Back to Journals » Research and Reports in Urology » Volume 15
Evaluation of the Diagnostic Performance of the LINEAR Cromatest and Laboquick URS 10-T Dipsticks Among Urinary Tract Infection Suspects in Addis Ababa, Ethiopia: A Cross-Sectional Study
Authors Gebretensaie Y, Atnafu A , Alemu Y , Girma S , Desta K
Received 6 August 2023
Accepted for publication 28 September 2023
Published 4 October 2023 Volume 2023:15 Pages 437—445
DOI https://doi.org/10.2147/RRU.S434128
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Yosef Gebretensaie,1,* Abay Atnafu,2,* Yonas Alemu,3 Selfu Girma,2 Kassu Desta4,*
1American Advanced Medical Laboratory, American Medical Center, Addis Ababa, Ethiopia; 2Armauer Hansen Research Institute, Addis Ababa, Ethiopia; 3Department of Microbiology, Immunology, and Parasitology, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 4Department of Medical Laboratory Science, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
*These authors contributed equally to this work
Correspondence: Yosef Gebretensaie, Tel +251913063450, Email [email protected]
Background: Urinary tract infections (UTIs) bring a significant and serious health-related problem. Repeated infections may lead to the development of renal scarring and end-stage renal dysfunction. Therefore, balancing the choices of UTI diagnostic tools depending on the costs versus accuracy can minimize false results that may subject patients to wrong treatments.
Objective: The objective of the study was to evaluate the diagnostic performance of LINEAR cromatest and Laboquick URS 10-T dipsticks against conventional urine culture at Arsho Advanced Medical Laboratory (AAML), Addis Ababa, Ethiopia.
Methods: A similar cohort of UTI-suspected patients from our previous study, who were prospectively enrolled from Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia, were considered for this analysis. Data analysis was performed using SPSS version 26. The sensitivity, specificity, and predictive value of different dipsticks were calculated using culture as a gold standard. ROC curve analysis was also used to determine diagnostic performance. A test with a P-value of < 0.05 was considered statistically significant.
Results: Out of 446 urine samples processed, bacterial growth was observed in 141 (31.6%). Of this figure, 105/141 (74.5%) and 36/141 (25.5%) were from female and male participants, respectively. The sensitivity and specificity of the LINEAR Cromatest dipstick were 83.7% and 67.9%, respectively (P-value < 0.001). The Laboquick URS 10-T dipstick showed sensitivity and specificity of 87.9% and 68.5%, respectively (P-value < 0.001). The ROC analysis showed an AUC of > 0.7 for both dipsticks.
Conclusion: In a setting where there is no access to urine culture, the urine dipstick may be considered an alternative diagnostic tool in the diagnosis of UTIs.
Keywords: AUC, dipstick test, diagnostic accuracy, sensitivity, urine culture, UTI
Introduction
Urinary tract infection (UTI) is an infection of the urinary tract system involving the kidney, bladder, ureter, and urethra.1 It has been shown that UTIs lead to serious public health concerns in different resource-poor settings, affecting people of all ages; females are reported to be at higher risk.2–4
In resource-poor countries like Ethiopia, the diagnosis of UTIs primarily relies on the evaluation of clinical signs and symptoms, which often, upon generation of relevant clinical evidence, are further referred for more reliable bacteriological confirmation, such as culture for the etiological agent.2,5–7
When dictating the diagnosis of UTI using urine culture, some issues, such as the fact that it is time-consuming, there is limited availability of the necessary infrastructure, and it is expensive, have been raised as concerns.2,8 In another instance, such limitations seem to be alleviated with the advent of urine dipstick tests, despite their inherent drawbacks such as low accuracy and non-specificity, which hinders their potential applicability in clinical use and make them unsuitable for treatment decisions.8,9 However, besides the indicated limitation of the urine dipstick test, a positive result generated by the dipstick is that it provides generalized evidence of the presence of a UTI. A negative result, in contrast, needs further urine culture confirmation before ruling out a UTI.10
On the positive side, the urine dipstick test is a user-friendly method to perform, is easier to interpret, has a short turn-around time, and has the potential of being applicable on a larger scale in different health settings.10–12 An effort to establish an effective laboratory diagnosis, such as that of a urine dipstick, could provide great benefits, such as a rapid and inexpensive test that allows the practitioner to plan targeted, more effective therapy and indirectly reduce unnecessary time wastage and expense.2 However, there is a paucity of data in our setting narrating the diagnostic effectiveness of such diagnostic tools. Therefore, this study aimed to evaluate the diagnostic performance of the Combiscreen and Laboquick dipsticks among urinary tract infection suspected in Addis Ababa, Ethiopia, with culture as the gold standard.
Materials and Methods
Study Setting
A similar cohort of UTI suspected patients, who were prospectively enrolled13 from Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia, were considered for this analysis. Arsho Advanced Medical Laboratory has been providing routine and advanced laboratory diagnostic services for the entire city and for other referral cases from different regional states of Ethiopia. The sample size calculations were performed to calculate the prevalence rate based on the following assumptions. The value of the constant proportion was set conservatively at 12%14 for the prevalence rate of UTIs in Ethiopia, an alpha, type 1 error, balanced on each side, set to 5%, and a statistical power of 80%. The minimum required sample size satisfying the indicated assumptions was 425 from a calculation done using the G*Power 3.1.9.7 software.15 All UTI suspected patients who were willing to participate in this study were included and patients with a history of drug treatment within the past 2 weeks before starting this study were excluded from it. Patients were asked to consent to participation after a brief explanation, then a structured data collection format was used to collect baseline data that included information about socio-demographic characteristics and patients’ medical records using trained interviewers. Informed consent from parents/guardians was obtained for the participants under the age of 18. Data was entered and statistically analyzed using SPSS version 26.0 software. The sensitivity (SN), specificity (SP), and predictive value of different dipsticks were calculated using culture as a gold standard. A test with a P-value of <0.05 was considered statistically significant. The study was conducted after receiving ethical approval, which complies with the Declaration of Helsinki, from the Department of Research and Ethical Review Committee (DRERC) of the Department of Medical Laboratory Sciences, College of Health Sciences, Addis Ababa, Ethiopia. Informed written consent was obtained from participants before data collection.
Sample Collection
To reduce the risk of contamination, participants were instructed to clean their hands and genital area, respectively, before collection of the clean catch mid-stream urine samples. The samples were collected using a sterile, wide-mouthed urine cup and processed in the laboratory within 2 hours of collection. Specimens that were not processed within 2 hours were kept in the refrigerator at 4°C until being processed.
Sample Processing for Identification Using Urine Culture and Urine Dipstick Test
The appropriate urine samples collected from each patient were inoculated onto blood agar base (Oxoid, Basingstoke, Hampshire, UK) to which 10% sheep blood and MacConkey agar (Oxoid, Basingstoke, Hampshire, UK) were added using a calibrated loop 10µL. Following incubation at 37°C for 18–24 hours aerobically and in an atmosphere containing 5–7% CO2 for 48 hours, the number of colonies was counted and a bacterial growth of >105 cfu/mL in urine was considered significant for bacteriuria. Pure isolates of the bacterial pathogen were preliminarily characterized by colony morphology, gram stain, and biochemical tests. Above all, preparation and performance evaluation of culture media was performed as per manufacturers’ instructions. At the same time, urine samples from all participants were tested within 10 minutes using two dipsticks, LINEAR Cromatest (Barcelona, Spain) and LABOQUICK URS-10T (Bornova Izmir, Turkey). Reagent strips were used for all specimens in accordance with manufacturers’ instructions. Urine dipstick bottles were stored at room temperature and expiration dates were also checked before use. Urine dipstick test results were interpreted according to manufacturers’ instructions.
Results
Socio-Demographic Characteristics
A total of 446 UTI suspected patients who were willing to take part in this study and who hadmet the inclusion criteria were enrolled. There were more female than male participants and ages ranged between 20–69 years, accounting for 293/446 (65.7%) and 336/446 (75.3%), respectively. Patients ranged in age from 10 months to 90 years, with a mean of 43.39 years and a standard deviation of ± 21.68 years.
Prevalence of UTI and Bacterial Isolates in Urine Culture
The prevalence of UTIs was 141/446 (31.6%) in accordance with the conventional culture method. The lowest prevalence of significant bacterial growth in urine culture was shown in the infant and baby age group, 0–2 years; for those aged 20–29, it was 27/141 (19.14%); and for those aged 30–39, it was 30/141 (21.27%). A higher rate of prevalence of UTIs was observed in females, who accounted for 105/141 (74.5%), compared to men, 36/141 (25.5%); see Table 1.
 |
Table 1 Prevalence of UTI Distribution Corresponding to Age Group and Gender in the Study Participants at Arsho Advanced Medical Laboratory from March 08 to May 20, 2021 |
Detection Rate of the Two Urine Dipstick Tests
Of the 446 urine samples tested, according to the LINEAR Cromatest dipstick test 216/446 (48.4%) UTIs were identified. The individual parameters included in the LINEAR Cromatest dipstick results were 153/446 (34.3%), 79/446 (17.7%), and 84/446 (18.8%) leukocyte esterases, nitrites, and blood, respectively. On the other hand, UTI cases detected by Laboquick URS-10T dipstick accounted for 220/466 (49.3%). The individual parameters of the Laboquick URS-10T dipstick were reported as 177/446 (39.7%), 52/466 (11.7%), and 82/446 (18.4%) for leukocytes, nitrites, and blood, respectively, as shown in Table 2.
Diagnostic Performance of Rapid Urine Dipstick Using Area Under the Curve (AUC)
The AUCs shown on receiver operating characteristic (ROC) curve analysis were 0.782 and 0.758 for Laboquick URS-10T dipstick and LINEARCromatest dipstick, respectively. ROC analysis for each individual parameter revealed different test results: poor diagnostic performance was shown for blood and nitrite parameters when used alone to determine UTI cases (AUC <0.7) for both Laboquick and LINEAR Cromatest dipsticks; however, leukocyte esterase was determined to be a good diagnostic predictor (AUC >0.8) for both Laboquick and Combi dipsticks, showing AUC values of 0.827 and 0.814, respectively. See Table 3 and Figure 1.
 |
Table 3 Diagnostic Accuracy and Performance of linear Cromatest and Laboquick URS-10T Dipsticks Through Calculating AUC at Arsho Advanced Medical Laboratory from March to May 20, 2021 |
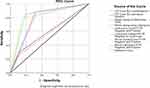 |
Figure 1 ROC curve for LINEAR Cromatest and Laboquick URS-10T dipstick diagnosis with urine culture as gold standard at Arsho Advanced Medical Laboratory from March to May 20, 2021. |
Diagnostic Performance of the Two Urinary Dipsticks with Culture as Gold Standard
Taking the culture results as a gold standard, the sensitivity and specificity of the LINEAR Cromatest dipstick were 83.7% and 67.9%, and the positive predictive value (PPV) and negative predictive value (NPV) were 54.6% and 90.0%, respectively. Similarly, the SN and SP values for leukocyte esterase (LE) were 77.3% and 85.6%, nitrite (NIT) were 30.5% and 88.2%, respectively, and for blood were 31.9% and 87.2%, respectively. On the contrary, the sensitivity and specificity values of the Laboquick URS-10T dipstick were 87.9% and 68.5%, with a PPV and an NPV of 56.4% and 92.5%, respectively. See Table 4.
 |
Table 4 Diagnostic Performance of LINEAR Cromatest and Laboquick URS 10-T Dipsticks with Culture as Gold Standard |
Discussion
This study was conducted to determine the diagnostic performance of UTIs using conventional and rapid diagnostic methods to identify the prevalence of bacterial agents involved in UTIs. To evaluate the magnitude of the drug susceptibility profile of bacterial uropathogens, 446 participants clinically suspected of having UTIs were enrolled, and revealed the following results: a prevalence rate for significant bacterial growth in culture media in urine samples of 141/446 (31.6%, 95% confidence interval, 27.3–36.2); and more female (105/293, 35.8%) than male (39/153, 23.5%) participants. Participants were aged between 10 months and 90 years. The prevalence of UTIs in the current study was reasonably in agreement with thosereported in Uganda (32.2%),16 South-Western Uganda (35%),17 and India (45.32%)18 but higher compared to Libya (13.9%),19 North India (17.0%),20 and Ethiopia, particularly in Yekatit 12 Medical College Hospital (15.9%)21 . On the contrary, the prevalence rate of UTIs in this study was much lower than those reported in Shashemene, Ethiopia (90.1%)22 and India, Madhya Pradesh (65.5%).23
In this study, the SN, SP, PPV, and NPV of LINEAR Cromatest and Laboquick URS 10–10 dipsticks for leukocyte esterase, nitrite, and blood, individual parameters and in combination, were assessed. The current study contradicted a finding at National Hospital, Tanzania12 revealing urine dipstick results of 56% SN and 85% SP and 91% PPV and 42% NPV. We reported better sensitivity through the utilization of leukocyte esterase, nitrites and blood used in combination with both LINEAR Cromatest and Laboquick URS 10–10 dipsticks, a finding supported by a study in Turkey9 whereby a combination of leukocyte esterase, nitrite, and blood significantly improved the SN value from 65% to 80%. On the contrary, SP decreased from 64% to 60% due to increased false-positive results. Moreover, a study in India5 found that blood parameter showed the highest sensitivity for the single test, which contradicted the current study, which found that leukocyte esterase was the only parameter that achieved the highest sensitivity value for both dipsticks; better sensitivity was achieved when nitrite, leukocyte, and blood were considered together, increasing sensitivity to 74.02% compared to the individual sensitivity values of nitrite, leukocyte esterase, and blood of 23.31%, 48.5%, and 63.94%, respectively. This study contradicted the results of a study conducted in 2017 in the Department of Pediatrics, Father Mullers Medical College and Hospital, Mangalore, Karnataka, India that found a highly significant P-value (0.000001) for the urine dipstick test for nitrite alone compared to leukocyte esterase alone with a P-value of 0.06, which is not significant when compared to urine culture in the diagnosis of UTI. However, the diagnostic advantage of the urine dipstick method for diagnosing UTIs using both LE and NIT together has a significant P-value of 0.018, which can permit its use as a screening test for ruling out (or in) UTIs,24 which agreed with the current study.
In Ethiopia many health care set-ups utilize rapid dipstick analysis using leukocyte esterase, nitrites, and blood for screening purposes of UTI, but different studies revealed the poor SN and PPV of rapid dipstick tests to detect UTIs.5,10,12,25,26 In this study, nitrite and blood dipstick found low SN and PPV that resulted in poor detection of culture-positive bacteriuria cases. Similarly, a study conducted in 2015 at the PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India showed that dipstick analysis in outpatient settings and primary health centers for first-level screening always needs to be correlated with a clinical presentation because the assay is not reliable for considering and predicting a definitive diagnosis of UTI. It thus recommends performing urine culture or, alternatively, increasing the sensitivity of blood, nitrite, and LE tests by using them in combination.5 Leukocyte esterase was not specific for bacteriuria, which is vulnerable to a high false-positive result if other inflammatory conditions exist, even if it persists after bacteriuria had cleared, which means the presence of leukocyte esterase in urine is not always correlated with bacteriuria and pyuria. In contrast, the low sensitivity of nitrite results in a false-negative outcome because the nitrite test depends on the formation or reduction of nitrate by enteric bacteria, most commonly by the genus of the Enterobacteriaceae family, which is highly specific and indicative of bacteriuria. As well as Enterobacteriaceae not reducing nitrate to nitrite, false-negative results may occur if urine stays for an insufficient time in the bladder, which means that the bacterial agent does not change the nitrate into nitrite; if urine remains in the bladder for a protracted time, in contrast, this results in a reduction of nitrates beyond the nitrite stage, something that also happens if dietary nitrite is absent in the body.10
Deviating from this study, a study conducted in South-Western Uganda17 found that Klebsiella pneumoniae is the most common isolate (37.41%). Similarly, unlike in the current study, K. pneumoniae has been recorded as the most common isolate in Asia, specifically Madhya Pradesh, India.23
Despite the limitations of a rapid dipstick test for diagnosing UTIs, it is used as a preliminary diagnostic tool before beginning empirical treatment, which makes it beneficial in health settings lacking trained personnel or ill-equipped for processing urine cultures. The rapid dipstick test will reduce the unnecessary use of broad spectrum antibiotics and, therefore, decrease and fight the excessive use of antibiotics.27 Rapid screening tests contribute to the diagnosis of UTIs by providing information in a timely manner for early initiation of antibiotic therapy to halt further complications, and encourage the screening of many populations, including those in the symptomless stage, such as elderly people. It is a cost-efficient technique.24,28
Conclusion
From the findings in our study, we concluded that, in a resource-poor setting, employing urine dipsticks as an alternative preliminary diagnostic tool could benefit healthcare providers before the provision of empirical treatments. Patients, on the other hand, could benefit from the provision of urinary dipsticks in the light of economy and obtaining early diagnosis. However, a urinary dipstick test suffers from relatively lower specificity, which may result in low accuracy, therefore culture confirmation should better be provided whenever possible for more accurate and confirmatory outcomes.
Data Sharing Statement
The underlying data is available upon request.
Acknowledgment
We would like to extend our gratitude to the study participants enrolled in this study.
Funding
The authors received no specific funds to conduct this study.
Disclosure
The authors declare no conflicts of interest in this study.
References
1. Mayo clinic. Urinary tract infection (UTI): mayo Foundation for Medical Education and Research; 2020 Available from: https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447.
2. Murgia L, Stalio O, Arienzo A, et al. Management of Urinary Tract Infections: problems and Possible Solutions. Urinary Tract Infection-The Result of the Strength of the Pathogen, or the Weakness of the Host. 2018.
3. Sabih A, Leslie SW. Complicated Urinary Tract Infections. Europe PMC. 2020.
4. Harb A, Yassine V, Ghssein G, Salami A, Fakih H. Prevalence and Clinical Significance of Urinary Tract Infection among Neonates Presenting with Unexplained Hyperbilirubinemia in Lebanon: a Retrospective Study. Infection Chemotherapy. 2023;55(2):194–203. doi:10.3947/ic.2022.0117
5. Mambatta AK, Jayarajan J, Rashme VL, Harini S, Menon S, Kuppusamy J. Reliability of dipstick assay in predicting urinary tract infection. J Family Med Prim Care. 2015;4(2):265–268. doi:10.4103/2249-4863.154672
6. Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis. 2004;38(8):1150–1158. doi:10.1086/383029
7. Sokhn ES, Salami A, El Roz A, Salloum L, Bahmad HF, Ghssein G. Antimicrobial Susceptibilities and Laboratory Profiles of Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis Isolates as Agents of Urinary Tract Infection in Lebanon: paving the Way for Better Diagnostics. Med Sci. 2020;8(3):32. doi:10.3390/medsci8030032
8. Rangaiahagari A, Nyirabanzi J, Uwizeyimana J, Ngoga E, Wane J. Comparison of urine culture and urine dipstick nitrite test in diagnosis of Urinary Tract Infection. Rwanda Medical J. 2015;72(1):5–7.
9. Memişoğulları R, Yüksel H, Yıldırım HA, Yavuz Ö. Performance characteristics of dipstick and microscopic urinalysis for diagnosis of urinary tract infection. Eur J Gen Med. 2010;7(2):174–178.
10. Demilie T, Beyene G, Melaku S, Tsegaye W. Diagnostic accuracy of rapid urine dipstick test to predict urinary tract infection among pregnant women in Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia. BMC Res Notes. 2014;7(1):481. doi:10.1186/1756-0500-7-481
11. Huysal K, Budak YU, Karaca AU, et al. Diagnostic accuracy of uriSed automated urine microscopic sediment analyzer and dipstick parameters in predicting urine culture test results. Biochem Med (Zagreb). 2013;23(2):211–217. doi:10.11613/BM.2013.025
12. George Msema B, Leonard K, James K, Lilian N, Akili M, Kennedy Daniel M. Diagnostic accuracy of dipsticks test among clinically suspected urinary tract infected patients at National Hospital, Tanzania. Open J Bacteriol. 2019;3(1):003–7. doi:10.17352/ojb.000009
13. Gebretensaie Y, Atnafu A, Girma S, Alemu Y, Desta K. Prevalence of Bacterial Urinary Tract Infection, Associated Risk Factors, and Antimicrobial Resistance Pattern in Addis Ababa, Ethiopia: a Cross-Sectional Study. Infect Drug Resist. 2023;16:3041–3050. doi:10.2147/IDR.S402279
14. Alemu M, Belete MA, Gebreselassie S, Belay A, Gebretsadik D. Bacterial Profiles and Their Associated Factors of Urinary Tract Infection and Detection of Extended Spectrum Beta-Lactamase Producing Gram-Negative Uropathogens Among Patients with Diabetes Mellitus at Dessie Referral Hospital, Northeastern Ethiopia. Diabetes Metab Syndrome Obesity. 2020;13:2935–2948. doi:10.2147/DMSO.S262760
15. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi:10.3758/BF03193146
16. Odoki M, Almustapha Aliero A, Tibyangye J, et al. Prevalence of Bacterial Urinary Tract Infections and Associated Factors among Patients Attending Hospitals in Bushenyi District, Uganda. Int J Microbiol. 2019;2019:4246780. doi:10.1155/2019/4246780
17. Johnson B, Stephen BM, Joseph N, Asiphas O, Musa K, Taseera K. Prevalence and bacteriology of culture-positive urinary tract infection among pregnant women with suspected urinary tract infection at Mbarara regional referral hospital, South-Western Uganda. BMC Pregnancy Childbirth. 2021;21(1). doi:10.1186/s12884-021-03641-8
18. Shaifali I, Gupta U, Mahmood SE, Ahmed J. Antibiotic susceptibility patterns of urinary pathogens in female outpatients. N Am J Med Sci. 2012;4(4):163–169. doi:10.4103/1947-2714.94940
19. Mohammed MA, Alnour TM, Shakurfo OM, Aburass MM. Prevalence and antimicrobial resistance pattern of bacterial strains isolated from patients with urinary tract infection in Messalata Central Hospital, Libya. Asian Pac J Trop Med. 2016;9(8):771–776. doi:10.1016/j.apjtm.2016.06.011
20. Chooramani G, Jain B, Chauhan PS. Prevalence and antimicrobial sensitivity pattern of bacteria causing urinary tract infection; study of a tertiary care hospital in North India. Clin Epidemiol Global Health. 2020;8(3):890–893. doi:10.1016/j.cegh.2020.02.018
21. Merga Duffa Y, Terfa Kitila K, Mamuye Gebretsadik D, Bitew A. Prevalence and Antimicrobial Susceptibility of Bacterial Uropathogens Isolated from Pediatric Patients at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia. Int J Microbiol. 2018;2018:8492309. doi:10.1155/2018/8492309
22. Seifu WD, Gebissa AD. Prevalence and antibiotic susceptibility of Uropathogens from cases of urinary tract infections (UTI) in Shashemene referral hospital, Ethiopia. BMC Infect Dis. 2018;18(1):30. doi:10.1186/s12879-017-2911-x
23. Singh R, Netam AK, Sharma P. Prevalence and in vitro antibiotic susceptibility pattern of bacterial strains isolated from tribal women suffering from urinary tract infections in District Anuppur, Madhya Pradesh, India. Biomed Res Therapy. 2020;7(8):3944–3953. doi:10.15419/bmrat.v7i8.625
24. Fernandes DJ, Jaidev M, Castelino DN. Utility of dipstick test (nitrite and leukocyte esterase) and microscopic analysis of urine when compared to culture in the diagnosis of urinary tract infection in children. Int J Contemporary Pediatrics. 2017;5(1):156. doi:10.18203/2349-3291.ijcp20175578
25. Semeniuk H, Church D. Evaluation of the leukocyte esterase and nitrite urine dipstick screening tests for detection of bacteriuria in women with suspected uncomplicated urinary tract infections. J Clin Microbiol. 1999;37(9):3051–3052. doi:10.1128/JCM.37.9.3051-3052.1999
26. Cystitis TE. Uncomplicated urinary infection in women: diagnosis. Rev Assoc Med Bras. 2011;57(3):255–258. doi:10.1016/S0104-4230(11)70054-9
27. Ezzeddine Z, Ghssein G. Towards new antibiotics classes targeting bacterial metallophores. Microb Pathog. 2023;182:106221. doi:10.1016/j.micpath.2023.106221
28. Pfaller MA, Koontz FP. Use of rapid screening tests in processing urine specimens by conventional culture and the AutoMicrobic system. J Clin Microbiol. 1985;21(5):783–787. doi:10.1128/jcm.21.5.783-787.1985
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

