Back to Journals » Clinical Ophthalmology » Volume 17
Evaluation of Surgical Requirements and Competencies of the Saudi Ophthalmology Training Program in a Tertiary Eye Specialist Hospital- A Cross-Sectional Study
Authors Bin Helayel H , Almazyad EM , Almazyad LM , Qadi R, Almubaiyd A, Al-Shahwan S
Received 21 March 2023
Accepted for publication 27 July 2023
Published 16 August 2023 Volume 2023:17 Pages 2373—2382
DOI https://doi.org/10.2147/OPTH.S411239
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Halah Bin Helayel,1 Enmar Mazyad Almazyad,1 Laith Mazyad Almazyad,2 Ruba Qadi,2,3 Alhanoof Almubaiyd,2,4 Sami Al-Shahwan2
1Anterior Segment Division, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 2Fellowship and Residency Training Program, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 3Ophthalmology Department, King Abdulaziz Specialist Hospital, Taif, Saudi Arabia; 4Ophthalmology Department, King Saud Medical City, Riyadh, Saudi Arabia
Correspondence: Halah Bin Helayel, Anterior Segment Division, King Khaled Eye Specialist Hospital, Uruba Road, Riyadh, 11462, Saudi Arabia, Tel +966114821234, Email [email protected]
Purpose: To evaluate the adequacy of a Saudi ophthalmology training programs in achieving the competencies outlined by the Saudi Commission for Health Specialties (SCFHS) and the Accreditation Council for Graduate Medical Education (ACGME) and to assess resident satisfaction with their training.
Methods: A cross-sectional survey was sent electronically to all trainees (n=50) enrolled in the King Khaled Eye Specialist Hospital (KKESH) ophthalmology training program by email and messaging app (Whatsapp). The survey was sent between January 20, 2021, and January 30, 2021. It evaluated the level of satisfaction with surgical training and skills. The surgical logbooks of all trainees were extracted, and identifiers were removed. Then they were compared with SCFHS and ACGME curriculums for ophthalmology training.
Results: Out of 50 invitees, 47 returned the questionnaire. All trainees were confident they could meet surgical requirements by the end of their training. Most trainees were satisfied (n=29, 61.7%) with their performance in core competency requirements. There was no difference between female and male trainees’ comfort levels when performing surgical steps in core competency requirements (P=0.2). Senior trainees seem more satisfied with their performance, especially in core competency requirements (P=0.087). All trainees practice at the wet lab and a virtual reality simulator to improve their skills. Obstacles faced during training were highlighted, including low exposure in the operating theater (n=18, 37.50%), competition on cases (n=5, 10.42%), attending surgeons not willing to teach (n=5, 10.42%), COVID-19 pandemic (n=5, 10.42%), and complex cases (n=4, 8.33%).
Conclusion: The outcomes of the current study indicate that trainees at KKESH were adequately satisfied with their surgical training in general. Also, competencies outlined by both the SCFHS and the ACGME were adequately fulfilled.
Keywords: ophthalmology training, curriculum, surgical training, medical education
Introduction
Training resident ophthalmologists is a challenging task for both faculty and trainees.1 Teaching surgical knowledge must be a high priority in any successful residency program.1 All surgical training programs aim to enhance residents’ surgical judgment, confidence, and skills to ensure patient safety and well-being.2
Technological and surgical advancements within ophthalmology have constantly changed the competencies required of trainee surgeons.3 Additionally, there are major challenges in teaching surgery on live patients, such as ethical concerns, the nature of ophthalmic microsurgery, and dealing with complications. Therefore, a surgical training program must balance the need for trainees to gain surgical competency and ensure patient safety at the same time.1,4,5 The ophthalmology residency program began in 1984 in Saudi Arabia.6 It consists of four years. The program curriculum includes an introductory science course in the first two months of the first year, followed by subspecialty lectures, conferences, journal clubs, weekly grand rounds, and case presentations. Hence, the curriculum allows trainees to build their clinical and surgical knowledge. In addition, to improving the microsurgical skills of trainees, our center engaged in proficiency-based virtual reality training and wet lab courses.7 The Saudi Commission for Health Specialties (SCFHS) and, in some centers, the Accreditation Council for Graduate Medical Education (ACGME) regulate most training programs in Saudi Arabia. The scientific review committee regularly monitors compliance with training requirements. Also, SCFHS and ACGME set the minimum number of specific surgical and office-based procedures in their curriculums that must be completed before the end of the training and sitting for the board certification examination. This is the format in many ophthalmology-training programs. Accordingly, assessment tools have been developed to help the supervising surgeon objectively assess the trainee resident’s competency while performing surgery. Even more importantly, resident feedback on their training and level of satisfaction is a key element for continuous improvement, perfecting the program outcomes, and graduating competent, well, established future ophthalmologists.
Hence, this study aims to establish the patterns in the cumulative surgical experience of ophthalmology trainees in Saudi Arabia and assess trainee satisfaction with their surgical training. Additionally, this study evaluated the adequacy of the Saudi ophthalmology training programs in achieving the objectives outlined by both SCFHS and ACGME regarding surgical competency.
Methods
The ethical committee at King Khaled Eye Specialist Hospital (KKESH), Riyadh, Saudi Arabia, approved this study (study number: 21071-P). This study adhered to the tenets of the Declaration of Helsinki. A questionnaire was sent to all residents (n-50) enrolled in the KKESH ophthalmology training program, including batches that graduated in September 2019 and September 2020 between January 20, 2021, and January 30, 2021. Participation was voluntary, and the study protocol ensured the complete anonymity of participants. Participants included in this study provided informed consent. The questionnaire (Appendix 1) consisted of 19 questions that covered mainly age, gender, and level of training. Additionally, there were questions regarding the satisfaction with surgical training at KKESH, obstacles the residents faced that hindered their progression, and areas they believe need improvement. Also, we inquired about how frequently the residents used the surgical wet lab and which procedures they practiced there.
Additionally, through the hospital training portal, the surgical logbooks of all trainees were extracted, and identifiers were removed. Then they were compared with SCFHS and ACGME curriculums for ophthalmology training. The primary outcome was finding the cumulative surgical experience of ophthalmology trainees while the secondary outcome variable was to assess the residents’ satisfaction level with their surgical training.
Statistical Analysis
All analyses were performed using Stata version 16.1 (StataCorp, College Station, Texas, 77845, USA). Qualitative variables such as gender and level of training were presented as numbers and percentages. Quantitative variables such as age, frequency of wet lab visits per week, and the number of surgeries were presented as mean and standard deviation. Fisher’s exact test was used to find associations between categorical variables, and one-way ANOVA was used to compare multiple means. A P-value less than 0.05 was considered statistically significant.
Results
Of the 50 total current and previous KKESH ophthalmology residents, 47 (94%) returned the questionnaire. The mean age of the participants was 27.64±1.9 years (range:25–31). Out of 47 participants, 23 (48.94%) were females. Fifteen respondents (31.91%) finished their residency training and joined subspecialty fellowship training. The remaining 32 (68.09%) were enrolled in the residency training program. Table 1 summarizes the distribution of respondents among training levels. Figure 1 summarizes the desired subspecialties among the participants.
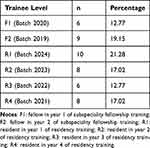 |
Table 1 The Distribution of Respondents Among Training Levels (n=47) |
 |
Figure 1 The desired subspecialty of ophthalmology residents (n=47). |
Participants were asked if they were confident that they could meet their surgical requirements. Twenty-four (51.07%) trainees reported they were confident of meeting the requirements by the end of their training. Out of 47, twenty trainees (42.55%) were somewhat confident, and only 3 (6.38%) were not confident at all that by the end of their training that they would be able to meet the surgical requirements. Figure 2 presents the residents’ satisfaction level with case volume/ exposure, case complexity, case variety, quality of teaching, didactic surgical courses, surgical skills they developed, videotapes of their surgical cases, and virtual surgical simulation.
 |
Figure 2 Satisfaction levels with surgical training of ophthalmology residents (n=47). |
Seven trainees reported being extremely satisfied that they could comfortably perform surgical steps in core competency requirements. Most trainees were very satisfied (29:61.70%). Only 9 (19.15%) stated they were slightly satisfied with their performance in core competency requirements, and two (4.26%) were not satisfied at all. The study participants were queried whether they felt competent in performing different ophthalmic assessments and procedures. Their responses are summarized in Table 2.
 |
Table 2 Responses of Participants who felt they are competent in Performing Ophthalmic Assessments and Procedures (n=47) |
There were no differences between genders in the comfort level when performing surgical steps in core competency requirements (P=0.2). However, male trainees were statistically more confident that they would meet the surgical requirements by the end of their training than female trainees (P=0.01).
The difference between training level and resident satisfaction with their training in certain aspects was assessed. For example, there was no difference between junior and senior trainees regarding training on virtual surgical simulators (P=0.66), using videotapes to review surgical cases (P=0.90), training in the wet lab (P=0.26), given didactic surgical courses (P=0.44), quality of teaching (P=0.40), cases variety (P=0.33), case complexity (P=0.55), case volume and exposure (P=0.99). However, compared to junior trainees, senior trainees (including the recent two batches that graduated) were slightly more confident they could meet surgical requirements by the end of their training (P=0.32). Also, senior trainees seemed somewhat more satisfied with their performance, especially in core competency surgical requirements (P=0.087).
Using data obtained through residency office archived data, Table 3 illustrates the trainees’ performance compared to SCFHS and ACGME surgical requirements.
 |
Table 3 Trainees’ Performance Compared to Saudi Commission for Health Specialties and Accreditation Council for Graduate Medical Education Surgical Requirements |
We observed the same trend that senior trainees who completed training (batch 2019 and 2020) performed more cases compared to their junior colleagues. This difference was evident in the cornea, conjunctiva, and refractive procedures such as primary repair (P<0.001), lid surgeries including lid laceration repair (P=0.002), pan-retinal photocoagulation (PRP) (P<0.001), intravitreal injection (P<0.001), YAG laser capsulotomy (P<0.001), YAG laser peripheral iridotomy (P<0.001), vitreoretinal procedures (P<0.001), glaucoma filtering surgeries (P<0.001), probing ± stent placement (P<0.001), assisting in dacryocystorhinostomy (DCR) (P=0.001), evisceration or enucleation (P=0.007), performing in strabismus surgery (P=0.001), and minor procedures such as chalazia excision and removal of superficial corneal foreign bodies (P<0.001).
All participants responded “YES” when asked about attending the wet lab and virtual surgical simulator to practice surgical techniques. The mean visit weekly to the wet lab was 1.74±0.9 days (range: 1–4 days). The most common surgical procedures they commonly performed in the wet lab were: suturing (37:40.22%), phacoemulsification (32:34.78%), capsulorrhexis training (13: 9.77%), and simulator use for phacoemulsification training (4:4.35%). The remaining responses indicated that the trainees go to the wet lab to practice performing extracapsular cataract extraction (ECCE) (3:3.26%), glaucoma procedures such as Ahmed valve placement (1:1.09%), vitreoretinal procedures (1:1.09%) and keratoplasty (2:2.17%). Some trainees responded that they went to the wet lab to learn how to adjust the microscope and handle instruments properly inside the eye.
Figure 3 illustrates the obstacles the trainees perceived they faced during their surgical training.
 |
Figure 3 The perceived obstacles that ophthalmology residents faced during their surgical training. |
Figure 4 presents the trainee responses regarding the procedures they needed to improve further.
Discussion
The study results showed that most ophthalmology trainees at a major training center in Saudi Arabia were satisfied with their surgical training. However, there were some inconsistencies when examining each subspecialty requirement and their comfort level in performing their assessment and procedures. Compared to the surgical requirements proposed by SCFHS and ACGME, our trainees are performing more cataract surgery cases, glaucoma laser procedures than lid and orbital surgeries. The proposed reasons behind these differences are explained below under the obstacles reported by the trainees.
We explored the differences in responses between the male and female trainees regarding their satisfaction with their surgical training, and there were no statistically significant differences in this regard.
Gender disparities in ophthalmology have been previously described in several studies. This disparity was evident in surgical exposure, allocated subspecialty fellowship seats, editor-in-chief, and society president positions, last authorship and citation in published articles during the last decade, and presentations in subspecialty conferences.8–12 In Gong et al’s report, investigators found that female ophthalmology trainees performed fewer surgical cases than their male colleagues.8
Female surgical trainees showed lower confidence levels in previous reports.13 A similar observation was noticed among female medical students compared to their male peers.13 Similarly, male ophthalmology residents were statistically more confident that they would meet the surgical requirements than their female colleagues.
Developing confidence is crucial for trainees to feel satisfied with their training. The confidence level can influence the decision to continue in the specialty, leave it, or pursue additional training. In our study, we looked at factors influencing satisfaction with various aspects of training based on the training level. We found statistically significantly higher satisfaction among senior residents with their performance, specifically in the core competency requirements, compared with the junior residents. Additionally, the survey results indicated that senior residents performed a greater number of overall cases, which was a consistent trend in data analysis. This difference was evident, particularly in the cornea, conjunctiva, and refractive procedures, including cases of primary repair. The trend of senior trainees performing more cases than the junior residents varied statistically when the cases were performed as the trainees being the main surgeon or assistant surgeons. Similar findings were observed previously as the trainees advanced in their training and performed more cases; they became more confident.14–16 In results of the current survey indicated that all the trainees attended the wet lab and simulation to practice surgical techniques. The most common procedures performed in the wet lab were suturing, phacoemulsification, and capsulorrhexis. The surgical simulator was used for phacoemulsification training. These findings are consistent with the conclusion of an earlier study by Alwadani (2018), who considered wet lab training an important component of the ophthalmology training program in academic ophthalmology training programs in the Kingdom of Saudi Arabia (KSA).17 Traditionally, the trainees grasped technical skills while observing and assisting the attending surgeon in the operating room. However, this method is not optimal, especially in ocular surgeries, as we deal with sensitive organ, and most patients undergo surgery under local anesthesia while awake. Such a situation is considered stressful for the patient, trainee, and attending surgeon. Teaching basic and advanced surgical skills in the wet lab before starting on patients can overcome this issue.18,19 Also, this can alleviate trainee distress, anxiety, or frustration and allow tutors to provide feedback to their trainees to enhance skills and improve outcomes.14
The major obstacles faced by the trainees in the current study were, in descending order: low exposure in the operating theatre secondary to competition on cases, a high number of trainees in each team, faculty resistance to training, and rotation timing. In addition, surgical lists contained complex and difficult cases that did not fit the trainee level. Residents also indicated that the COVID-19 pandemic reduced exposure to surgical cases. This was clearly observed when comparing the number of cases performed by residents who graduated prior to or during the pandemic (batch 2019 and 2020) compared to the later batches. The finding of reduced trainee exposure due to the COVID-19 pandemic concurs with an earlier study by Alahmadi et al, who reported disrupted clinical and surgical training of ophthalmology residents in the KSA due to the pandemic.7 Similar findings were also obtained in a global-level study that found a reduction in the clinical and surgical activity of ophthalmology trainees after the COVID-19 pandemic.20
This study surveyed the procedures that required further improvement among the trainees. The most frequently mentioned procedures included phacoemulsification, strabismus surgery, oculoplastic procedures, glaucoma procedures, suturing techniques, capsulorrhexis, secondary IOL implantation techniques, evisceration, enucleation, and keratoplasty.
Surgical skills related to strabismus surgery have been highly emphasized by the Royal College of Ophthalmologists of the United Kingdom and were rightly identified by the trainees as an area warranting improvement.21 The trainees identified phacoemulsification as a skill that requires further improvement and is consistent with previous research findings.1,22,23 A study on phacoemulsification surgeries by residents in the Philippines also emphasized that more cases are needed to meet the competency requirements.22 Improving surgical training for ophthalmology residents has been highly emphasized in the literature.1,23 Overall, the results of the current study indicate that achieving surgical competencies is perceived as very important for ophthalmological trainees. In addition, the study found the trainees to be adequately satisfied with their surgical exposure during their training despite the obstacles posed by the COVID-19 pandemic. These findings are in contrast with an earlier study on an ophthalmological residency training program in the KSA that found trainees lacking surgical exposure during their ophthalmology residency.24
The adequate level of satisfaction expressed by the participants in the current study is consistent with earlier studies evaluating the satisfaction of ophthalmology trainees worldwide. For example, ophthalmology trainees in Canada were highly satisfied with their residency training and considered their training programs to meet international standards.25 Similarly, the trainees in Iran were found to be adequately pleased with the curriculum of their training programs.26 The ophthalmology trainees expressed the highest level of satisfaction in the United States.27 However, the current study’s findings contrast with an earlier survey of ophthalmology training in Jordan that reported most trainees were dissatisfied with their training programs.28 Similar to the current study, many studies identified obstacles in training and recommended changes to empower the residents to further achieve their competencies and improve their satisfaction with the program. For example, a Greek study recommended introducing new structured curricula, reduced interference from bureaucracy, and enhanced surgical training of ophthalmological residents.29
All trainees at our center chose to pursue fellowship training. However, we did not explore the reasons behind their decision and their subspeciality choice. Many factors were discussed previously that influence the decision of the trainee to continue fellowship training, such as prestige, lifestyle consideration, focusing their clinical practice, being known as experts in their chosen subspecialty, significant and rapid advances in the field, mastering basic and advanced surgical skills, improving confidence levels, and receiving further mentorship.30–36 Grover and Kothari discussed resident interests in continuing with fellowship training and the perception that better care can be provided with subspecialty training.34
The current study has some limitations, including the analysis being limited to trainees in a single hospital setting and a relatively small sample size. Therefore, large-scale studies evaluating trainee satisfaction and achievement of requisite competency requirements in multiple settings are recommended in the future to arrive at more generalized conclusions about the adequacy of ophthalmology training programs in meeting their objectives in different countries or from different programs within Saudi Arabia. Another limitation is that we did not inquire if any leave or approved program freeze (and duration) was taken during training, which may affect an individual resident’s case volume. This factor may explain the difference in the confidence levels between genders and the subspecialty fellowship choices.
The results of the current survey evaluating the surgical requirements and competencies demonstrated that trainees in one of the Saudi Ophthalmology training programs at a tertiary eye specialist hospital achieved competencies outlined by SCFHS and ACGME. In addition, the trainees were adequately satisfied with their training.
Ethics Approval
Ethical approval was granted by the institutional review board of the King Khaled Eye Specialist Hospital.
Consent to Participate
Participants included in this study provided informed consent.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Alfawaz AM. Ophthalmology resident surgical training: can we do better? Saudi J Ophthalmol. 2019;33(2):159–162. doi:10.1016/j.sjopt.2018.11.009
2. Dreyer EB, Volpe NJ. Eleven commandments for teaching ophthalmic surgery. Ophthalmology. 2000;107(3):415–416. doi:10.1016/S0161-6420(99)00095-0
3. Bhagat PR, Jethva J. Wet laboratory training in ophthalmology as a tool for formative assessment. Int J Appl Basic Med Res. 2022;12(4):228–233. doi:10.4103/ijabmr.ijabmr_334_22
4. Roberts KE, Bell RL, Duffy AJ. Evolution of surgical skills training. World J Gastroenterol. 2006;12(20):3219–3224. doi:10.3748/wjg.v12.i20.3219
5. Roberts TV, Plant AJH, Hodge C. Ophthalmic surgery teaching. Ann Eye Sci. 2019;4:25. doi:10.21037/aes.2019.07.01
6. AlEnezi SH, Alfawaz AM, Al Owaifeer AM, Althiabi SM, Tabbara KF. Assessment of ophthalmology residency programs in Saudi Arabia: a trainee-based survey. J Med Educ Curric Dev. 2019;6:2382120519855060. doi:10.1177/2382120519855060
7. Alahmadi AS, Alhatlan HM, Bin Helayel H, Khandekar R, Al Habash A, Al-Shahwan S. Residents’ perceived impact of COVID-19 on Saudi ophthalmology training programs-a survey. Clin Ophthalmol. 2020;14:3755–3761. doi:10.2147/OPTH.S283073
8. Gong D, Winn BJ, Beal CJ, et al. Gender differences in case volume among ophthalmology residents. JAMA Ophthalmol. 2019;137(9):1015–1020. doi:10.1001/jamaophthalmol.2019.2427
9. Dotan G, Qureshi HM, Gaton DD. Chairs of United States academic ophthalmology departments: a descriptive analysis and trends. Am J Ophthalmol. 2018;196:26–33. doi:10.1016/j.ajo.2018.08.016
10. Camacci ML, Lu A, Lehman EB, Scott IU, Bowie E, Pantanelli SM. Association between sex composition and publication productivity of journal editorial and professional society board members in ophthalmology. JAMA Ophthalmol. 2020;138(5):451–458. doi:10.1001/jamaophthalmol.2020.0164
11. Kramer PW, Kohnen T, Groneberg DA, Bendels MHK. Sex disparities in ophthalmic research: a descriptive bibliometric study on scientific authorships. JAMA Ophthalmol. 2019;137(11):1223–1231. doi:10.1001/jamaophthalmol.2019.3095
12. Patel SH, Truong T, Tsui I, Moon JY, Rosenberg JB. Gender of presenters at ophthalmology conferences between 2015 and 2017. Am J Ophthalmol. 2020;213:120–124. doi:10.1016/j.ajo.2020.01.018
13. Van Boerum MS, Jarman AF, Veith J, et al. The confidence gap: findings for women in plastic surgery. Am J Surg. 2020;220(5):1351–1357. doi:10.1016/j.amjsurg.2020.06.037
14. Crespi-Flores VG, Minguini N, Temporini ER, Carvalho KM. Strabismus surgery learning for ophthalmology residents of university service. Arq Bras Oftalmol. 2012;75(3):188–191. doi:10.1590/S0004-27492012000300008
15. Elfenbein DM. Confidence crisis among general surgery residents: a systematic review and qualitative discourse analysis. JAMA Surg. 2016;151(12):1166–1175. doi:10.1001/jamasurg.2016.2792
16. Bucholz EM, Sue GR, Yeo H, Roman SA, Bell RH Jr, Sosa JA. Our trainees’ confidence: results from a national survey of 4136 US general surgery residents. Arch Surg. 2011;146(8):907–914. doi:10.1001/archsurg.2011.178
17. Alwadani S. Cataract surgery training using surgical simulators and wet-labs: course description and literature review. Saudi J Ophthalmol. 2018;32(4):324–329. doi:10.1016/j.sjopt.2018.01.003
18. Binenbaum G, Volpe NJ. Ophthalmology resident surgical competency: a national survey. Ophthalmology. 2006;113(7):1237–1244. doi:10.1016/j.ophtha.2006.03.026
19. Lee AG, Beaver HA, Greenlee E, et al. Teaching and assessing systems-based competency in ophthalmology residency training programs. Surv Ophthalmol. 2007;52(6):680–689. doi:10.1016/j.survophthal.2007.08.021
20. Ferrara M, Romano V, Steel DH, et al. Reshaping ophthalmology training after COVID-19 pandemic. Eye. 2020;34(11):2089–2097. doi:10.1038/s41433-020-1061-3
21. Pilling RF, Bradbury JA, Reddy AR. Strabismus surgical skills assessment tool: development of a surgical assessment tool for strabismus surgery training. Am J Ophthalmol. 2010;150(2):275–278 e272. doi:10.1016/j.ajo.2010.03.007
22. Umali MIN, Castillo TR. Operative time and complication rates of resident phacoemulsification surgeries in a national university hospital: a five-year review. Clin Ophthalmol. 2020;14:4065–4072. doi:10.2147/OPTH.S283754
23. Ezra DG, Chandra A, Okhravi N, Sullivan P, McDonnell P, Lee J. Higher surgical training in ophthalmology: trends in cumulative surgical experience 1993–2008. Eye. 2010;24(9):1466–1473. doi:10.1038/eye.2010.54
24. Al Saedi NG, Al-Sharif EM, Mousa A, Alsuhaibani AH. The impact of surgical training on the practice of recently graduated ophthalmologists at Riyadh’s ophthalmology residency program. Saudi J Ophthalmol. 2019;33(4):319–325. doi:10.1016/j.sjopt.2019.08.001
25. Zhou AW, Noble J, Lam WC. Canadian ophthalmology residency training: an evaluation of resident satisfaction and comparison with international standards. Can J Ophthalmol. 2009;44(5):540–547. doi:10.3129/i09-155
26. Mostafaei A, Hajebrahimi S. Perceived satisfaction of ophthalmology residents with the current Iranian ophthalmology curriculum. Clin Ophthalmol. 2011;5:1207–1210. doi:10.2147/OPTH.S18907
27. Abdelfattah NS, Radwan AE, Sadda SR. Perspective of ophthalmology residents in the United States about residency programs and competency in relation to the International Council of Ophthalmology guidelines. J Curr Ophthalmol. 2016;28(3):146–151. doi:10.1016/j.joco.2016.06.001
28. Al-Salem KM, Al-Sarayra FA, Abu Al-Dabaat M, et al. Ophthalmology residency training in Jordan: an evaluation of quality and comparison with international standards. Int J Ophthalmol. 2014;7(5):898–904. doi:10.3980/j.issn.2222-3959.2014.05.28
29. Lamprogiannis L, Tzamalis A, Tsaousis KT, et al. Ophthalmology training in Greece as perceived by resident ophthalmologists in the times of crisis: a National, Questionnaire-based Survey. J Curr Ophthalmol. 2020;32(1):88–93. doi:10.1016/j.joco.2019.10.001
30. Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379(9827):1749–1761. doi:10.1016/S0140-6736(12)60437-1
31. Manche E, Roe J. Recent advances in wavefront-guided LASIK. Curr Opin Ophthalmol. 2018;29(4):286–291. doi:10.1097/ICU.0000000000000488
32. Aref AA, Gedde SJ, Budenz DL. Glaucoma drainage implant surgery. Dev Ophthalmol. 2017;59:43–52.
33. Yim CK, Teng CC, Warren JL, Tsai JC, Chadha N. Microinvasive glaucoma surgical training in United States ophthalmology residency programs. Clin Ophthalmol. 2020;14:1785–1789. doi:10.2147/OPTH.S255103
34. Grover BT, Kothari SN. Fellowship training: need and contributions. Surg Clin North Am. 2016;96(1):47–57. doi:10.1016/j.suc.2015.09.003
35. Chen X, Zafar S, Srikumaran D, et al. Factors influencing post-graduate career decisions of ophthalmology residents. J Acad Ophthalmol. 2019;12(02):e124–e133.
36. Gedde SJ, Budenz DL, Haft P, Tielsch JM, Lee Y, Quigley HA. Factors influencing career choices among graduating ophthalmology residents. Ophthalmology. 2005;112(7):1247–1254. doi:10.1016/j.ophtha.2005.01.038
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

