Back to Journals » Clinical and Experimental Gastroenterology » Volume 15
Experience of Telemedicine in Gastroenterology Out-Patient Practice During the COVID-19 Pandemic: Experiences from a Tertiary-Care Hospital in a Developing Country
Authors Shaikh A, Khan M, Ismail FW
Received 11 February 2022
Accepted for publication 6 June 2022
Published 17 June 2022 Volume 2022:15 Pages 91—99
DOI https://doi.org/10.2147/CEG.S361381
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wing-Kin Syn
Anjiya Shaikh,1,* Maria Khan,2,* Faisal Waseem Ismail3
1Department of Medicine, University of Connecticut School of Medicine, Farmington, CT, USA; 2Department of Medicine, Aga Khan University, Karachi, Sindh, Pakistan; 3Section of Gastroenterology, Department of Medicine, Aga Khan University, Karachi, Sindh, Pakistan
*These authors contributed equally to this work
Correspondence: Faisal Waseem Ismail, Department of Medicine, Aga Khan University, Karachi, Sindh, Pakistan, Tel +92-3009214175, Email [email protected]
Objective: Telemedicine is being widely implemented in the COVID-19 pandemic to avoid infection risk. However, its effectiveness has not been evaluated, especially in developing countries, where it is invaluable for healthcare access. This study assesses physicians’ and patients’ perspectives of the usefulness and challenges of telemedicine in the gastroenterology department to identify its pitfalls.
Methods: A cross-sectional telephonic survey was conducted on patients presenting to the gastroenterology department at a tertiary care hospital in Pakistan. An online survey was sent to physicians in the department.
Results: A total of 160 patients participated, with a mean age 49.8 years, and 42.8% (n=68) males. There were 23.8% (n=38) initial visits and 76.3% (n=122) follow-ups. More than 85% of patients agreed telemedicine saved cost and time, 46.5% (n=74) said it improved healthcare access, and 76.3% (n=122) wanted to use it again. More than 80% were satisfied with the physician-patient interaction. Of the 7 physicians who participated, most felt telemedicine was inadequately facilitated, but felt comfortable with technology. Most felt it did not negatively affect healthcare, but thought it was complex for patients and that lack of physical interaction is a limitation. Nearly half were in favor of continuing its use after the pandemic.
Conclusion: Telemedicine is an effective alternative to in-person visits. Patients find it convenient, with adequate interaction. Physicians have reservations that need addressal, such as poor administration. Most patients and half of physicians are welcome to using telemedicine in the post-COVID era.
Keywords: telemedicine, gastroenterology, teleconsultation
Introduction
The emergence of the COVID-19 (SARS-CoV-2 coronavirus variant) pandemic has led to a sudden change in healthcare delivery. Governments across the globe have taken drastic measures to reduce the rate of transmission of Sars-Cov-2 and protect the population. Social distancing requirements have led hospitals to call for deferral of all non-essential in-person clinic encounters, suspension of elective procedures, and a reduction in hospital-wide staffing. Patients themselves are also very hesitant and afraid to seek even urgent care as hospitals are considered very high-risk areas.
These recent events have therefore caused an immediate need to implement telemedicine. Telemedicine is a broad term defined as distant healthcare delivery, where technology is used to support long-distance clinical care and healthcare education and administration, without the need for physical interaction.1 Common modalities include physician consultations virtually on simple calls, emails or live video teleconferencing as well as remote patient monitoring and mobile health applications.2 Telemedicine has allowed continuity of healthcare delivery while reducing the risk of Sars-cov19 transmission, preventing physical interaction and reducing exposure to hospital settings. It has also allowed healthcare workers to provide care even when they are in self-quarantine.3 As such, telemedicine is useful in both the primary, secondary and tertiary healthcare system.4 However, because it eliminates the distance between patients and healthcare workers, it is most applicable to secondary and tertiary healthcare, where healthcare facilities are fewer and further away from patients.5
However, it is a relatively new way of healthcare delivery, with its potential benefits and shortcomings.6 Although previous studies have explored the potential of using telemedicine in disasters and public health emergencies,3 health care systems all over were challenged to develop telemedical innovations and fulfill the demand rapidly due to the pandemic. Added to this is how telemedicine is not adopted by all groups of patients, which use of telemedicine linked to factors such as socio-economic status and education.6 Similarly, not all physicians are keen to use telemedicine as well, with concerns about its complexity and effectiveness leading to acceptance or hesitancy to use telemedicine.7,8 Due to the limited evidence on the effectiveness of telemedicine, telehealth programs require study to allow the identification of problems encountered by patients and physicians. However, the lack of physical interaction in telemedicine has been deemed to reduce its usefulness. In addition to this, telemedicine also has ethical and privacy issues, and can only be used effectively by individuals who are well-versed with technology.9
Despite these limitations, telemedicine has been implemented successfully on a large-scale across the world. In Gastroenterology, telemedicine was previously being used to facilitate patient care in chronic diseases, which do not require repeated physical examination,10 such as liver diseases11 and Inflammatory Bowel Disease.12,13 Since the Sars-Cov-2 pandemic, emphasis has been placed on developing programs to conduct consultations remotely. Studies have assessed the feasibility of such remote healthcare delivery.14,15 Many studies have seen encouraging results from patients, with studies finding high patient interest5 and high patient satisfaction with telemedicine programs.14,16 However, most of these studies have dealt with specific patient populations, many of whom have chronic diseases. How telemedicine is perceived by patients with acute diseases, who often expect a physical examination to be an essential part of the consultation, is not well-studied.
In Lower Middle-Income Countries (LMICs) such as Pakistan, telemedicine has only recently been formalized into healthcare, with the recent introduction of guidelines for healthcare workers aiming to use telemedicine.17 Specific institutional guidelines do not exist, with the opportunity of tele consults allowed to all patients. Telemedicine is not only essential in urban areas during the COVID-19 pandemic but can also increase access to healthcare in the rural setting.18 Yet Pakistan does not have large scale telemedicine programs.19 In fact, one survey found that many physicians here did not have basic knowledge about telemedicine.20 The COVID-19 pandemic has, however, changed the landscape, wherein telemedicine may be a necessity, and may even be preferred by patients and physicians.
The first large-scale telemedicine gastroenterology clinics at our tertiary care center started in June 2020. This major shift in modality has not been evaluated for effectiveness, ease of access to patients, and convenience for physicians. Hence, this study aims to evaluate this telemedicine program to improve it for future use. We aim to assess physicians’ and patients’ perspectives of the benefits and challenges of telemedicine at the gastroenterology department at a tertiary care center in Pakistan.
Methods
This cross-sectional study was conducted in the Section of Gastroenterology (SoG) at the Aga Khan University Hospital, a tertiary care center in Pakistan after ethical approval from the institutional ethical review board. All data was analyzed using SPSS (IBM Corp. IBM SPSS Statistics for MAC, Version 25. IBM Corp, Armonk, NY, USA). Physicians employed at the SoG who have conducted telemedicine clinics since June 2020 (N=7) were recruited via an email sent to them on their institutional email address. All consenting physicians were asked to fill the online questionnaire. As only 7 physicians were recruited, data has been analyzed descriptively.
Patients who had at least one telemedicine appointment since June 2020 were recruited using convenience sampling. The sample size of patients required was calculated as follows: in 3 months from mid-March until mid-June 2020, approximately 280 patients took telemedicine appointments and the average number of patients per clinic was 5–7. Adjusting for the population size, the minimum sample size required came to be approximately 150. The questionnaire was tested on 20 patients, who were later excluded from the analysis. Patients above the age of 18 years who consented to participate were recruited and interviewed via telephone calls by trained data collectors. Patients who did not provide consent, had significant language barriers, and those for whom there was no contact information available were excluded. Patients with missing data (missing or incorrect phone numbers) were excluded. Data was analyzed descriptively, with categorical data presented as proportions and percentages and continuous data presented as means and standard deviation. Pearson’s Chi-Square test was used to assess for associations, with a p-value <0.05 considered statistically significant.
Results
Patients’ Perspectives
A total of 473 patients were eligible, but 48 had missing data such as date of consultation, reason for consultation, investigation plan or treatment plan. A total of 425 had complete records and utilized telemedicine in the specified time interval. All patients were called, and after excluding those patients who did not consent, or were not able to be contacted, 160 patients were included in the study, as shown in Figure 1. The mean age of participants was 49.8 ± 17.8 years, with 42.8% (n=68) males. Only 23.8% (n=38) of all visits were initial visits, while 76.3% (n=122) visits were follow-ups, as shown in Table 1. Patients’ perspectives of telemedicine are mentioned in Table 2.
 |
Table 1 Demographic Characteristics of Patients Who Availed Telemedicine Services |
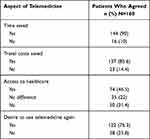 |
Table 2 Patients’ Perspectives of Telemedicine Appointments |
 |
Figure 1 Study flow. |
The majority of patients found telemedicine to be satisfactory with regards to physician-patient communication, as shown in Table 3. However, only 39.6% (n=61) patients felt the visit was as good as an in-person visit. The majority of patients (86.3%, n=138) said they would want to use telemedicine again, as shown in Table 3. Subgroup analysis for gender and age were conducted, but no associations were found significant at a p-value of <0.05.
 |
Table 3 Patients’ Satisfaction with Physician Interaction at the Teleclinic Appointment |
Physicians’ Perspectives
A total of 7 physicians who were conducting telemedicine clinics consented to participating in the study, with most scheduling 3 teleclinics per week. All physicians had been practicing for more than 5 years, with 5 (71.4%) practicing for more than 15 years. Physicians’ perspectives of the telemedicine project team organization and physicians’ satisfaction with telemedicine is given in Table 4. Only 3 (43%) physicians said they would recommend their colleagues to use telemedicine. With regards to the challenges they faced, 2 physicians volunteered that they faced technological issues, 1 stated their team needed training, and 3 stated they could not examine the patient or could not make conclusive clinical decisions. In addition, 3 physicians were of the view that teleclinics should be used in conjecture with in-person visits, 2 suggested training the team, and 1 wanted improvements in technology.
 |
Table 4 Physicians’ Views of the Organization of the Telemedicine Project Team and Their Satisfaction with Teleconsultations |
Discussion
Telemedicine is an umbrella term for long-distance healthcare,1 however, in this article we focused on only a few media of telemedicine: simple phone calls, internet-backed phone calls and videoconferencing. Such media, when used for outpatient consultation, transform the traditional clinic visit into a teleconsultation.21 The use of some of this technology might entail that only those with access to such technology and with the skills to use it benefit from telemedicine. Studies have found that dependence on patient or caregiver literacy is a major disadvantage of telemedicine.22,23 However, this is not only limited to patients. Physicians may also struggle with technology, and there are inherent drawbacks to technology itself, such as issues with software and mistakes in prescription.22 Such limitations mold perceptions about telemedicine that result in an unwillingness of physicians and patients to adopt telemedicine.7
Despite these disadvantages, telemedicine offers novel flexibilities of space and time and reduces travel costs and saves time for patients. Most of the patients interviewed in our study stated that the consultation saved their travel expenditure, which, for a large tertiary-care hospital in a metropolitan city in a LMIC, can mean anywhere from an hour-long drive to travel from the suburbs or other cities. This also translates into saved travel time, along with eliminating waiting time and delays, which are common in large hospitals.
Nearly half of all our participants said they felt telemedicine made it easier to access healthcare. This is similar to a prior study conducted in Pakistan13 and for other low socioeconomic groups,23 as with the widespread accessibility to technology required for telemedicine, healthcare is now accessible to many more patients living in remote areas. However, this technology is still not accessible to all,7 a factor which must be addressed before rural healthcare becomes too reliant on telemedicine. Literature also mentions hidden barriers apart from technological issues,24 such as difficulties in access for individuals with sensory deprivation.24 This indicates the need of a careful assessment of the true access to telemedicine.
The type of visit can also govern the utility of telemedicine. In our study, most of the patients using telemedicine were on follow-up appointments, where the physician had already interacted with them in person prior to their tele-visit. This in-person visit gave the physician the opportunity to assess many aspects of the patient’s life and disease which may not be immediately obvious in the teleconsultation. As remote examinations, such as via the digital stethoscope, are quite uncommon, and unlikely to be widely used until specialized teams are in place,25 and because no adequate substitutes are in place for patient examinations, it is unlikely that telemedicine will fulfill all the demands of the physical consult. This is all the more important in gastroenterology, where the physical examination is of paramount importance, all the way from assessing manifestations of liver disease, to just differentiating abdominal pain using an abdominal exam. Similarly, in our study we did see that 86.3% of patients would use telemedicine again, but only 39.6% felt it was as good as an in-person visit. Moreover, literature shows that patients who met their physician before were more likely to be satisfied with telemedicine.26 Thus, telemedicine may play a more valuable role in close follow-up care.27
Apart from patients’ perspectives, the perspectives of the physician are of paramount importance in the evaluation of telemedicine. Our study focused on two major areas of telemedicine when asking physicians their perspectives: technological issues and effect on healthcare, as shown in Table 4. Our study shows that physicians do not think their telemedicine team has sufficient training, even at a large academic tertiary-care hospital, however, physicians themselves are comfortable with the technology. Technological issues have been a major challenge in using telemedicine28 since its inception. Apart from the major issue of inability to perform a physical examination and technological issues,29 there are inherent limitations in the technology interface itself.29,30 This indicates the need for not only training for existing teams and improvements in technology, but also a careful assessment of the true access to telemedicine. However, with improvements in technology, higher satisfaction rates are possible, as in a study conducted by Lee et al on pediatric gastroenterologists, which found that most physicians felt the technology was usable.30 This indicates the need for improvements in training for existing teams and in technology.
With regards to telemedicine’s effect on healthcare, we found mixed views. Most physicians believed that telemedicine is useful for healthcare, but not as many wanted to use it, nor did they find it useful for their own practice. These results are not as encouraging as those found in literature. Our study showed that physicians’ difficulty with learning and using technology may not be as significant as previously thought. We found that most physicians did not need to learn to use this technology, possibly because it was already widely used during the pandemic, and all were comfortable using it. Even if they required help, all felt they could call for assistance. As such, they were in favor of telemedicine and felt it did not negatively affect their healthcare delivery. A study conducted by Lee et al on pediatric gastroenterologists found high satisfaction with telemedicine.30 Similarly, Tenforde et al, which shows a 92% satisfaction rate for telemedicine during the pandemic in musculoskeletal medicine physicians, another specialty for which physician examination is vital.28 In order to enhance the uptake of telemedicine, physician hesitation must be explored in more detail with large, multi-centered studies, so that the shortcomings of telemedicine are met and physicians’ reservations are addressed.
There are several ways in which physician and patient perspectives can be addressed to ensure that telemedicine is utilized more in the future. While focusing on tackling many of the technological barriers and other concrete issues is undoubtably necessary, perhaps, beyond this, it is important to correct negative perceptions regarding telemedicine amongst both patients and physicians. An example is by organizing discussions with physicians regarding not only the problems they face when using telemedicine to provide healthcare, but also to identify and address any misconceptions they might have about telemedicine, such as providing statistics about how useful patients find it, or correcting ideas about true complexity of use. Well-informed physicians can be a bridge to improved patient perceptions as well. Apart from that, formally advertising telemedicine as the useful tool, on both the individual and the national level, that it is, is of utmost importance as well. Lastly, to facilitate the use of telemedicine, we require future studies that assess perceptions in more detail, such as how patient perceptions are affected by physicians’ attitudes about telemedicine. Thus, this study can help frame questions for future research and also shape programs to address barriers faced by physicians’ and patients’ in using telemedicine.
Conclusion
The use of telemedicine became widespread due to the COVID-19 pandemic, where it allowed accessibility to effective healthcare without the risk of infection from a hospital visit.22,23,27 Telemedicine is, however, here to stay due to its many advantages. However, its use must be evaluated to ensure that teleconsultations are utilized in the correct setting after appropriate training of staff and physicians, so that the experience is as rewarding for patients and physicians as possible, and patient care is not compromised. Tackling physicians’ and patients’ perspectives regarding telemedicine can help increase its usage and allow many more patients to experience its benefits. Further research into how perspectives about telemedicine are shaped can be used to better address misconceptions and increase telemedicine adoption.
Author Information
Anjiya Shaikh and Maria Khan share co-first authorship.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Bashshur RL, Reardon TG, Shannon GW. Telemedicine: a new health care delivery system. Annu Rev Public Health. 2000;21:613–637. doi:10.1146/annurev.publhealth.21.1.613
2. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. In: JAMA Internal Medicine. Vol. 178. American Medical Association; 2018:745–746.
3. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi:10.1056/NEJMp2003539
4. Baldwin LP, Clarke M, Eldabi T, Jones RW. Telemedicine and its role in improving communication in healthcare. Logist Inform Manag. 2002;15:309–319. doi:10.1108/09576050210436147
5. Nobre LF, Wangenheim AV. Development and implementation of a statewide telemedicine/telehealth system in the state of Santa Catarina, Brazil. In: Technology Enabled Knowledge Translation for eHealth. New York, NY: Springer; 2012:379–400.
6. Luo J, Tong L, Crotty BH, et al. Telemedicine adoption during the COVID-19 pandemic: gaps and inequalities. Appl Clin Inform. 2021;12(04):836–844. doi:10.1055/s-0041-1733848
7. Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Irish J Med Sci. 2021;190(1):1. doi:10.1007/s11845-020-02299-z
8. Jnr BA. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):1–9.
9. Lee T, Kim L. Telemedicine in gastroenterology: a value-added service for patients. Clin Gastroenterol Hepatol. 2020;18(3):530–533. doi:10.1016/j.cgh.2019.12.005
10. Technology literacy as a barrier to telehealth during COVID-19 [Internet]; 2020. Available from: https://www.researchgate.net/publication/341513611_Technology_Literacy_as_a_Barrier_to_Telehealth_During_COVID-19.
11. Siegel CA. Transforming gastroenterology care with telemedicine. Gastroenterology. 2017;152(5):958–963. doi:10.1053/j.gastro.2017.01.048
12. Cross RK, Kane S. Integration of telemedicine into clinical gastroenterology and hepatology practice. Clin Gastroenterol Hepatol. 2017;15(2):175–181. doi:10.1016/j.cgh.2016.09.011
13. Riaz MS, Atreja A. Personalized technologies in chronic gastrointestinal disorders: self-monitoring and remote sensor technologies. Clin Gastroenterol Hepatol. 2016;14(12):1697–1705. doi:10.1016/j.cgh.2016.05.009
14. Population health management for inflammatory bowel disease - PubMed [Internet]; 2020. Available from: https://pubmed.ncbi.nlm.nih.gov/29122544/.
15. Serper M, Cubell AW, Deleener ME, et al. Telemedicine in liver disease and beyond: can the COVID-19 crisis lead to action? Hepatology. 2020;72:723–728. doi:10.1002/hep.31276
16. Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2):e18810. doi:10.2196/18810
17. Ministry of National Health, Government of Pakistan. Policy for telemedicine in Pakistan. Ministry of National Health, Government of Pakistan; 2021. Available from: https://nhsrc.gov.pk/SiteImage/Misc/files/FinalPolicy%20for%20Telemedicine%20in%20Pakistan%20(1)(1).pdf. Accessed June 11, 2022.
18. Siniscalchi M, Zingone F, Savarino EV, D’Odorico A, Ciacci C. COVID-19 pandemic perception in adults with celiac disease: an impulse to implement the use of telemedicine. Dig Liver Dis. 2020;52:1071–1075. doi:10.1016/j.dld.2020.05.014
19. Zafar A. Telemedicine Country Report-Pakistan. 2007:90–94.
20. Qureshi A. The telemedicine landscape in Pakistan - why are we falling behind? J Pak Med Assoc. 2019;69:757.
21. Kamal SA, Hussain S, Shafiq M, Jahanzaib M. Investigating the adoption of telemedicine services: an empirical study of factors influencing physicians’ perspective in Pakistan. Nucleus. 2018;55(3):153–163.
22. Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health. 2020;11:2150132720980612. doi:10.1177/2150132720980612
23. Mahajan V, Singh T, Azad C. Using telemedicine during the COVID-19 pandemic. Indian Pediatr. 2020;57(7):658–661. doi:10.1007/s13312-020-1895-6
24. Tenforde AS, Iaccarino MA, Borgstrom H, et al. Feasibility and high quality measured in the rapid expansion of telemedicine during COVID‐19 for sports and musculoskeletal medicine practice. Pm R. 2020;12:926–932. doi:10.1002/pmrj.12422
25. Bokolo AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID‑19 pandemic. Health Technol. 2021;11(2):359–366. doi:10.1007/s12553-020-00516-4
26. Ramirez AV, Ojeaga M, Espinoza V, Hensler B, Honrubia V. Telemedicine in minority and socioeconomically disadvantaged communities amidst COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;64:91–92.
27. Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Irish J Med Sci. 2020;190:1.
28. Pinar U, Anract J, Perrot O, et al. Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic. World J Urol. 2020;38:1–6. doi:10.1007/s00345-019-03039-4
29. Zhai Y. A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom. 2020;2020:1.
30. Lee JA, Di Tosto G, McAlearney FA, et al. Physician perspectives about telemedicine: considering the usability of telemedicine in response to coronavirus disease 2019. J Pediatr Gastroenterol Nutr. 2021;73(1):42. doi:10.1097/MPG.0000000000003149
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
