Back to Journals » Patient Preference and Adherence » Volume 17
Exploring Motivations Regarding Dietary Intake Intentions in Gestational Diabetes Mellitus: Development and Validation of a Questionnaire
Authors Di J , Zhu Q, Wu L, Tan J, Gao Y, Liu J
Received 7 August 2023
Accepted for publication 31 October 2023
Published 14 November 2023 Volume 2023:17 Pages 2939—2948
DOI https://doi.org/10.2147/PPA.S434348
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Jiajin Di,1 Qingxian Zhu,2 Lei Wu,2 Jiali Tan,2 Yi Gao,1 Jun Liu2
1Wuxi Medical College, Jiangnan University, Wuxi, Jiangsu, People’s Republic of China; 2The Affiliated Maternity and Child Health Hospital of Jiangnan University, Wuxi, Jiangsu, People’s Republic of China
Correspondence: Jun Liu, The Affiliated Maternity and Child Health Hospital of Jiangnan University, No. 48, Samuel Lane, Liangxi District, Wuxi, Jiangsu, People’s Republic of China, Tel +86 180 6836 0717, Email [email protected]
Purpose: The maintenance of stable blood glucose levels in gestational diabetes patients depends on their ability to make scientific decisions. Decision-making ability is influenced by factors such as preferences, knowledge acquisition, and risk perceptions. At present, problems such as irrational dietary structure, difficulties in decision-making, and poor adherence still exist in clinical practice. The key to guiding gestational diabetes patients in developing their scientific decision-making abilities lies in identifying the weak key points that affect their decision-making abilities. There is a lack of validated tools to assess these patients’ perceptions of dietary intake. In this study, we aimed to develop and validate the Dietary Intake Perceived Motivation Questionnaire for Patients with Gestational Diabetes Mellitus with the purpose of accurately identifying the obstacles encountered by gestational diabetes mellitus patients in the development of their scientific decision-making abilities.
Patients and Methods: In this study, 304 individuals with gestational diabetes were recruited from a public hospital in Wuxi, China. The questionnaire was developed in 3 stages, consisting of questionnaire development, a pilot study, and a formal test, and the validity and reliability of the questionnaire were tested and confirmed. The content validity index and exploratory factor analysis were completed by expert correspondence to indicate the validity of the content and structure. In addition, Cronbach’s α was used to evaluate the internal consistency of each item of the questionnaire, and Spearman-Brown analysis was used to analyze the split-half reliability. In addition to the questionnaire, the study participants were asked to complete a general information questionnaire that included items on various demographic factors such as age, week of gestation, and mode of conception.
Results: The questionnaire was validated through principal component analysis, resulting in a 31-item questionnaire named the Dietary Intake Perceived Motivation Questionnaire for Patients with Gestational Diabetes Mellitus. This questionnaire explained 86.267% of the variance and demonstrated good internal consistency (Cronbach’s α= 0.929).
Conclusion: Our study determined that the questionnaire serves as a valuable tool in evaluating the motivation behind dietary intake in gestational diabetes patients.
Keywords: questionnaire, gestational diabetes, pregnancy, validation
Introduction
Gestational diabetes mellitus (GDM) is defined as carbohydrate intolerance resulting in hyperglycemia of varying severity with onset or first recognition during pregnancy.1 According to the International Diabetes Federation, GDM occurs in approximately 14% of pregnant women globally.2 The latest systematic review and meta-analysis showed that the pooled prevalence of GDM in mainland China was 14.8%.3 GDM patients are at a higher risk of developing metabolic syndrome within three months after delivery. The likelihood of GDM recurrence during subsequent pregnancy ranges from 30% to 84%.4 In the long term, the risk of type 2 diabetes among GDM patients is almost ten times higher than that among pregnant women without GDM.5 Additionally, the risk of metabolic diseases such as overweight/obesity, hypertension, and T2DM in adolescence is significantly higher among offspring of GDM patients.6,7 According to research, GDM patients in China spend an average of $915 on treatment, which is 1.95 times higher than the cost per person among pregnant women without GDM. Due to the high prevalence, severe complications, and heavy economic burden associated with GDM, it has become a subject of continuous attention in recent years in China.
According to the latest guidelines in China, GDM patients with type A1 can ideally manage their blood sugar levels through nutrition management and exercise guidance.8 Among these factors, diet serves as the foundation and energy source for the body to carry out all life activities and directly affects blood glucose fluctuations in GDM patients. Previous studies have shown that diet has an important influence on the incidence of GDM, and a reasonable diet can effectively prevent the development of GDM.9
Numerous studies have demonstrated that GDM patients exhibit irrational dietary intake behaviors.10–12 These behaviors include poor adherence to carbohydrate intake, an unreasonable dietary composition, a low awareness of dietary types and intake, and susceptibility to various factors, such as insufficient knowledge of GDM, inadequate disease awareness, a lack of active control, passive eating attitudes, and inadequate family support. The increased likelihood of adverse pregnancy outcomes in GDM patients and the resulting financial burden on families highlight the need for a deeper understanding of the factors that influence these patients’ dietary intake decisions. This understanding can help health care professionals provide tailored care that meets the unique needs of GDM patients.
Research on GDM primarily focuses on dietary intake patterns and behavior but neglects the decision-making behaviors and influencing factors involved in the dietary intake process.13,14 Decision-making behavior refers to the process in which patients evaluate advantages and disadvantages, taking into account their personal preferences, values, and cognitive factors, when making health-related decisions.15 Currently, there is a significant amount of research on the behavioral decision-making abilities of Chinese individuals in the fields of education and sociology. However, there has been limited discussion on this topic in the medical field, and research in this area has only recently begun.16,17 Decision-making behavior among GDM patients is a complex process that is influenced by various factors related to individual psychology and physiology. Accurately assessing GDM patients’ decision-making behaviors, understanding their motivations, and identifying the factors that affect changes in their motivation are crucial. Therefore, it is important to select an appropriate tool for assessment.
This study delved into the topic extensively by utilizing protection motivation theory (Figure 1) within the realm of social psychology.18 The theory was employed to examine the process of individual behavior changes, specifically focusing on motivation factors that can aid in analyzing and predicting patient decision-making behaviors.
 |
Figure 1 Protection Motivation Theoretical Framework. |
To effectively assess influencing factors in GDM, it is imperative to utilize a valid and reliable tool. However, our search revealed a limited number of validated assessment tools that meet these criteria. Huang developed a questionnaire to assess the decision-making behaviors of GDM patients regarding blood glucose management.19 The reliability and validity of the questionnaire were tested, but the questionnaire primarily focused on the overall blood glucose control of GDM patients and did not specifically address dietary decision-making. As a result, the questionnaire did not provide the necessary information on the dietary habits of GDM patients.
At present, comprehensive and validated tools for measuring decision-making behavior in GDM patients are lacking. To identify factors that influence dietary decision-making in GDM patients and to guide future research on patient-centered decision-making interventions, we developed a questionnaire. Additionally, we sought input from experienced nutritionists to ensure that the questionnaire was well informed and effective.
Materials and Methods
Participants and Recruitment
In this study, 304 GDM patients visiting the outpatient and inpatient departments of the obstetrics department of a hospital in Wuxi, China, from March 2023 to August 2023 were invited to participate (the number of subjects to be recruited for ethical review was approximately 340). After obtaining informed consent from the GDM patients, they were invited to complete the questionnaire at the hospital, which was distributed in person on site, and the purpose of the survey was explained to the patient and the confidentiality of the questionnaire responses was assured. The inclusion criteria were as follows:
The exclusion criteria were as follows:
A retest phase of questionnaire validation was not performed in this study due to changes in patient decision-making behavior over time.
Setting
The study was conducted in the Wuxi region of China, where the diet is mainly composed of refined foods with a preference for sweeter options. Limited nutritional knowledge and poor eating habits in the region have been identified as factors that negatively impact the dietary intake of GDM patients and are significantly associated with adverse pregnancy outcomes such as GDM.
Ethical Considerations
Research ethics approval for this study was obtained from the Ethics Committee of Wuxi Medical College of Jiangnan University under approval number JNU20230301IRB18. Informed consent was obtained from each subject prior to enrollment. All women who agreed to participate in the study provided their data voluntarily and could withdraw from the study at any time.
Procedure
Phase 1: Questionnaire Development
The task force executed a series of steps, including identifying research questions and objectives, defining the inclusion and exclusion criteria, searching the literature, integrating or synthesizing the findings, and extracting data from included studies. A literature review on the diets of GDM patients was conducted by searching Chinese and English databases such as CNKI, Wanfang, PubMed and CHINAL. A research team was then established, comprising a senior medical doctor with expertise in pregnancy endocrinology research, three diabetes specialist nurses with more than 10 years of experience in pregnancy endocrinology and obstetrics, a nutritionist, a psychologist, and a postgraduate tutor. The questionnaire dimensions were determined based on the 7 major factors of Protective Motivation Theory and designed with reference to the sentence structure of similar questionnaires for other diseases. The aim was to analyze and predict glycemic management behavior.
During the preliminary phase, the research team formulated and refined 35 potential projects. In January and February 2023, experts received invitations via email to review the questionnaire items and provide feedback. The inclusion criteria for experts in this research were as follows: individuals engaged in GDM-related medical, nursing, and educational work, with more than 10 years of work experience; those who held a bachelor’s degree or above and an associate senior title or above; and those who volunteered to participate in the study. The content, relevance, and clarity of the questionnaire were assessed by a panel of experts. To ensure content validity, a Likert-type scale ranging from 1 to 5 was utilized, with a score of 1 indicating very little importance and a score of 5 indicating very high importance. The content validity index (CVI) was calculated, with scores greater than 0.80 being considered acceptable Ultimately, a total of 31 items were selected for the study.
Phase 2: Pilot Sample
The questionnaire was reviewed by a panel of experts and tested in early March 2023 in 30 GDM patients who were later excluded from the final study sample. The researchers collected the data in the maternity ward and explained the purpose and content of the questionnaire to the respondents before they were asked to rate their degree of conformity with each item. The questionnaire was then completed and returned on site. After completion of the pilot testing phase, the language used in the questionnaire was further refined by modifying the items that were not clearly expressed.
Phase 3: Formal Test
The assessment questionnaire used in this study consisted of 31 items and was administered to a sample of GDM patients who were receiving care at a tertiary Grade A obstetrics and gynecology hospital in Wuxi, China. The sample size was estimated to be 5–10 times the number of questionnaire items, and 8 times the number of questionnaire items were ultimately selected. Considering a potential loss-to-follow-up rate of 20%, a sample size of 297 GDM patients was recommended. A total of 304 questionnaires were distributed in this study, and 304 valid questionnaires were recovered, with a valid recovery rate of 100%.
The study utilized the General Information Questionnaire and the Dietary Intake Perceived Motivation Questionnaire for GDM Patients to gather data. The General Information Questionnaire consisted of items regarding various demographic factors, such as age, gestational week, method of conception, family per capita monthly income, education level, GDM history, family history of diabetes, employment status, fasting blood glucose levels during glucose tolerance tests, and 2-hour postprandial blood glucose levels. The questionnaire used to assess dietary intake protection motivation in GDM patients contains two parts: a threat assessment (which includes four dimensions: susceptibility, severity, internal reward, and external reward) and coping assessment (which includes three dimensions: response efficacy, self-efficacy, and response cost). In total, there are 31 items in the questionnaire. Each item is scored using a 5-point Likert-type scale ranging from “strongly disagree” to “strongly agree”. Each dimension is scored separately, and the higher the scores of the four dimensions (susceptibility, severity, response efficacy, and self-efficacy) are, the stronger the protective motivation; the lower the scores of the three dimensions (internal reward, external reward, and response cost) are, the stronger the protective motivation.
Data Analysis
Excel 2019 was used to enter relevant data, and SPSS 26.0 was used to analyze the data. First, a descriptive analysis was carried out on the sociodemographic variables of the participants: enumeration data are described by the number of patients and percentages; and measurement data with a normal distribution are expressed by the mean ± standard deviation.
For the screening and evaluation of questionnaire items, the item analysis method was adopted, including the correlation coefficient method and critical ratio method. In terms of reliability analysis, Cronbach’s α coefficient was used to evaluate the internal consistency of the items in the questionnaire, and acceptable values were considered to be higher than 0.70; the split-half reliability was determined by Spearman-Brown split-half reliability, and the test level was α=0.05.
In terms of validity analysis, content validity and construct validity were evaluated. For the content validity analysis, the expert evaluation method was adopted to calculate the content validity index at the questionnaire level and the item level; in the structural validity analysis, the principal component analysis and the variance maximization orthogonal rotation method were used, according to a characteristic root ≥1. The number of common factors retained was determined by the decrease in factor variation in the gravel map, and the variance contribution rate of the common factors to the original index and the loading of each item on the common factor were determined. Items with a loading value of the common factor >0.4 were retained, and the absolute value of the load difference was <0.2.20
Results
Sociodemographic Characteristics of the Sample
The age of the 304 GDM patients ranged from 22–44 (31.276±4.035) years old; the gestational age ranged from 24–41 (36.245±4.261) weeks; 286 patients (94.08%) had naturally conceived, and 18 (5.92%) conceived by assisted reproduction; 7 patients (2.30%) had a monthly income of ≤3000 yuan, 84 patients (27.63%) had a monthly income of 3000–5000 yuan, and 213 patients (70.07%) had a monthly income of ≥5000 yuan; 61 patients (20.07%) had an education level of high school and below, 80 patients (26.32%) had an education level of junior college, 150 patients (49.34%) had an undergraduate education, and 13 patients (4.28%) had a postgraduate education and above; 47 patients (15.46%) had a history of gestational diabetes; 232 patients (76.32%) were employed, and 72 patients (23.68%) were unemployed; 280 patients (92.11%) were covered by medical insurance, and 24 patients (7.89%) were self-financed; 231 patients (75.99%) had recorded food diaries; and 19 patients (6.25%) underwent insulin therapy, with a fasting blood glucose level ranging from 3.85–8.21 (5.053±0.681) mmol/l.
Result of Expert Inquiry
In this study, two rounds of expert consultation were conducted, and the return rate of the questionnaires was 100%. Experts added or deleted questionnaire items and modified the expression of some items according to their opinions. For example, the items “If you do not increase your weight reasonably during pregnancy, your blood glucose will be poorly controlled” and “My family wants me to eat as much as possible during pregnancy” were deleted. The following items were modified: “Eating my favorite food during pregnancy will make me feel happy” was changed to “During pregnancy, following my usual eating habits (such as reducing the intake of carbohydrates) will make me feel very happy”; “Frequently held health lectures are conducive to the management of dietary intake behavior of luck” was changed to “Various forms of knowledge acquisition channels are helpful”; “It is conducive to the management of dietary intake behavior during pregnancy”, “I am confident that I will consume enough energy during pregnancy according to the recommendations of medical personnel” and “I am confident that I will consume nutrient-rich foods during pregnancy according to the recommendations of medical personnel”. In the first round of expert consultation, except for the deleted items, the importance scores of the other items ranged from 3.00 to 5.00, and the coefficient of variation ranged from 0.09 to 0.23. The importance scores of each item in the second round of expert correspondence ranged from 4.00–5.00, and the coefficient of variation ranged from 0.00–0.12. The results are shown in Table 1.
 |
Table 1 Questionnaire Importance Score and Coefficients of Variation |
Pretest Results
According to the feedback from GDM patients, it took approximately 5–10 minutes to complete each questionnaire. The patients agreed that the statement of the scale items, except for the double negative of the “susceptibility” item, was clear and easy to understand. However, since “susceptibility” examines the perception of research subjects regarding adverse outcomes, the presentation of the items was not modified.
Validity Analysis
Project Analysis
According to the results of the critical ratio method, the differences between the items in the high group and the low group were statistically significant (P<0.01); the correlation coefficient method also showed that the items in the study were significantly correlated with the total score of the scale, and the correlation coefficient ranged from 0.364–0.782 (P<0.01). It showed that the 31 items had good distinction and should be reserved.
Content Validity
The total content validity index of the dietary intake perceived motivation questionnaire for patients with GDM was 0.903, and the content validity index of each item ranged from 0.857–1.000.
Construct Validity: Exploratory Factor Analysis
The χ2 value of Bartlett’s sphericity test was 5203.422, reaching the significance test level (P<0.01), and the KMO value was 0.909, indicating that this study was suitable for factor analysis. The analysis results show that there were 7 common factors with eigenvalues > 1, and the cumulative variance contribution rate was 86.267%. Combined with the gravel map (Figure 2), it was found that after the seventh common factor, the slope gradually became flat. Therefore, 7 common factors were extracted. This showed that the questionnaire has good construct validity. At the same time, the questionnaire structure obtained by exploratory factor analysis was basically consistent with the theoretical framework. Among the items, the loading value of entry A4 “Adding foods containing vitamins and minerals without a plan will cause nutritional imbalance” on the two common factors (Factor 5 and Factor 6) was >0.4, and the absolute value of the difference between the loads was >0.2. The research group opinion was that this item should not be deleted.
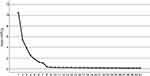 |
Figure 2 Scree plot of the factor analysis. |
Trust Level Analysis
The Cronbach’s α coefficient of the total questionnaire was 0.929, and the Cronbach’s α coefficient of each dimension ranged from 0.913–0.958, indicating that the scale has good internal consistency reliability; the half-time reliability of the total questionnaire is 0.809, and the split-half reliability of each dimension ranged from 0.914–0.958.
Discussion and Conclusions
Discussion
Despite the advancement of the concept of precision glucose management in China today, hospitals are still unable to implement it and GDM patients are unable to acquire knowledge about it.21 This is similar to the findings of a semistructured interview study, in which most GDM patients faced a conflict between dietary control and nutritional needs, and the inability to consume adequate amounts of carbohydrates had become a major problem for them; however, most of the information provided by existing health care professionals advocated for the intake of adequate amounts of carbohydrates, which added many barriers to the management process for health care professionals. In addition, many health care decision-makers lack adequate decision-making skills, resulting in GDM patients mostly having little knowledge about diet.22 Therefore, accurate identification of GDM patients with weak decision-making skills and reinforcement is urgently needed.
Despite an extensive search, studies assessing motivation regarding dietary intake in individuals with GDM were difficult to find. The few available studies mainly involved qualitative interviews rather than questionnaire-based research.14,15 It is not possible to conduct detailed qualitative interviews with each individual in clinical practice, making simple questionnaires the most convenient and quickest method available. This is in high agreement with Ying’s findings.23 The purpose of this study was to develop and validate a questionnaire suitable for the analysis of barriers to meal choices in GDM patients—The Dietary Intake Perceived Motivation Questionnaire for Patients with Gestational Diabetes Mellitus. The results showed that this questionnaire is a reliable and valid method for assessing GDM patients’ reasons for making dietary decisions, and it showed good validity and reliability overall. The overall Cronbach’s α coefficient (correlation coefficient 0.929) was satisfactory, and the Cronbach’s α values for each domain ranged from 0.913–0.958. This is consistent with the expected results, as internal reliability values ≥0.7 are generally considered satisfactory.
First, the development of this questionnaire was based on a number of questionnaires described in previously published journal papers that can be used to assess the glucose management decisions of GDM patients. Some of these questionnaires have been well validated, so many of their statements have been recognized in several studies. The questionnaire statements were also developed with reference to well-established theories and GDM-specific dietary patterns to ensure that the questionnaire would be a valid tool for targeting the motivation regarding dietary intake in GDM patients. Third, the draft questionnaire was discussed and created by experts with great expertise. Thus, their knowledge and experience were perfectly integrated in the discussion and selection of the questionnaire statements. In other words, this questionnaire can reliably measure the facilitators and barriers that may arise for GDM patients when making scientific decisions regarding dietary choices.
The cross-sectional nature of the study design was a limitation of the current study. While our study did not examine the relationship between decision-making and disease duration in GDM patients, it is important to note that decision-making is a type of executive cognitive function that may manifest differently at different stages of the disease. To better understand the decision-making abilities of GDM patients during pregnancy and postpartum, longitudinal studies are necessary to document developmental trajectories and psychosocial correlates.
Conclusion
Our study demonstrated that the Dietary Intake Perceived Motivation Questionnaire for Patients with Gestational Diabetes Mellitus is a psychometrically reliable and valid instrument for comprehensively assessing the critical and ancillary factors that emerge when GDM patients make decisions about dietary intake. Specifically, GDM patients’ perceived knowledge of the disease and perceived severity of the disease should be measured to indicate their level of understanding of the disease; external and self-influences on dietary choices should be measured to reflect their individual self-selectivity; self-efficacy and response efficacy should be measured to indicate their subjectivity regarding the event after it occurs; and their perceptions of the cost of the event should be measured to indicate their acceptance.
Acknowledgments
We are grateful to the individuals who took the time to participate in this study. We would like to thank the “Postgraduate Research & Practice Innovation Program of Jiangsu Province (Project Approval Number: SJCX23_1246)” for their support and assistance in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Freinkel N, Metzger BE, Phelps RL, et al. Gestational diabetes mellitus. Heterogeneity of maternal age, weight, insulin secretion, HLA antigens, and islet cell antibodies and the impact of maternal metabolism on pancreatic B-cell and somatic development in the offspring. Diabetes. 1985;34(2):1–7. PMID: 3888733. doi:10.2337/diab.34.2.s1
2. International Diabetes Federation. IDF diabetes atlas. Brussels, Belgium; 2021. Available from: https://www.diabetesatlas.org.
3. Gao C, Sun X, Lu L, et al. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis. J Diabetes Investig. 2019;10(1):154–162. PMID: 29683557; PMCID: PMC6319492. doi:10.1111/jdi.12854
4. Geng S, Congying X, Huixia Y. Prediction and prevention of recurrent pregnancy-induced diabetes mellitus. Chin J Pract Inter Med. 2018;38(06):538–540. doi:10.19538/j.nk2018060112
5. Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi:10.1136/bmj.m1361
6. Liang Z, Liu H, Wang L, et al. Maternal gestational diabetes mellitus modifies the relationship between genetically determined body mass index during pregnancy and childhood obesity. Mayo Clin Proc. 2020;95(9):1877–1887. PMID: 32861332; PMCID: PMC7672776. doi:10.1016/j.mayocp.2020.04.042
7. Lu J, Zhang S, Li W, et al. Maternal gestational diabetes is associated with offspring’s hypertension. Am J Hypertens. 2019;32(4):335–342. PMID: 30624576; PMCID: PMC6420681. doi:10.1093/ajh/hpz005
8. Chinese Medical Association Obstetrics and Gynecology Branch Obstetrics Group, Chinese Medical Association Perinatal Medicine Branch, Chinese Maternal and Child Health Association Pregnancy Complicated Diabetes Professional Committee. Guidelines for Diagnosis and Treatment of Hyperglycemia in Pregnancy (2022) [Part I]. Chin Obstet Gynecol Magaz. 2022;57(1):3–12. doi:10.3760/cma.j.cn112141-20210917-00528
9. Ying W, Hua B, Fengzhi Z, et al. Research progress on high-risk factors and preventive measures of gestational diabetes mellitus. Mod Prevent Med. 2020;47(01):156–159.
10. Phan L, Kubota J, Pignotti GAP. Carbohydrate knowledge observed to be low in Vietnamese women with gestational diabetes mellitus. J Nutr Educ Behav. 2022;54(6):551–556. PMID: 35305897. doi:10.1016/j.jneb.2021.12.007
11. Pengtu Z. Diet Analysis and Nutrition Therapy Effect Research on Overweight and Obese Patients with Gestational Diabetes Mellitus Before Pregnancy. Qingdao University; 2021.
12. Smyth S, Mulligan K, Rutter E, et al. Attitudes of women with gestational diabetes toward diet and exercise: a qualitative study. J Matern Fetal Neonatal Med. 2023;36(1):2155045. PMID: 36599434. doi:10.1080/14767058.2022.2155045
13. Qiushuang Z, Yuanjie D, Yucun N. Dietary pattern and serum metabolomics analysis of gestational diabetes mellitus. J Harbin Med Univer. 2021;55(06):666–670.
14. Yaping S. Analysis of Current Situation and Influencing Factors of Self-Management of Patients with Gestational Diabetes Mellitus During Pregnancy. Peking Union Medical College; 2018.
15. Pierce PF, Hicks FD. Patient decision-making behavior: an emerging paradigm for nursing science. Nurs Res. 2001;50(5):267–274. PMID: 11570711. doi:10.1097/00006199-200109000-00003
16. Na H, Yingfeng Z, Li L, et al. Study on decision-making behavior and influencing factors of blood glucose management in pregnant women with gestational diabetes mellitus. Chin J Nurs. 2021;56(09):1312–1317.
17. Yingfeng Z, Na H, Li L, et al. A qualitative study on the decision-making dilemma of blood glucose management in pregnant women with gestational diabetes mellitus. PLA J Nurs. 2022;39(01):9–12.
18. Rogers RW, Prentice-Dunn S. Protection Motivation Theory. Plenum Press; 1997.
19. Na H, Yingfeng Z, Li L, et al. Development and reliability and validity of a questionnaire on the protection motivation of blood sugar management in pregnant women with gestational diabetes mellitus. Chin J Nurs. 2021;56(04):561–566.
20. Wu ML. Questionnaire Statistical Analysis Practice: Operation and Application of SPSS. Chongqing: Chongqing University Press; 2010.
21. Qin G, Yingqian X, Yiqing Z, et al. Analysis of the effects of one-day outpatient dietary individualized guidance on glycemic control, body mass gain and pregnancy outcome in pregnant women with gestational diabetes mellitus. J Shanghai Jiao Tong Univer. 2022;42(02):185–191.
22. Zhang X, Yin W, Qiaoyan L, et al. A longitudinal qualitative study of glucose management decision-making experiences in patients with gestational diabetes mellitus. J Nurs. 2023;30(12):22–26. doi:10.16460/j.issn1008-9969.2023.12.022
23. Ying F, Caihong Z, Liping M, et al. Development of a questionnaire on health education needs of gestational diabetes mellitus patients based on the Delphi method and test of reliability and validity. Chin J Rep Health. 2022;33(06):544–549.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
