Back to Journals » Local and Regional Anesthesia » Volume 14
Evaluation of the Analgesic Efficacy of Bilateral Ultrasound-Guided Transversus Thoracic Muscle Plane Block on Post-Sternotomy Pain: A Randomized Controlled Trial
Authors Shokri H , Ali I, Kasem AA
Received 13 September 2021
Accepted for publication 30 October 2021
Published 12 November 2021 Volume 2021:14 Pages 145—152
DOI https://doi.org/10.2147/LRA.S338685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Hoda Shokri,1 Ihab Ali,2 Amr A Kasem1
1Department of Anesthesiology, Ain Shams University, Cairo, Egypt; 2Department of Cardiothoracic Surgery, Ain Shams University, Cairo, Egypt
Correspondence: Hoda Shokri
Ain Shams University, Cairo, Egypt
Tel +20 1211179234
Email [email protected]
Purpose: Transverse thoracic block is a new perioperative analgesic method for post-sternotomy discomfort. This study discusses the efficacy of an ultrasound-guided transversus thoracic muscle plane block (TTPB) in patients undergoing heart surgery, including sternotomy.
Patients and Methods: In this prospective trial, 60 patients were randomly assigned to two groups: transversus (T) or general anesthesia (GA). Patients in the T group received TTPB with GA and 15 mL of 0.25% bupivacaine was administered on either side. Patients in the GA group received TTPB along with GA, but 15 mL saline was injected on either side instead. The patients were followed up postoperatively. The percentage of patients receiving additional opioids, extubation time, intensive care unit (ICU) length, postoperative morphine dose, and adverse events were documented.
Results: The percentage of patients requiring additional morphine was significantly lower in the T group (p< 0.015). Pain scores were comparable between the groups at extubation time and 18 h postoperatively. At 8, 12, and 24 h after surgery, pain scores in the T group were significantly lower (P< 0.001). The total amount of morphine required after surgery was much lower in the T group (8± 0.74 mg), and the duration to initial analgesic necessity was significantly greater in the GA group (P< 0.001). Patients in the GA group had a considerably longer ventilation time (11.07± 0.64) (P< 0.001). The ICU stay in the T group was substantially shorter (P< 0.001), and postoperative complications were comparable.
Conclusion: For patients undergoing heart surgery, TTPB offers sufficient postoperative pain control, resulting in lower pain scores, lower postoperative analgesic doses, shorter extubation times, and shorter ICU stay lengths.
Keywords: transversus thoracic block, adult cardiac surgery, postoperative analgesia, sternotomy
Introduction
Cardiac surgery with a median sternotomy generates severe discomfort in the sternum, which may lead to delirium, hemodynamic instability, or pulmonary problems.1 Multimodal analgesic techniques for perioperative pain control in cardiac surgery rely heavily on systemic opioids which cause side effects such as vomiting, respiratory depression and itching.2,3 Because of the risk of hematoma formation following full heparinization intraoperatively, regional methods such as epidural or spinal blocks are not routinely employed in heart surgery but it drew the attention to increased use of plane blocks due to their safety and closeness to the field of surgery.4
The anterior branches of the T2–T6 intercostal nerves, which provide sensory supply to the internal mammary area, carry sternotomy-induced discomfort. It has been discovered that inhibiting nerves at the surgery site can relieve sternotomy discomfort while avoiding the hazards of more intrusive procedures.5
Ultrasound-guided transversus thoracic muscle plane block (TTPB), introduced by Ueshima in 2015, is a novel technique in which a local anesthetic (LA) is given as a single shot into the fascial plane between the transversus thoracic muscle (TTM) and the internal intercostal muscles (IIM) to block the anterior branches of T2-T6 as part of multimodal analgesic techniques.6,7 The goal of this prospective randomized trial was to determine the effectiveness of TTPB for adult patients undergoing heart surgery including sternotomy incision in terms of the percentage of patients requiring extra doses of morphine, postoperative pain scores, postoperative opioid consumption, intensive care unit (ICU) stay length, and the incidence of local or systemic complications of the technique or the agents injected.
Patients and Methods
The study was approved by the Research Ethics Committee of Ain Shams University (approval number FMASU R 20/2020/2021) done on January 21st, 2021. This study was registered at ClinicalTrials.gov (registration number NCT04872192).
Inclusion and Exclusion Criteria
All patients signed a written informed consent form. This prospective, double-blind, parallel-group clinical investigation included 60 adult patients aged 55–74 years who were ASA (American Association of Anesthesiologists) II and III who underwent elective cardiac surgery with median sternotomy performed by the same surgical team at Ain Shams University Hospital, cardiothoracic academy, from May to August 2021.
Patients who had been intubated for more than 24 h prior to surgery, patients undergoing complex cardiac procedures, patients with severe chronic obstructive pulmonary disease, patients unable to communicate, patients with chronic pain and severe pulmonary hypertension, as well as any contraindication to regional anesthesia or drug allergy, were all excluded from the study.
Study Design and Participants
Induction of Anesthesia and Monitoring
A detailed medical history, including medications used, and full investigations were performed at the night of the surgical procedure. In the pre-induction room, midazolam (1–3 mg IV) was used as a premedication. Fentanyl (5–6 g/kg), propofol (2 mg/kg), and rocuronium (0.6 mg kg–1) were used to induce anaesthesia, which was maintained with 1%-2% isoflurane. The heart rate and blood pressure were maintained within 20% of baseline levels. After intravenous catheterization and endotracheal intubation, arterial and central venous catheters were inserted. Pulse oximetry, esophageal temperature, and invasive arterial blood pressure by cannulating the radial and/or femoral artery to evaluate beat-to-beat changes in blood pressure with a 5-lead electrocardiogram with automatic ST segment analysis, transesophageal echocardiography, and coagulation profile monitoring using activated clotting time.
Nerve Block and Grouping
After induction of anesthesia, patients were assigned to either the transversus group (T group) or general anesthesia (GA) group at random (N group) using a computer-generated random number in various block sizes in a 1:1 ratio. Randomization was performed using the SAS statistical package version 9.3 (SAS Institute, Cary, NC, USA) by a statistician who was not involved in the study.
Patients in the T group (n=30) received a bilateral TTPB with general anesthesia and 15 mL of 0.25% bupivacaine administered on either side. The patient was placed in the supine position and after proper sterilization, a 12 L-RS linear probe of the Sonosite M Turbo ultrasonography system was used prior to surgical incision (National Electrical Manufacturers, USA) and positioned in the sagittal plane under the clavicle lateral to the sternal edge and the ribs were counted by sliding the probe downward till the fifth rib was encountered. The probe was placed horizontally over the fourth intercostal space to identify the internal mammary artery, transverse thoracic (TT) and internal intercostal muscles(II) as shown in Figure 1A. The probe then rotated vertically to identify internal mammary artery in parasagittal view as seen in Figure 1 (B). After that the probe was slid more laterally to identify transverse thoracic plane between II and TT muscles Figure 1C. A 20-gauge Tuohy needle was advanced using inplane technique from caudal to cranial and its tip was adjusted in the transverse thoracic plane between the IIM and the TTM. To identify this plane, 1 mL of normal saline was injected, followed by 15 mL of 0.25% bupivacaine on each side following intermittent aspiration, monitoring of the LA spread and pressure on the pleura to confirm the accurate injection (Figure 1). To avoid unintended arterial puncture and subsequent bleeding, it is critical to identify the internal mammary artery (IMA), which is a hypoechoic pulsatile structure. Proper visualization of the IMA can also help with the block. Patients in the GA group (n=30) received a bilateral ultrasound-guided TTPB technique combined with general anesthesia, but instead received 15 mL saline (control) on either side. The TTPB approach was used in both groups, along with general anesthesia. A single expert anesthetist performed all the blocks. A pharmacist who was uninformed of the nature of the study produced drug packs prior to the start of the study. Additional 0.5–1 micrograms/kg IV fentanyl dosages were administered if hemodynamic abnormalities, such as elevated blood pressure or severe tachycardia, were observed. All cardiac surgical techniques included medial sternotomy.
Recovery and Postoperative
After the cardiac surgical procedure, all patients were moved to the ICU to maintain hemodynamics, control bleeding, and correct hemoglobin levels, serum electrolytes, and acid-base balance. Standard postoperative analgesia was accomplished using acetaminophen (1 gm/6 h).
All patients received postoperative care according to the protocol, which was implemented by well-trained, qualified bedside nurses who were overseen 1:1 by well-trained ICU specialists. When the patient was able to maintain spontaneous breathing following extubation, all patients were extubated when deemed clinically appropriate according to the local ICU procedure by the ICU staff. The patients were encouraged to sit in a chair and move around with the help of health care workers in the ICU, after which the physiotherapist ensured the enhancement of the patients’ mobility and rehabilitation until they were discharged.
Patient demographics, medical status before surgery, left ventricular function, and surgical data (total ischemia duration and number of grafts) were recorded.
Measurements
The percentage of patients requiring additional doses of morphine was the primary outcome of the study. The secondary outcomes included the total dose of postoperative morphine consumed, postoperative visual analogue pain scores obtained after patient extubation for pain assessment at rest (0 = no pain, 10 = maximum unbearable pain) were recorded at the time of extubation, and at 8h, 12 h,18 h and 24 h postoperatively. Pain scores >4 were recorded, and patients were given morphine (0.05 mg/kg) administered by a physician who was blinded to the nature of the study. Time needed for first rescue analgesic, postoperative mean blood pressure, and heart rate were recorded in addition to extubation time, length of ICU stay, and incidence of complications related to the technique such as hemothorax or pneumothorax, arrhythmias, and LA toxicity. The endpoints were unstable medical conditions such as difficult weaning from cardiopulmonary bypass, significant postoperative bleeding that necessitated re-exploration. All difficulties were dealt with in accordance with surgical and medical protocols.
Sample Size Calculation
After accounting for a 20% dropout rate, software for statistics and data science (Stata program version 10; Stata Corp LLC, Texas, USA) revealed that 60 patients (30 per arm) were required (setting an alpha error of 5% and power of 90%). The percentage of patients who required extra analgesia (pentazocine) within 24 h after surgery was much lower in the T group (57%) than in the GA group8 (94%).
Statistical Analysis
SPSS Statistics version 23 (IBM Corp., Armonk, NY, USA) was used to analyze the data. The mean and standard deviation were used to represent normally distributed numerical data, whereas the median and interquartile range were used to represent skewed data. The number, percentage, or ratio was used to present qualitative data. An unpaired t-test was used to compare normally distributed numerical data. The Mann–Whitney test was used to compare skewed numerical data, and Chi-square test was used to analyze qualitative data. Statistical significance was defined as a P<0.05.
Results
This research was conducted by researchers from Ain Shams University Hospital from May to August 2021. As illustrated in the CONSORT flow diagram, a total of 60 patients were enrolled and analyzed in this study (Figure 2).
No significant difference was observed between the study groups in terms of demographic, surgical, and preoperative data (Table 1). At the extubation time and 18 h postoperatively, pain scores were similar between the study groups; on the other hand, pain scores were significantly lower for the T group than the GA group at 8, 12, and 24 h postoperatively, P<0.001 (Table 2). The total dose of postoperative morphine required was significantly smaller in the T group than in the GA group, and the time to first analgesic requirement was markedly longer in the GA group (P<0.001) (Table 3). The percentage of patients requiring additional doses of morphine was higher in the GA group than in the T group (P<0.015) (Table 3).
 |
Table 1 Demographic Data, Surgical Data and Comorbidities |
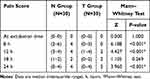 |
Table 2 Postoperative Pain Scores |
 |
Table 3 Total Postoperative Morphine Dose, Time to First Analgesic Dose and Percentage of Patients Receiving Extra Doses of Morphine |
Postoperative mean blood pressure and pulse rate were lower in the T group than in the GA group (P<0.001) (Table 4). The ventilation time was significantly longer in the GA group (P<0.001) (Table 4). The need for inotropic support was comparable between groups (Table 4). ICU stay length was significantly shorter in the T group (p <0.001) (Table 5). Postoperative complications such as pneumothorax, arrhythmia, LA toxicity, and skin infection were not significantly different between the study groups. There were no recorded cases of hemothorax or anaphylactic shock (Table 5).
 |
Table 4 Postoperative Hemodynamic Values, Need for Inotropic Support and Ventilation Time |
 |
Table 5 ICU Stay Length and Postoperative Complications |
Discussion
This study investigated the effectiveness of TTPB in the management of postoperative pain after cardiac surgery in adults with a median sternotomy.
The results of this prospective study showed that in the first 24 h after surgery, the percentage of patients needing extra morphine doses, postoperative morphine use, pain scores, and first analgesic requirement were significantly lower in the T group than in the GA group. Ventilation time and ICU stay were significantly shorter in the T group. There were no significant differences in postoperative complications between the study groups.
Earlier studies reported that post-sternotomy pain was conducted through the T2-T6 intercostal nerves; thus, blocking these nerves can efficiently control sternotomy-induced pain and reduce ICU and hospital stay length.4
In a study by Chaudhary et al, pediatric patients scheduled for cardiac surgery received parasternal block to block the T3-T6 intercostal nerves prior to sternal closure. They found that ventilation time was significantly shorter.9 In addition, pain scores and postoperative opioid requirements were significantly lower.9 These results support the findings of the present study.
A retrospective study by Ueshima et al who underwent single-shot TTPB for patients undergoing cardiac surgery through sternotomy, revealed fentanyl doses as rescue analgesics and pain scores were significantly reduced. These findings are consistent with ours.6
Kendigelen et al demonstrated that TTPB has a duration of more than 48 h because it is one of the interfascial blocks known for prolonging analgesia.10
After reviewing the literature, no complications related to TTPB have been reported, such as hemothorax, pneumothorax, wound infection, or hematoma.11
Previous studies reported that a large volume of diluted LA must be injected to ensure adequate diffusion of the drug and increase its efficacy without exceeding the maximum dose.12
A retrospective study by Cakmak et al studied the analgesic efficacy of TTPB in pediatric patients undergoing congenital cardiac surgery through median sternotomy.13 They found that pain scores and postoperative fentanyl doses were significantly lower in the T group than in the non-T group.13 Extubation time was significantly shorter in the T group (p<0.001). These results are consistent with the findings of the present study.
Severe postoperative pain following cardiac surgery lasts for 1–7 days originally caused by median sternotomy, as mentioned by Mueller et al.1 In addition, Lahtinen et al reported that 75% of patients experienced postoperative chest pain.14
The superficial technique of TTPB reduces the incidence of bleeding, especially with heparinization and the presence of coagulopathy.15
Earlier studies showed that the optimal place of administration of LA was the T4–T5 intercostal space because it resulted in better spread from the manubrium to the fifth intercostal space than injection at the T3-T4 intercostal space.16
The duration of action of the TTB can last approximately 24 h postoperatively because of the roughness of the TTM and LA spread intramuscularly; thus, its absorption is slower.17
A study by Ueshima et al studied 299 patients receiving TTPBs and reported that there were only two cases of mild skin infection at the puncture site of the block.18
Satoru et al studied single-shot TTPB efficacy in adult patients undergoing elective cardiac surgery. They revealed that pain scores were significantly lower in the block group than in the control group. On the other hand, 24-hour total hydromorphine doses were similar in both groups, unlike the current study that showed lower morphine doses required for the block group.19
Ueshima et al investigated the effectiveness of TTB in female patients undergoing breast surgery and found that the pain scores as well as the number of patients requiring further doses of analgesics were lower in the T group than in the GA group.8
A study by Abd Elbaser et al20 performed TTB in pediatric patients undergoing cardiac surgery with median sternotomy, and found that postoperative fentanyl requirements were significantly lower in the T group than in the saline group, and pain scores were significantly lower in the T group at all time points. These findings are consistent with our results.
There are few limitations to the present study. Firstly, the efficiency of TTPB in patients undergoing high risk cardiac procedures was not determined in this study. Also, the sample size was modest, thus necessitating more clinical trials with a larger number of patients to identify the occurrence of rare side effects and we did not record any failures in the blocks because the blocks were delivered under ultrasound guidance by an expert.
Lastly, the blocks were performed after induction of anesthesia, so the sensory levels could not be measured.
Conclusion
For adult patients undergoing heart surgery, TTPB offers sufficient postoperative pain control, resulting in lower pain scores, lower postoperative analgesic requirements, faster extubation time, and shorter ICU stay length without any major consequences.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mueller XM, Tinguely F, Tevaearai HT, et al. Pain location, distribution, and intensity after cardiac surgery. Chest. 2000;118(2):391–396. doi:10.1378/chest.118.2.391
2. Wolf AR, Jackman L. Analgesia and sedation after pediatric cardiac surgery. Paediatr Anaesth. 2011;21:567–576. doi:10.1111/j.1460-9592.2010.03460.x
3. B€osenberg A. Neuraxial blockade and cardiac surgery in children. Pediatr Anesth. 2003;13:559–560. doi:10.1046/j.1460-9592.2003.00960.x
4. Raj N. Regional anesthesia for sternotomy and bypass—Beyond the epidural. Paediatr Anaesth. 2019;29:519–529. doi:10.1111/pan.13626
5. Ueshima H, Kitamura A. Blocking of multiple anterior branches of intercostal nerves (Th2-6) using a transversus thoracic muscle plane block. Reg Anesth Pain Med. 2015;40:388. doi:10.1097/AAP.0000000000000245
6. Ueshima H, Hara E, Marui T, Otake H. The ultrasound-guided transversus thoracic muscle plane block is effective for the median sternotomy. J Clin Anesth. 2016;29:83. doi:10.1016/j.jclinane.2015.10.014
7. Fuji S, Roche M, Jones PM. Transversus thoracis muscle plane block in cardiac surgery: a pilot feasibility study. Reg Anesth Pain Med. 2019;44:556–560. doi:10.1136/rapm-2018-100178
8. Ueshima H, Otake H. Addition of transversus thoracic muscle plane block to pectoral nerves block provides more effective perioperative pain relief than pectoral nerves block alone for breast cancer surgery. BJA. 2017;118(3):439–443. doi:10.1093/bja/aew449
9. Chaudhary V, Chauhan S, Choudhury M, et al. Parasternal intercostal block with ropivacaine for postoperative analgesia in pediatric patients undergoing cardiac surgery: a double-blind, randomized, controlled study. J Cardiothorac Vasc Anesh. 2012;26:439–442. doi:10.1053/j.jvca.2011.10.012
10. Kendigelen P, Tütüncü C, Ashyralyyeva G, et al. Transversus abdominis plane (TAP) block for postoperative analgesia in neonates and young infants: retrospective analysis of a case series. TAP blocks in neonates and young infants. Minerva Anestesiol. 2017;83:282–287. doi:10.23736/S0375-9393.16.11420-8
11. Ueshima H, Otake H. Ultrasound guided transversus thoracic muscle plane block: complication in 299 consecutive cases. J Clin Anesth. 2017;41:60. doi:10.1016/j.jclinane.2017.03.056
12. Chin KJ. Thoracic wall blocks: from paravertebral to retrolaminar to serratus to erector spinae and back again—A review of evidence. Best Pract Res Clin Anaesthesiol. 2019;33:67–77. doi:10.1016/j.bpa.2019.02.003
13. Cakmak M, Isik O. Transversus thoracic muscle plane block for analgesia after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2020;2:1–7.
14. Lahtinen P, Kokki H, Hynynen M. Pain after cardiac surgery: a prospective cohort study of 1-year incidence and intensity. Anesthesiology. 2006;105(4):794–800. doi:10.1097/00000542-200610000-00026
15. Bignami E, Castella A, Pota V. Perioperative pain management in cardiac surgery: a systematic review. Minerva Anestesiol. 2018;84(4):488–503. doi:10.23736/S0375-9393.17.12142-5
16. Ueshima H, Otake H. Where is an appropriate injection point for an ultrasound-guided transversus thoracic muscle plane block? J Clin Anesth. 2016;33:190–191. doi:10.1016/j.jclinane.2016.03.057
17. Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006;103:703–708. doi:10.1213/01.ane.0000230603.92574.4e
18. Ueshima H, Otake H. Ultrasound-guided transversus thoracic muscle plane block. Complication in 299 consecutive patients. Clin Anesth. 2017;41:60.
19. Fujii S, Roche M, Jones PM, Vissa D, Bainbridge D, Zhou JR. Transversus thoracic muscle plane block in cardiac surgery: a pilot feasibility study. Reg Anesth Pain Med. 2019;44(5):556–560. doi:10.1136/rapm-2018-100178
20. Abdelbaser II, Mageed NA. Analgesic efficacy of ultrasound guided bilateral transversus thoracis muscle plane block in pediatric cardiac surgery: a randomized, double-blind, controlled study. J Clin Anesth. 2020;67:110002. doi:10.1016/j.jclinane.2020.110002.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


