04.006
31. Lake AJ, Rees G, Clinical SJ. Psychosocial factors influencing retinal screening uptake among young adults with type 2 diabetes. Curr Diab Rep. 2018;18(7):41. doi:10.1007/s11892-018-1007-3
32. Thomas CG, Channa R, Prichett L, Liu TYA, Abramoff MD, Wolf RM. Racial/ethnic disparities and barriers to diabetic retinopathy screening in youths. JAMA Ophthalmol. 2021;139(7):791–795. doi:10.1001/jamaophthalmol.2021.1551
33. Kelly SR, Loiselle AR, Pandey R, et al. Factors associated with non-attendance in the Irish national diabetic retinopathy screening programme (INDEAR study report no. 2). Acta Diabetol. 2021;58(5):643–650. doi:10.1007/s00592-021-01671-4
34. Knight A, Lindfield R. The relationship between socio-economic status and access to eye health services in the UK: a systematic review. Public Health. 2015;129(2):94–102. doi:10.1016/j.puhe.2014.10.011
35. Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. Diabetes Care. 2017;40(10):1409–1419. doi:10.2337/dci17-0025
36. Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ. 2007;33(6):
37. Due-Christensen M, Zoffmann V, Hommel E, Lau M. Can sharing experiences in groups reduce the burden of living with diabetes, regardless of glycaemic control? Diabet Med. 2012;29(2):251–256. doi:10.1111/j.1464-5491.2011.03521.x
38. Heisler M. Overview of peer support models to improve diabetes self-management and clinical outcomes. Diabetes Spectr. 2007;20(4):214–221. doi:10.2337/diaspect.20.4.214
39. Skinner TC, Van der Ven N. Psychological group interventions in diabetes care. In: Snoek FJ, Skinner TC, editors. Psychology in Diabetes Care.
40. Heuer L, Lausch C. Living with diabetes: perceptions of Hispanic migrant farmworkers. J Community Health Nurs. 2006;23(1):49–64. doi:10.1207/s15327655jchn2301_5
41. Quandt SA, Reynolds T, Chapman C, et al. Older adults’ fears about diabetes: using common sense models of disease to understand fear origins and implications for self-management. J Appl Gerontol. 2013;32(7):783–803. doi:10.1177/0733464811435506
42. Witte K. Fear as motivator, fear as inhibitor. In: Andersen PA, Guerrero LK, editors. Handbook of Communication and Emotion. Academic Press; 1996:423–450.
43. Kuniss N, Freyer M, Muller N, Kielstein V, Muller UA. Expectations and fear of diabetes-related long-term complications in people with type 2 diabetes at primary care level. Acta Diabetol. 2019;56(1):33–38. doi:10.1007/s00592-018-1217-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
