Back to Journals » Clinical Ophthalmology » Volume 16
Evaluation of Postoperative Total Ocular Aberrations After Bilateral Implantation of Monofocal IOL with Extended Depth of Focus in Phacoemulsification
Authors Abd Elghaffar Shehata M , Hosny MH , Tolba DA, Attya M
Received 8 October 2022
Accepted for publication 1 December 2022
Published 21 December 2022 Volume 2022:16 Pages 4257—4261
DOI https://doi.org/10.2147/OPTH.S391355
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohammed Abd Elghaffar Shehata, Mohamed Hassan Hosny, Doaa Ahmed Tolba, Mohamed Attya
Department of Ophthalmology, Cairo University, Cairo, Egypt
Correspondence: Mohamed Attya, Department of Ophthalmology, Cairo University, 15th Zahret Alsokar, Alsheikh Othman, Alhawamedia, Giza, Egypt, Tel +201113332892, Email [email protected]
Purpose: To evaluate postoperative visual performance and total ocular aberration in cataract patients after implantation of the TECNIS Eyhance™ intraocular lens (IOL).
Methods: Our study is a prospective interventional non-comparative study that was conducted on 34 eyes of 17 patients who underwent phacoemulsification and Eyhance IOL implantation. Postoperative corrected and uncorrected near and far visual acuity and total ocular aberration were assessed 3 months after surgery.
Results: Our study included 34 eyes of 17 patients. At the third postoperative month, the mean spherical equivalent (SE) was − 0.32 diopters (D) (SD ± 0.62), and the mean distance-corrected near visual acuity (DCNVA) was 0.33 (SD ± 0.15) and 0.42 (SD ± 0.17) decimal notation (DN) monocular and binocular, respectively. The mean near distance with maximum visual acuity was 79.47 cm (SD ± 7.70) and 74.76 cm (SD ± 7.90) monocular and binocular, respectively. The mean postoperative minimum reading addition (add) was 1.6 D (SD ± 0.47). The mean spherical aberration (SA) was 0.13 μm (SD ± 0.09). The correlation of amount of spherical aberration with power of minimum reading add at 40 cm was not statistically significant (p=0.324).
Conclusion: The TECNIS Eyhance IOL provides good intermediate visual acuity and decreases the power of the reading add needed after phacoemulsification.
Keywords: high-order aberration, presbyopia, extended depth of focus, aspheric IOLs, Eyhance
Introduction
Patient anticipation regarding refractive outcomes and spectacle independence have increased markedly in the recent past, and cataract patients have the same expectations as refractive patients. For the refractive surgeon, this means that the final goal is to achieve precise postoperative target refraction less than ±0.5 diopters (D).1
Recently, the variety of designs for intraocular lenses (IOLs) has increased, with the development of lenses that improve far and/or intermediate and/or near vision. These IOLs are branded as multifocal lenses, accommodative, trifocal, bifocal, and extended depth of focus (EDoF) IOLs.2
Nowadays, the prolonged use of computers and mobile devices has changed the preference of spectacle independence from near to intermediate distance. Concerning uncorrected intermediate visual acuity (UIVA), great variability in results has been observed with the use of different multifocal IOL models. The enhancement of intermediate vision is still required to improve patient satisfaction.3–8
A novel monofocal IOL with an altered design has become available, namely, monofocal IOL with EDoF, such as the Vivity® IOL (Alcon Inc., USA) and the Eyhance™ (model ICB00; Johnson & Johnson Vision, Santa Ana, CA, USA) IOL. This innovative feature of monofocal IOLs provides a wider range of clear vision without the need for multifocal IOLs. The new EDoF monofocal IOL (Eyhance in our study) provides an adequate depth of focus to offer patients comfortable vision without impairing far vision, as the power of the Eyhance IOL gradually increases from the periphery towards the center of the lens, and this offers superior intermediate visual acuity (VA).9 On the other hand, the newer non-diffractive type of EDoF IOL (AcrySof IQ Vivity) uses X-wave™ technology in the central 2.2 mm area to extend the depth of focus.10
Patient and Methods
Our study is a prospective interventional study that was conducted at Kasr Al-Aini Ophthalmology Hospital, Cairo, Egypt, on 34 eyes of 17 patients. They were implanted with the TECNIS Eyhance by the same surgeon during the interval between April 2021 and December 2021. The study protocol was reviewed and accepted by the Research Ethics Committee (REC) of Cairo University (MS-241-2021) and followed the principles of the Declaration of Helsinki. This study was registered with www.pactr.org (ID: PACTR202112812889125).
Participants were recruited from the cataract pre-assessment clinics. They were given a patient information sheet and signed appropriate consent before participating in the study.
Inclusion criteria: 1) patients with senile cataract scheduled for implantation with TECNIS Eyhance; 2) age of 40 years and older; 3) clear intraocular media; and 4) accessibility, willingness, and sufficient intellectual alertness to comply with the examination techniques.
Exclusion criteria: 1) visual potential of less than 0.63 in each eye due to ocular retinal or optic nerve disorders; 2) corneal astigmatism over 1D cylinder; 3) use of systemic or ocular medication that may affect vision; 4) amblyopia, strabismus, forme fruste keratoconus, or keratoconus; 5) lens zonular dehiscence that affects postoperative centration or tilt of the IOL (eg pseudoexfoliation syndrome); 6) abnormalities of the pupil (non-reactive, tonic pupils, abnormal pupil shape, or pupil diameter ≤3.5 mm under mesopic/scotopic conditions); 7) patients who had undergone refractive eye surgery (LASIK, PRK) or corneal crosslinking; and 8) intraoperative complications (eg posterior capsular tear or zonular dialysis, eccentric capsulorrhexis).
Methodology
- Preoperative assessment: All patients were subjected to slit-lamp examination of the anterior segment, intraocular pressure measurement using a Goldman applanation tonometer, measurement of best-corrected visual acuity (BCVA) using Snellen’s chart, refraction using a NIDEK AR 360-A autorefractometer (Nidek Co. Ltd, Tokyo, Japan), dilated examination of the fundus using slit-lamp biomicroscopy and +90 D lens, and biometry with an IOLMaster 500 (Carl Zeiss Meditec, Jena, Germany).
- Phacoemulsification procedure: the standard phacoemulsification was performed using the stop-and-chop technique followed by implantation of the TECNIS Eyhance (model ICB00; Johnson & Johnson Vision, Santa Ana, CA, USA) IOL in the capsular bag, and centration was ensured by excellent capsulorrhexis and uncomplicated phacoemulsification surgery.
- Postoperative care: All patients were prescribed topical antibiotics for 2 weeks and steroids for 4 weeks. Follow-up clinical examinations were performed on the first day, 1 week, 1 month, and 3 months postoperatively.
During the third month of follow-up, all patients underwent assessment of the distance-corrected near visual acuity (DCNVA) at 40 cm; the maximum near point of functional vision, measured using the Jaeger near-vision eye chart; best-corrected distant visual acuity (BCDVA), using Snellen’s chart; refraction, using the NIDEK AR-360A autorefractometer; and total wavefront analysis and corneal topography, using the SCHWIND Combi Wavefront Analyzer (CSO srl, Firenze, Italy), to calculate total ocular aberrations, total ocular high-order aberrations, corneal coma, and spherical aberration (SA).
Statistical Methods
Data were coded and entered using SPSS version 28 (IBM Corp., Armonk, NY, USA). Data were summarized using mean, standard deviation, median, minimum and maximum for quantitative data, and using frequency (count) and relative frequency (percentage) for categorical data. Correlations between quantitative variables were assessed using Spearman’s correlation coefficient.11 p-Values less than 0.05 were considered statistically significant.11
Results
This study included 34 eyes of 17 patients, with mean age 56 (±6.96) years; 64.7% of patients were male and 35.3% were female.
Preoperative Data
- The mean preoperative BCVAwas 0.26 decimal notation (DN) (SD ±0.12), range 0.05–0.5.
- The mean axial length was 22.73 mm (SD ±1.8).
- The mean preoperative K1 reading was 43.88 D (SD ±1.07).
- The mean preoperative K2 reading was 43.67 D (SD ±1.02).
- The mean IOL power was 22.35 D (SD ±1.75), range 18–25 D.
Postoperative Data
The patients’ postoperative data are summarized in Table 1.
- The mean SA was 0.21 µm (SD ±0.07) for 0.75 D minimum reading addition (add) and 00.05 (SD ±0.00) for 2.75 D minimum reading add.
- The correlation of the amount of SA with power of minimum reading add at 40 cm was not statistically significant (p=0.324), but we found that the postoperative SA ranging between 0.2 and 0.25 µm gave the minimum reading add (+0.75 D) (Figure 1).
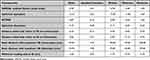 |
Table 1 Postoperative Clinical Data |
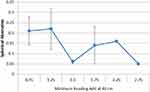 |
Figure 1 Correlation between spherical aberration and minimum reading add. |
Discussion
Despite the fact that cataract surgery with monofocal IOL implantation is an extremely successful treatment, monofocal IOLs are exclusively meant to correct distance vision.12,13
Presbyopia correction during cataract surgery is becoming more common, and patients are requesting it more often.14
Intermediate vision has become increasingly significant in the past two decades, owing to the increased usage of technologies such as computers, cellphones, and tablets. While multifocal IOLs provide good VA at all distances, the risk of dysphotopsia and the deterioration of contrast sensitivity are two disadvantages of multifocal IOLs.15
The new TECNIS Eyhance IOL represents a substantial advancement in the field of monofocal IOLs, aiming for good distance vision and intermediate vision enhancement, while avoiding photic disturbances.9
In our study, the monocular and binocular DCNVA were 0.33 and 0.42 DN, respectively. Similarly to our study, Mencucci et al and Cinar et al obtained monocular DCNVA of 0.38 DN and binocular DCNVA of 0.5 DN, and monocular DCNVA of 0.46 logarithm of the minimum angle of resolution (log MAR) (0.35 DN), respectively.14,17
Furthermore, Unsal and Sabur conducted a retrospective comparative study and found that both monocular and binocular distance-corrected and uncorrected intermediate visual acuity (DCIVA and UCIVA) were significantly higher in the TECNIS Eyhance group than the TECNIS 1-piece group after 1 month follow-up, but DCNVA was comparable between both groups.16
Moreover, we found that the minimum reading add at 40 cm equals 1.6 D, and this was in agreement with Cinar et al, who obtained a minimum reading add at 40 cm of 1.74 D.17
Postoperative SE in our study was −0.51±1.09 D. Mencucci et al also reported that the postoperative objective spherical equivalent values had a wider distribution in the TECNIS Eyhance group than the TECNIS 1-piece group, and the new design of the anterior surface with increased distribution of the power from the periphery to the center was claimed to be responsible for this.14
To our knowledge, this is the first study to measure the maximum near point of functional vision, which was found to be 79 and 75 cm monocular and binocular, respectively. This helps the patients to see clearly at intermediate distances without affecting the far distances.
Our study revealed that binocular implantation of Eyhance gives patients more comfortable intermediate and far vision than uniocular implantation. This is important when selecting patients, to give them maximum benefit from this IOL.
Our study demonstrated a statistically non-significant correlation between the amount of SA and minimum reading add, but we found that a postoperative SA ranging between 0.2 and 0.25 gives the minimum reading add (+0.75 D). De Luis Eguileor et al found a significant correlation between SA and intermediate VA; this endorses that with SA of intermediate values, the Eyhance IOL offers better intermediate VA.9
On the other hand, Nanavaty et al found a clinically non-significant difference in total and internal SA with the TECNIS Eyhance IOL, indicating that the Eyhance IOL does not induce SA.18
The Eyhance can be offered to patients undergoing routine cataract surgery. It is a great choice when premium IOLs are not desired.
Our study limitations were the small sample size and short follow-up period. To validate our findings, additional studies on Eyhance are needed with long-term results. Our focus in this study was assessment of ocular aberrations and the VA at near, intermediate, and far distances. The defocus curve and contrast sensitivity were not investigated.
In conclusion, the TECNIS Eyhance IOL provides good intermediate VA without affecting the far vision, and decreases the power of the reading add needed after phacoemulsification.
Data Sharing Statement
The authors have no problem in sharing individual deidentified participant clinical data upon reasonable request to the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Olsen T, Funding M. Ray-tracing analysis of intraocular lens power in situ. J Cataract Refract Surg. 2012;38:641–647. doi:10.1016/j.jcrs.2011.10.035
2. Pedrotti E, Carones F, Aiello F, et al. Comparative analysis of visual outcomes with 4 intraocular lenses: monofocal, multifocal, and extended range of vision. J Cataract Refract Surg. 2018;44:156–167. doi:10.1016/j.jcrs.2017.11.011
3. Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012;6:1421–1427.
4. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39:1093–1099. doi:10.1016/j.jcrs.2013.01.048
5. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014;40:60–69. doi:10.1016/j.jcrs.2013.06.025
6. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013;39:343–349. doi:10.1016/j.jcrs.2012.09.017
7. Voskresenskaya A, Pozdeyeva N, Pashtaev N, et al. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010;248:1299–1306. doi:10.1007/s00417-010-1424-8
8. Alio JL, Plaza-Puche AB, Montalban R, Javaloy J. Visual outcomes with a single-optic accommodating intraocular lens and a low-addition-power rotational asymmetric multifocal intraocular lens. J Cataract Refract Surg. 2012;38:978–985. doi:10.1016/j.jcrs.2011.12.033
9. de Luis Eguileor B, Martínez-Indart L, Martínez Alday N, Sacristán Egüén C, Cuadros Sánchez C. Differences in intermediate vision: monofocal intraocular lenses vs. monofocal extended depth of focus intraocular lenses. Arch Soc Esp Oftalmol. 2020;95(11):523–527. doi:10.1016/j.oftal.2020.06.009
10. Kohnen T, Petermann K, Böhm M, et al. Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract Refract Surg. 2022;48(2):144–150. doi:10.1097/j.jcrs.0000000000000826
11. Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614–619.
12. Fine IH, Hoffman RS. Refractive aspects of cataract surgery. Curr Opin Ophthalmol. 1996;7(1):21–25. doi:10.1097/00055735-199602000-00005
13. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;2012(9):CD003169.
14. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378–387. doi:10.1097/j.jcrs.0000000000000061
15. Lopes D, Loureiro T, Carreira R, et al. Comparative evaluation of visual outcomes after bilateral implantation of an advanced or conventional monofocal intraocular lens. Eur J Ophthalmol. 2022;32(1):229–234. doi:10.1177/1120672121995343
16. Unsal U, Sabur H. Comparison of new monofocal innovative and standard monofocal intraocular lens after phacoemulsification. Int Ophthalmol. 2021;41(1):273–282. doi:10.1007/s10792-020-01579-y
17. Cinar E, Bolu H, Erbakan G, et al. Vision outcomes with a new monofocal IOL. Int Ophthalmol. 2021;41(2):491–498. doi:10.1007/s10792-020-01599-8
18. Nanavaty MA, Ashena Z, Gallagher S, Borkum S, Frattaroli P, Barbon E. Visual acuity, wavefront aberrations, and defocus curves with an enhanced monofocal and a monofocal intraocular lens: a prospective, randomized study. J Refract Surg. 2022;38(1):10–20. doi:10.3928/1081597X-20211109-02
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
