Back to Journals » Clinical Ophthalmology » Volume 16
Evaluation of Quality of Vision and Visual Outcomes with Bilateral Implantation of a Non-Diffractive Extended Vision Intraocular Lens with a Target of Slight Myopia in the Non-Dominant Eye
Received 29 November 2021
Accepted for publication 13 January 2022
Published 25 January 2022 Volume 2022:16 Pages 183—190
DOI https://doi.org/10.2147/OPTH.S350850
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
T Hunter Newsom,1 Richard Potvin2
1Newsom Eye & Laser Center, Sebring, FL, USA; 2Science in vision, Bend, OR, USA
Correspondence: T Hunter Newsom, Email [email protected]
Purpose: To assess the visual outcomes and quality of vision of patients receiving the AcrySof® IQ Vivity™ non-diffractive extended vision intraocular lens (NDEV IOL) after uneventful cataract surgery when the non-dominant eye is targeted for slight myopia.
Design: Single site, prospective, single-arm study.
Methods: Eligible subjects interested in reducing their dependence on spectacles over a range of working distances were enrolled and followed for 3 months after the second eye surgery. Subjects were bilaterally implanted with this NDEV IOL, with a target of emmetropia in the dominant eye and a myopic refraction of − 0.75D in the non-dominant eye. At 3 months postoperative, the uncorrected and distance-corrected (with monovision) visual acuity at 40 cm, 66 cm and 4 m were recorded, along with the manifest refraction. Questionnaires related to spectacle independence, patient satisfaction and quality of vision were also administered.
Results: Data from 33 subjects were analyzed. The mean difference between eyes by subject was 0.80 ± 0.37 D. Twenty-nine of 33 (88%) subjects had a binocular uncorrected near VA of 0.2 logMAR or better. Twenty-five of 33 eyes (76%) had a binocular distance-corrected (− 0.75 D in the non-dominant eye) VA of 0.2 logMAR or better at all three test distances. Satisfaction with vision at all distances was high. The reported level of spectacle independence was higher than for the same lens without monovision. Visual disturbances were higher than has been previously reported for this lens but were not correlated to the level of monovision.
Conclusion: A target of − 0.75 D of myopia in the non-dominant eye of patients bilaterally implanted with this NDEV IOL improved near vision, increasing the rate of spectacle independence in patients relative to those targeted for bilateral emmetropia, with no correlated increases in visual disturbances.
Keywords: wavefront shaping, spectacle independence, presbyopia correction, EDOF, extended depth of focus, extended depth of vision, non-diffractive, monovision
Plain Language Summary
Patients who are having cataract surgery may be interested in reducing their need for glasses at one or more working distances. One alternative to provide good vision at distance and intermediate (eg, for computer viewing) is an extended depth of vision intraocular lens (IOL). Such an IOL can “stretch” the focal length of the eye to provide the ability to see at arm’s length, while avoiding the visual disturbances that can be associated with other IOLs that “split” light to provide different focal points. The primary interest in our study was whether subjects implanted with one such an IOL could have functional near vision if one eye were corrected to be slightly short-sighted. Results indicated that near vision could be improved with this approach, with no increase in expected visual disturbances.
Introduction
Patients presenting for cataract surgery today have a wide range of intraocular lens (IOL) options to consider, depending on their relative desire for spectacle independence and their tolerance for potential visual disturbances. Bifocal and trifocal IOLs have been shown to provide better near vision than options such as extended depth of focus (EDOF) or monofocal IOLs.1,2 Some authors have found a higher likelihood of visual disturbances with multifocal IOLs relative to previously studied EDOF lenses,2 though others report no difference.3,4 Previous EDOF and multifocal IOLs have been associated with higher rates of visual disturbances than monofocal IOLs.1,5
A commonly used option for increasing the visual range of a patient is to make one eye slightly myopic (monovision). Considerable research on monovision was conducted when monofocal contact lenses were widely adopted.6–8 Evidence suggested that anisometropia of up to 2.5 D could be tolerated by some patients, but the level of acceptance of monovision decreased with the magnitude of the anisometropia.6 Monovision with contact lenses is easily reversible, which is not the case with surgical procedures such as LASIK or cataract surgery. Perhaps for this reason the level of monovision generally targeted in LASIK has been around 1.50 D, to reduce the potential for non-adaptation.9,10 Monovision has also been successful as an option for cataract patients, though again the target refraction of 1.0 to 1.5 D of myopia is recommended, to reduce the potential for unwanted visual symptoms.11,12 With a monofocal IOL this level of monovision correction may not be sufficient to provide functional near vision. However, using an EDOF lens with a monovision correction is expected to address this, as the IOL effect and monovision offset will have a cumulative effect.
There are a number of different approaches to creating an EDOF IOL.13 Spherical aberration can be incorporated into the IOL design, but this approach can be confounded by the wide range of existing spherical aberration in the population, and pupil size, making outcomes potentially more variable.14,15 Another approach is the use of diffractive elements to produce the EDOF effect, but there may be little advantage to such an IOL design relative to a diffractive multifocal; visual disturbances may not be any lower, though near vision would be compromised.16 A third approach involves using a small aperture to extend the depth of focus, a common technique in photography.17 This approach may significantly limit the light entering the eye, so it is often used in only the non-dominant eye of patients.
A relatively recent innovation, the AcrySof® IQ Vivity™ IOL, incorporates a unique wavefront shaping technology to produce an extended depth of focus.18 It does not incorporate diffractive elements, or rely on small aperture technology, to modify the wavefront so it can be considered a non-diffractive extended vision (NDEV) IOL. The rates of visual disturbances with this NDEV IOL appear similar to those for a monofocal IOL.19 In clinical trials the intermediate and near vision were significantly better than for a monofocal IOL, but near vision was not as good as can be achieved with a multifocal IOL.19
The binocular defocus curve for this NDEV IOL19 suggests that a myopic shift of 0.75 D in one eye might be sufficient to provide better near vision to patients relative to bilateral emmetropia. A recent study of spectacle-based monovision in patients bilaterally implanted with this IOL corroborates this finding.20
The purpose of the current study was to determine how targeting a low level of myopia (0.75 D) in the non-dominant eye of subjects bilaterally implanted with this NDEV IOL affected visual acuity and range of vision, spectacle independence, quality of vision and satisfaction.
Methods
This was a prospective single-arm study of the visual outcomes and quality of vision associated with bilateral implantation of this NDEV IOL with a target of slight myopia in the non-dominant eye. The study was approved by an appropriate institutional review board (Salus IRB, Austin, TX) and registered with clinicaltrials.gov (NCT04482439). The study was conducted in accordance with the tenets of the Declaration of Helsinki and Good Clinical Practice. All subjects signed an appropriate informed consent document before being admitted to the study. Data are not available for sharing.
Eligible subjects were patients ≥40 years of age presenting for cataract surgery who were interested in reducing their dependence on spectacles at all distances, and who were deemed appropriate candidates for extended depth of focus (EDOF) lens implantation. All subjects had to meet the requirements for on-label implantation of the IOL in both eyes, with good ocular health and no pathology that would compromise visual acuity (outside of refractive error and cataract). Corneal astigmatism had to be regular and have a magnitude that could be treated with a toric or non-toric IOL. Potential acuity measured before surgery had to be 20/32 (0.2 logMAR) or better in both eyes. Eyes with prior corneal refractive surgery, macular pathology, diabetic retinopathy or previous anterior or posterior chamber surgery were excluded.
Surgical planning and IOL power calculation were performed using the surgeon’s preferred method, using the manufacturer’s a-constant from the packaging. When a toric IOL was used, planning was performed with the Alcon Barrett Toric calculator, which takes the effects of posterior corneal astigmatism into account. All subjects had cataract surgery with bilateral implantation of this NDEV IOL, using the surgeon’s usual standard of care with regard to surgical treatment and intraoperative/postoperative medication. Mile’s test was used to determine eye dominance. The dominant eye was targeted for emmetropia while the non-dominant eye was targeted for a myopic refraction close to −0.75 D. Surgical findings were recorded and any adverse events/serious adverse events (AEs/ SAEs) occurring during surgery were noted. Subjects whose surgery was not completed successfully were monitored for safety, but clinical performance data were excluded from the analysis.
The measure of primary interest was the binocular distance-corrected near (40 cm) visual acuity 3 months postoperative. In this context, distance-corrected means the dominant eye corrected for emmetropia and the non-dominant eye corrected to −0.75 D of myopia. Other measures of interest were the manifest refraction, the uncorrected and distance-corrected binocular VAs at 66 cm and 4 m and the uncorrected VA at 40 cm. All vision testing was performed using the Clinical Trial Suite from M&S Technologies (Niles, IL, USA). Spectacle independence was measured using the Patient Reported Spectacle Independence Questionnaire (PRSIQ).21 Patient satisfaction and quality of vision questionnaires were also administered. The Intraocular Lens Satisfaction (IOLSAT) questionnaire is a proprietary Alcon questionnaire that asks subjects about how well they see at various distances in bright and dim light. The Questionnaire for Visual Disturbances (QUVID) is also a proprietary Alcon questionnaire, and asks patients about the frequency, severity, and degree of bother of various visual disturbances such as glare, halos, and starbursts. These questionnaires were used in the study conducted to obtain FDA approval of the lens. All subjects were monitored for adverse events at all visits.
Results
Thirty-five subjects were successfully recruited for the study, with one lost to follow-up and one unable to complete the study due to an unrelated illness; results for 33 subjects were available for analysis. There were 21 females and 12 males in the data set, with an average age of 70.0 ± 5.5 years (range 57 to 80). The average IOL sphere power was 21 ± 2 D (range 16.5 to 25.0). Thirty-eight of the 66 implanted lenses (58%) were non-toric. There were no reported adverse events. Refractive results and visual acuity results were not statistically significantly different by type of IOL (toric or non-toric, p > 0.11 in all cases).
The distributions of the monocular refractive results for the emmetropic and monovision eyes are shown in Figure 1. The average mean refractive spherical equivalent (MRSE) was significantly different between the eye groups (0.01 ± 0.31 D in the emmetropic eyes vs −0.74 ± 0.39 D in the monovision eyes, p < 0.01). The mean difference between eyes by subject was 0.80 ± 0.37 D, with a range of 0.25 to 1.625 D. While not shown, the mean refractive cylinder was 0.42 ± 0.30 D (range 0.0 to 1.25 D), with no statistically significant difference between the emmetropic and monovision eyes (p = 0.77).
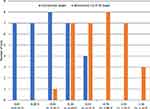 |
Figure 1 Distribution of postoperative mean spherical equivalent refraction by refractive target. |
The uncorrected visual acuity by target refraction and test distance is shown in Figure 2. While not shown, the corrected distance visual acuity (CDVA), with the monovision eye corrected to −0.75D, was statistically significant lower in the monovision eye (0.02 ± 0.07 logMAR in the emmetropic eye vs 0.17 ± 0.15 logMAR in the monovision eye, p < 0.01), as expected. CDVA was significantly better than the uncorrected distance VA by about 3 letters in both the emmetropic and monovision eyes (p < 0.01 in both cases).
 |
Figure 2 Monocular visual acuity by test distance and refractive target. Abbreviation: logMAR, log of the minimum angle of resolution. |
Figure 3 shows the binocular uncorrected and distance-corrected results by test distance. There was no statistically significant difference between the uncorrected and distance-corrected results at any distance (p > 0.32). There was a statistically significant difference in the VA by test distance. Post-hoc testing showed that the distance and intermediate results were not statistically significantly different, but the near VA was significantly lower than distance and intermediate VA (Tukey’s honestly significant difference test, p < 0.05). Eighteen of 33 subjects (55%) had an uncorrected near VA of 0.1 logMAR (20/25 Snellen) or better, while 29 of 33 (88%) had an uncorrected near VA of 0.2 logMAR (20/32 Snellen) or better. Twenty-five of 33 subjects (76%) had a distance-corrected VA of 0.2 logMAR or better at all three test distances. (Again, distance-corrected included −0.75D of monovision in the non-dominant eye.)
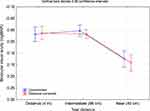 |
Figure 3 Binocular visual acuity by test distance and correction. Abbreviation: logMAR, log of the minimum angle of resolution. |
Summary results from the PRSIQ are shown in Table 1; one subject failed to complete the questionnaire. The PRSIQ evaluates the need for glasses, how often subjects wear glasses, how often they can function without glasses and their satisfaction with their vision without glasses. As can be seen, overall spectacle independence and satisfaction are high, with the greatest need for glasses at near. Note that even at 40 cm, 75% of subjects reported being able to function comfortably without glasses all or most of the time.
 |
Table 1 Summary Results for the PRSIQ (n = 32) |
Summary data from the IOLSAT results for this study are shown in Table 2, along with 6-month data from the Vivity Summary of Safety and Effectiveness,18 for comparative purposes. The overall percentage of subjects reporting they rarely or never needed glasses was much higher in the current study (70% vs 45.1%), driven primarily by the higher percentages at near in both bright light and dim light conditions. The percentage of subjects reporting “Good” or “Very good” vision without glasses was also higher for vision at near in the current study, though were somewhat lower for distance vision.
 |
Table 2 Summary of IOLSAT Questionnaire Results (n = 33) |
Table 3 contains summary data related to the QUVID questionnaire. Glare, halos and starbursts appeared to be the most problematic visual disturbances in terms of frequency, severity and degree of bother, though blurred vision was reported as more bothersome than glare. A two-way correlation matrix showed no significant correlations between QUVID results and the refractive status of either eye. A review of the questionnaires also pointed out several conflicting responses, where subjects recorded high levels of bother with visual disturbances in the QUVID questionnaire but reported complete satisfaction at all test distances, and overall, in the PRSIQ questionnaire.
 |
Table 3 Summary of QUVID Questionnaire Results (n = 33) |
One of the potential causes of higher levels of visual disturbance might be greater levels of anisometropia, but there was no correlation between the QUVID questionnaire results and the MRSE of the dominant eye, or the questionnaire results and either the dioptric difference between the eyes or the overall level of myopia in the non-dominant eye (p > 0.05 in all cases).
Discussion
To the best of our knowledge, this is the first study to provide clinical results for patients bilaterally implanted with this NDEV IOL with a target of −0.75 D in the non-dominant eye. The uncorrected monocular visual acuity in the emmetropic eye was similar to that reported in a previous study.19 The binocular visual acuity at distance and intermediate was somewhat lower than reported in previous studies with bilateral implantation of this IOL with a target of emmetropia in both eyes.19,22,23 With the monovision correction here, the near vision was more than a line better than was reported in these previous studies.
Gundersen and Potvin simulated monovision with this IOL using spectacle correction.20 Binocular VA at a vergence of −2.50 D (equivalent to a 40 cm viewing distance) was 1–2 lines better with 0.50 D and 1.00 D of monovision respectively than when both eyes were targeted for emmetropia. The binocular VA with 0.50 D of spectacle-induced monovision was the same as seen in the current study. They also reported the percentage of eyes with a 2.5 D range of vision at various acuities. The 76% of subjects in the current study with 0.2 logMAR or better VA at all test distances appears higher than the 60% with a 2.5 D range of vision reported in the previous study when both eyes were corrected for emmetropia, but lower than the 88% reported when one eye was corrected for 0.5 D of monovision.20 Overall binocular acuities at various distances were slightly higher in the previous study, potentially due to differences in test conditions.
Results from the PRSIQ and IOLSAT showed high levels of satisfaction, good functional vision, and indicated that a high degree of spectacle independence can be achieved with this monovision approach to using this NDEV IOL. The results here (Table 2) showed higher rates of spectacle independence at near than for a comparative IOLSAT data set from a clinical trial of the same IOL with both eyes targeted for emmetropia.19 Rates of spectacle independence and satisfaction appeared only 10–15% lower than were recently reported for a trifocal IOL using the same questionnaire.24
Results for the QUVID questionnaire in this study are difficult to interpret. The results appear higher than might be expected and appear inconsistent with the satisfaction results from the PRSIQ. This contrasts with the PRSIQ and IOLSAT data, which appear relatively consistent with each other. The reports of visual disturbances are higher than reported for the clinical trial conducted to obtain FDA approval of the lens,19 and higher than in several other recent clinical studies,22,23 though the same questionnaire was not used in all cases. It is important to note that this higher rate of reported visual disturbances did not appear to be associated with residual refractive error or the level of myopia in the non-dominant eye. One of the clinicians administering the test in the current study indicated that some patients appeared to have difficulty in understanding the questions. This points to a need to carefully review all questionnaires with patients to reduce potential confusion and inconsistent responses, while avoiding any influence in their responses. Of the 3 questionnaires administered, the QUVID results appeared to be the most problematic and seemed the least consistent with the results of the other two questionnaires.
This study has some limitations. As a single site study, the numbers were relatively low. It was also a single arm study, so no direct comparisons could be made with alternative lens designs. Comparing data across different studies can be problematic because of differences in inclusion/exclusion criteria, testing conditions and test procedures.
In conclusion, targeting 0.75 D of myopia in the non-dominant eye of patients bilaterally implanted with this NDEV IOL appeared to be a viable means of improving near vision, which is likely to increase the rate of spectacle independence in patients, with no correlated increases in visual disturbances.
Acknowledgments
Jaime Dixon, COA, study coordinator at Newsom Eye, provided administrative and data collection support for this study. Nicole Terfloth, BS, assisted with data collection for the study. This research was supported with an investigator-initiated study grant (IIT # 57706185) from Alcon. A subset of results from the study were presented at the ASCRS annual meeting in Las Vegas, USA, July 24–27, 2021.
Disclosure
Richard Potvin is a consultant to Alcon and Carl Zeiss Meditec. T Hunter Newsom has a financial interest in RxSight, Inc. The authors report no other conflicts of interest in this work.
References
1. Rodov L, Reitblat O, Levy A, Assia EI, Kleinmann G. Visual outcomes and patient satisfaction for trifocal, extended depth of focus and monofocal intraocular lenses. J Refract Surg. 2019;35(7):434–440. PMID: 31298723. doi:10.3928/1081597X-20190618-01
2. Pedrotti E, Carones F, Talli P, et al. Comparative analysis of objective and subjective outcomes of two different intraocular lenses: trifocal and extended range of vision. BMJ Open Ophthalmol. 2020;5:e000497. doi:10.1136/bmjophth-2020-000497
3. Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737–747. PMID: 28732606. doi:10.1016/j.jcrs.2017.03.037
4. Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–514. PMID: 30089179. doi:10.3928/1081597X-20180530-02
5. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. PMID: 27943250; PMCID: PMC6463930. doi:10.1002/14651858.CD003169.pub4
6. Josephson JE, Erickson P, Back A, et al. Monovision. J Am Optom Assoc. 1990;61(11):820–826. PMID: 2081823.
7. Collins MJ, Goode A. Interocular blur suppression and monovision. Acta Ophthalmol. 1994;72(3):376–380. PMID: 7976272. doi:10.1111/j.1755-3768.1994.tb02777.x
8. Johannsdottir KR, Stelmach LB. Monovision: a review of the scientific literature. Optom Vis Sci. 2001;78(9):646–651. PMID: 11587198. doi:10.1097/00006324-200109000-00009
9. Braun EH, Lee J, Steinert RF. Monovision in LASIK. Ophthalmology. 2008;115(7):1196–1202. PMID: 18061266. doi:10.1016/j.ophtha.2007.09.018
10. Reilly CD, Lee WB, Alvarenga L, Caspar J, Garcia-Ferrer F, Mannis MJ. Surgical monovision and monovision reversal in LASIK. Cornea. 2006;25(2):136–138. PMID: 16371770. doi:10.1097/01.ico.0000178722.19317.7b
11. Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. 2009;35(6):998–1002. PMID: 19465283. doi:10.1016/j.jcrs.2009.01.035
12. Barrett GD. Monovision with monofocal IOLs. In: Chang DF, editor. Mastering Refractive IOLs. New Jersey, Slack: The Art and Science; 2008:450–453.
13. Kohnen T, Suryakumar R. Extended depth-of-focus technology in intraocular lenses. J Cataract Refract Surg. 2020;46(2):298–304. PMID: 32126045. doi:10.1097/j.jcrs.0000000000000109
14. Bellucci R, Cargnoni M, Bellucci C. Clinical and aberrometric evaluation of a new extended depth-of-focus intraocular lens based on spherical aberration. J Cataract Refract Surg. 2019;45(7):919–926. PMID: 31133419. doi:10.1016/j.jcrs.2019.02.023
15. Fernández J, Rodríguez-Vallejo M, Burguera N, Rocha-de-lossada C, Piñero DP. Spherical aberration for expanding depth of focus. J Cataract Refract Surg. 2021;47(12):1587–1595. PMID: 34128496. doi:10.1097/j.jcrs.0000000000000713
16. Singh B, Sharma S, Dadia S, Bharti N, Bharti S. Comparative evaluation of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and an extended depth of focus intraocular lens. Eye Contact Lens. 2020;46(5):314–318. PMID: 31283552. doi:10.1097/ICL.0000000000000637
17. Hooshmand J, Allen P, Huynh T, et al. Small aperture IC-8 intraocular lens in cataract patients: achieving extended depth of focus through small aperture optics. Eye. 2019;33(7):1096–1103. PMID: 30792521; PMCID: PMC6707186. doi:10.1038/s41433-019-0363-9
18. Kohnen T. Nondiffractive wavefront-shaping extended range-of-vision intraocular lens. J Cataract Refract Surg. 2020;46(9):1312–1313. PMID: 32898097. doi:10.1097/j.jcrs.0000000000000247
19. US FDA. AcrySof™ IQ Vivity™ extended vision Intraocular Lens (IOL): Summary of safety and effectiveness data. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf/P930014S126B.pdf.
20. Gundersen KG, Potvin R. The effect of spectacle-induced low myopia in the non-dominant eye on the binocular defocus curve with a non-diffractive extended vision intraocular lens. Clin Ophthalmol. 2021;15:3541–3547. doi:10.2147/OPTH.S329922
21. Morlock R, Wirth RJ, Tally SR, Garufis C, Heichel CWD. Patient-Reported Spectacle Independence Questionnaire (PRSIQ): Development and validation. Am J Ophthalmol. 2017;178:101–114. doi:10.1016/j.ajo.2017.03.018
22. Bala C, Poyales F, Guarro M, et al. Multi-country clinical outcomes of a new nondiffractive presbyopia-correcting intraocular lens. J Cataract Refract Surg. 2021;Publish Ahead of Print. PMID: 34288635. doi:10.1097/j.jcrs.0000000000000712
23. Arrigo A, Gambaro G, Fasce F, Aragona E, Figini I, Bandello F. Extended depth-of-focus (EDOF) AcrySof® IQ Vivity® intraocular lens implant: a real-life experience. Graefes Arch Clin Exp Ophthalmol. 2021;259:2717–2722. PMID: 34050809. doi:10.1007/s00417-021-05245-6
24. Shatz AC, Potvin R. Spectacle independence and quality of vision after bilateral implantation of a trifocal intraocular lens. Clin Ophthalmol. 2021;15:2545–2551. PMID: 34168428; PMCID: PMC8216748. doi:10.2147/OPTH.S318203
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
