Back to Journals » Patient Preference and Adherence » Volume 8
Evaluation and improvement of doctor–patient communication competence for emergency neurosurgeons: a standardized family model
Authors Wu X, Wang Z, Hong B, Shen S, Guo Y, Huang Q, Liu J
Received 20 March 2013
Accepted for publication 15 May 2013
Published 20 June 2014 Volume 2014:8 Pages 883—891
DOI https://doi.org/10.2147/PPA.S45488
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Xi Wu,1 Zhinong Wang,2 Bo Hong,1 Shengjuan Shen,3 Yan Guo,4 Qinghai Huang,1 Jianmin Liu1
1Department of Neurosurgery, Changhai Hospital, Shanghai, People’s Republic of China; 2Department of Surgical Education, Changhai Hospital, Changzheng Hospital, Shanghai, People’s Republic of China; 3Department of Medical Education, The Second Military Medical University, Shanghai, People’s Republic of China; 4Department of Internal Medicine, Changhai Hospital, Shanghai, People’s Republic of China
Abstract: Disease treatments have been significantly influenced by the communications between patients, their families, and doctors the lack of which may lead to malpractice allegations and complaints. In particular, inadequate communication may delay diagnosis and treatment. Therefore, for doctors communication and interpersonal skills, are as important as clinical skills and medical knowledge. In this study we intended to develop two detailed communication content checklists and a modified interpersonal skills inventory, aiming to evaluate their integrity in the midst of communication skills assessments, to provide feedback for some participants, and to observe their communication competence in both aspects
Keywords: standardized patient, communication skill, training, medical education, neurosurgeon
Introduction
Disease treatments have been significantly influenced by the communications between patients, their families, and doctors,1,2 the lack of which may lead to malpractice allegations and complaints.3,4 In particular, inadequate communication may delay diagnosis and treatment. Therefore, for doctors, communication and interpersonal skills are as important as clinical skills and medical knowledge.
In the emergency cases, an eligible neurosurgeon should handle communication more competently than in other medical encounters. Ineffective communication and consultation before life-saving operations may postpone diagnosis and treatment, thus resulting in complaints and even litigation; in contrast, good communication may retrieve more detailed patient information and proper informed consent. Regardless, many neurosurgery residents remain incapable regarding communication and interpersonal skills.
Doctor–patient communication competencies are being assessed by psychometrically sound communication assessment tools,5 mobile information and communication systems,6 database and multimedia authoring tools,7 and the Medical House Call tool.8 However, these techniques and tools can only be applied to patients capable of communicating. If the patients are not capable of communicating as they are enrolled to the emergency room, coupled with the limited time, the strategies are prone to failure. Consequently, we created and trained a standardized family to simulate the communication counterparts and to evaluate, and rate the trainers. The standardized family consisted of actors without a medical background; they simulated patients’ families, or other representatives such as a friend, teacher, roommate, and/or colleague. When directly talking to the families of patients in a critical condition, above and beyond a kind attitude, well-developed and completely detailed medical practice and procedure information are important components of communication. In this study, we tried to develop a rating instrument that focused on the detailed content and knowledge intending to inform patients’ families by referring to the Kalamazoo II Consensus Report.9
We intended to develop two detailed communication content checklists and a modified interpersonal skills inventory, aiming to evaluate their integrity in the midst of communication skills assessments, to provide feedback for some participants, and to observe their communication competence in both aspects.
Methods
Participants
Four first-year and two second-year neurosurgery residents as well as six junior attending neurosurgeons from ten neurosurgery departments in east China, all men, aged between 25 years and 30 years, were voluntarily engaged in this study.
Assessment tools
Three assessment tools were applied in this study. One was an integrity checklist of communication content with 34 items and a 3-point rating scale for subarachnoid hemorrhage (SAH) scenarios; and the second checklist, with the same scale for head trauma (HT) scenarios (Tables 1 and 2). The third assessment tool was a 13-item modified version of the 5-point Likert Interpersonal Scale based on the US National Board of Medical Examiners prototype Clinical Skills Examination (Table 3).
  | Table 1 Integrity of the communication content with SAH patients’ families |
  | Table 2 Integrity of the communication content with severe HT patients’ families |
  | Table 3 Interpersonal skills inventory |
Raters
Raters included one standardized family involved in communication; another observing communication; five professors (Jianmin Liu, Zhijian Yue, Xiaoping Zhou, Xiaowu Hu, and Yi Xu); and five associate professors (Yiqun Cao, Laixing Wang, Bo Hong, Qinghai Huang, and Wenyuan Zhao) from the Department of Neurosurgery, Changhai Hospital. They were all specially trained to identify and rate the participants’ performance by watching “full marks videos” executed by Dr Bo Hong.
Standardized family training
The standardized families, were trained to discern participants’ performance and score them accurately before the commencement of the research; they are briefly introduced below.
Case 1: SAH
The virtual patient, Changxi Wang, described as a 44-year-old male smoker, chef, with hypertension and diabetes mellitus, was admitted to the emergency room because of the sudden onset of headache and coma. Emergency computerized tomography (CT) demonstrated diffused SAH, and CT angiography disclosed an aneurysm of the right posterior communicating artery, Glasgow coma scale 10 (E2V3M5), Hunt and Hess scale grade IV, and Fisher scale grade IV. The presumed primary therapeutic strategy was: (1) take medical measures to prevent rebleeding after SAH;10 (2) immediate interventional therapy after a cerebral artery digital subtraction angiography; and (3) possible lateral cerebral ventricle drainage depending on the CT post-aneurysm embolization.
The standardized family included a simulated patient’s wife: a 42-year-old tailor, Buddhist, introverted, middle school graduate, with a 16-year-old daughter. Standardized family behavior exhibited nervousness with great grief; the wife moved back and forth with her amulet and her legs jittering. She responded to participants politely and in a friendly manner.
Case 2: HT
The virtual patient, Xiaobao Ren, a 55-year-old woman, accountant, without chronic disease, was sent to the emergency room because of HT after a traffic accident. She had a Glasgow coma scale 7 (E1V1M5), right mydriasis (diameter 4.5 mm) without direct and consensual pupillary responses to light. Emergency CT showed a right frontotemporal contusion, laceration of brain, about 40 mL of subdural hematoma, and the middle line shifted more than 1 cm leftward. The presumed primary therapeutic strategy was immediate evacuation of subdural hematomas.
The standardized family was a simulated patient’s son: a 28-year-old engineer, Catholic, extroverted and resolute, graduated from Fudan University (Shanghai, People’s Republic of China), and the only child. Standardized family behavior exhibited anxiety and impatience, clenching of fists, and asking for an emergency operation numerous times. He responded to the participants rapidly and concisely, but politely.
Experimental design
All participants were randomly paired into two groups, (Figure 1) with two first-year and one second-year resident and three junior attending neurosurgeons in each group. Two groups of participants encountered the SAH scenario as the first assessment. Then, one randomly chosen group received feedback immediately (the feedback group), whereas the other group was labeled as the no-feedback group. During the feedback, participants were allowed to read the items of the interpersonal skills checklist and the integrity checklists of communication content, and they acknowledged their scores. To exclude the impact of the first assessment, both groups were subjected to a second assessment with HT scenario 14 days later, during which no feedback was received from any groups. To evaluate any midterm impact of the feedback, both groups experienced a third assessment with SAH scenario 9 months later, during which the delivery of bad news, informed consent, and treatment prescriptions were required and included. Each group had to be finished in 20 minutes, otherwise the rating procedure was terminated. Assessment tools, raters, and standardized families in the third assessment were identical to those in the first SAH scenario.
  | Figure 1 Outline of study design. |
Data analysis
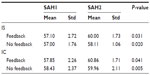
To determine the reliability level of the rating derived from the integrity checklists of communication and interpersonal skills checklists, inter-rater reliability and Cronbach’s α were calculated in the first SAH scenario. Communication scores of each scenario were processed by a two-way analysis of variance utilizing feedback (feedback, no feedback) and the education level of participants (eg, residents, junior attending doctors) as between-subjects variables (Table 4). We also launched a paired Student’s t-test on interpersonal skills and integrity of communication content in both groups between the first and second SAH scenarios (Table 5) to compare the midterm impact of feedback. SPSS 16.0 system (IBM Corporation, Armonk, NY, USA) was applied to perform statistical analyses, and P<0.05 was considered to be significant.
Results
Reliability and validity of assessment tools
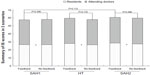
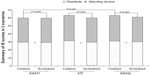
The reliability of the interpersonal skills assessment rating was acceptable (Cronbach’s α=0.752, intraclass correlation coefficient=0.987, 95% confidence interval [CI]), whereas the reliability of the integrity of communication content was good (Cronbach’s α=0.886, intraclass correlation coefficient=0.983, 95% CI). Both interpersonal skills and integrity of communication content assessment tools identified the differences between attending doctors and residents in all scenarios (Figures 2 and 3; Table 4), demonstrating the validity of those checklists by successfully distinguishing the two levels. In the first SAH scenario, the interpersonal skills checklists and the integrity checklists of communication content of the two groups did not differ significantly (P=0.929 and P=0.396, respectively), indicating a good homogeneity between groups.
Increase in communication competence by feedback
The feedback of the two groups differed significantly in the interpersonal skills in HT scenario (P<0.001), and remained thereafter until the second SAH assessment (P=0.025). In contrast, no significant differences of feedback existed in the two groups in the integrity of communication content in HT (P=0.176) and second SAH (P=0.488) scenarios.
Paired Student’s t-test revealed that both groups enjoyed boosted interpersonal skills and integrity of communication content after 9 months, which confirmed the sensitivity of both assessment tools. The increased integrity of communication content and interpersonal skills scores from the first SAH to the second SAH showed that the residents’ integrity of communication content scores rose faster (P=0.017) than those of the attending doctors, and the interpersonal skills of the feedback group was elevated more rapidly than that of the no-feedback group (P=0.028).
Discussion
Currently, doctors’ communication skills are mainly being evaluated by three methods:11 (1) checklists of observed behaviors during the interactions with real or simulated patients; (2) surveys of patients’ experience in clinical interactions; and (3) examinations using oral, essay, or multiple-choice response questions. This study selected the first protocol because: (1) it retains high fidelity to the evaluation on communication and interpersonal skills; (2) it minimizes the impact of raters;12 and (3) it allows standardized-patient exercises to be more reliable in evaluating history taking, physical examination, or communication skills than those in measuring problem-solving or clinical-reasoning skills.13,14
Although the Likert scale has been used in assessing communication skills for decades,15 it is concerned more with communication content, but it fails to cater to neurosurgeons in reality. The Likert scale was concerned more with doctors’ manners and attitudes, and patients’ sense, as well. A lot of medical disputes originate from the insufficiency of communication information as being against the rights and interests of patients and their families. Some doctors neglect patients’ families, who may not be aware of a neurosurgical emergency scenario, by just encouraging patients and their families to ask questions. Thus, patients’ families are accustomed to ascribing disease deterioration or unexpected events to a doctor’s incompetence,16 giving rise to conflicts confronting distrust and poor outcomes. To protect doctors,17 protect patients’ rights and interests, and to minimize doctor–patient conflicts, we herein developed an integrity checklist of communication content as an independent assessment tool.
In the present study, these checklists were satisfactorily reliable according to their Cronbach’s α value and intraclass correlation coefficient. The validities of the two checklists could not be calculated in the absence of available gold standards for both communication attitude and contents. However, both assessment tools managed to identify the differences between attending doctors and residents (Table 3), concomitant with desirable feedback. Additionally, they met the demands of effective communication assessment, which includes seven elements, as follows: (1) building relationships, (2) starting discussion, (3) gathering information, (4) understanding the patient’s perspective, (5) sharing information, (6) reaching agreements on problems and plans, and (7) providing closure.18 Therefore, we believe the checklists are valuable, reliable, and sensitive.
The analysis of variance results of the scenarios (first SAH, HT, and second SAH scenarios) suggest that the feedback and no-feedback groups were almost the same at the threshold of the first SAH assessment, but they began to differ significantly regarding interpersonal skills in HT and the second SAH scenarios, respectively, after 14 days and 9 months. Nevertheless, the integrity of communication content did not differ significantly between the feedback and no-feedback groups in the three scenarios.
We ascribe the feedback effect on interpersonal skills to the capabilities of the participants per se in the first place. Their communication skills stemmed from previous experiences or observations of senior physicians even without specific training.19 Some of them may not have been aware of expressing their attitudes and behaviors appropriately at first, but were corrected by referring to the feedback. The feedback boosted interpersonal skills not only in the second SAH scenario (P=0.025), but also in the HT scenario (P<0.001), indicating that communication attitudes and manners can be applied to similar situations. Contrarily, the integrity checklist of communication content was designed to assess participants’ communication skills based on their knowledge and comprehension of a certain disease, every item of which consisted of considerable detail. Thus, the feedback may not suffice to exert discernible effect on the integrity of communication content.
We assumed that utilizing “full marks video” as feedback might help participants acknowledge their errors and correct their behaviors in the future. We also believe that the feedback did not function in the HT scenario owing to the communication differences between the SAH and HT scenarios. In other words, the integrity of communication content may be scenario dependent. After 9 months of clinical practice, both groups experienced significantly raised integrity of communication content scores (Table 5), verifying the enhancement of participants’ knowledge and comprehension of diseases.
Nevertheless, this study is still not impeccable. The bias of this study essentially originated from (1) the differences between rater sources, which had been subtly decreased by pre-assessment score training, however; (2) the slightly flawed integrity checklist of communication content, which may provide more levels to distinguish examinees’ performances in the case of a 5-point scale; and (3) the lack a sufficient list of disease and operation complications in the integrity checklist of communication content, which may have befuddled the raters.
We trained standardized families and enabled doctors to communicate with the patients’ families instead of the patients themselves, which maximally simulated the critical situation in emergency rooms and expanded the conception of doctor–patient communication. As to the integrity of communication, the rating protocol we developed herein emphasized the details of content and information of which we need to inform patients’ families, which successfully bridged the gaps induced by the sole attitude- and behavior-targeting assessments. Last, those experienced doctors enjoyed remarkably enhanced interpersonal skills within a short time, benefiting from the repeated and correct feedback.
Conclusion
Traditional doctor–patient communication does not give enough credit to communication content because it is more concerned about doctors’ manners and attitudes, as well as patients’ sense. Neurosurgeons should communicate fully with patients and their families. The integrity of communication content, as equally important, can be evaluated simultaneously with interpersonal skills in communication competence assessment by these reliable, sensible, and feasible checklists. A primary feedback following evaluation may improve doctors’ interpersonal skills in different scenarios. In summary, both the integrity of communication content and interpersonal skill benefited from the method described herein in the midterm. Besides, the integrity of the communication content of residents ought to be further reinforced. Although we tried to avoid sensitivity to the Chinese culture in the design and application of the Standardized Family Model, more proof is still necessary.
Disclosure
The authors report no conflicts of interest in this work.
References
Whelan GP. Educational commission for foreign medical graduates: clinical skills assessment prototype. Med Teach. 1999;21(2):156–160. | |
[No authors listed]. Learning objectives for medical student education – guidelines for medical schools: report I of the Medical School Objectives Project. AcadMed. 1999;74(1):13–18. | |
Lefevre FV, Waters TM, Budetti PP. A survey of physician training programs in risk management and communication skills for malpractice prevention. J Law Med Ethics. 2000;28(3):258–266. | |
Shapiro RS, Simpson DE, Lawrence SL, Talsky AM, Sobocinski KA, Schiedermayer DL. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989;149(10):2190–2196. | |
Makoul G, Krupat E, Chang CH. Measuring patient views of physician communication skills: development and testing of the Communication Assessment Tool. Patient Educ Couns. 2007;67(3):333–342. | |
Ammenwerth E, Buchauer A, Bludau B, Haux R. Mobile information and communication tools in the hospital. Int J Med Inform. 2000;57(1):21–40. | |
Bental DS, Cawsey A, Jones R. Patient information systems that tailor to the individual. Patient Educ Couns. 1999;36(2):171–180. | |
Bouhaddou O, Warner H. An interactive patient information and education system (Medical HouseCall) based on a physician expert system (lliad). Medinfo. 1995;8 Pt 2:1181–1185. | |
Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med. 2004;79(6):495–507. | |
Bederson JB, Connolly ES, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009;40(3):994–1025. | |
Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med. 2004;79(6):495–507. | |
Keen AJ, Klein S, Alexander DA. Assessing the communication skills of doctors in training: reliability and sources of error. Adv Health Sci Educ Theory Pract. 2003;8(1):5–16. | |
Day SC, Grosso LJ, Norcini JJ Jr, Blank LL, Swanson DB, Horne MH. Residents’ perception of evaluation procedures used by their training program. J Gen Intern Med. 1990;5(5):421–426. | |
van der Vleuten CPM, Swanson DB. Assessment of clinical skills with standardized patients: state of the art. Teach Learn Med. 1990; 2(2):58–76. | |
Boon H, Stewart M. Patient–physician communication assessment instruments: 1986 to 1996 in review. Patient Educ Couns. 1998;35(3):161–176. | |
Chinese doctors are under threat. Lancet. 2010;376(9742):657. | |
Sun S, Wang W. Violence against Chinese health-care workers. Lancet. 2011;377(9779):1747. | |
Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med. 2001;76(4):390–393. | |
Colletti L, Gruppen L, Barclay M, Stern D. Teaching students to break bad news. Am J Surg. 2001;182(1):20–23. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.