Back to Journals » Cancer Management and Research » Volume 12
Evaluating the Performance of p16INK4a Immunocytochemistry in Cervical Cancer Screening
Authors Song F , Du H, Xiao A, Wang C, Huang X, Yan P, Liu Z, Qu X, Belinson JL, Wu R
Received 22 July 2020
Accepted for publication 1 September 2020
Published 25 September 2020 Volume 2020:12 Pages 9067—9075
DOI https://doi.org/10.2147/CMAR.S273079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Fangbin Song,1,2 Hui Du,1,2 Aimin Xiao,1,2 Chun Wang,1,2 Xia Huang,1,2 Peisha Yan,1,2 Zhihong Liu,1,2 Xinfeng Qu,3 Jerome L Belinson,4,5 Ruifang Wu1,2
1Department of Obstetrics and Gynecology, Peking University Shenzhen Hospital, Shenzhen, Guangdong, People’s Republic of China; 2Shenzhen Key Laboratory on Technology for Early Diagnosis of Major Gynecological Diseases, Shenzhen, People’s Republic of China; 3Sanming Project of Medicine in Shenzhen, Peking University Shenzhen Hospital, Shenzen, People’s Republic of China; 4Preventive Oncology International, Inc., Cleveland Heights, OH, USA; 5Gynecologic Oncology Division, Women’s Health Institute, Cleveland Clinic, Cleveland, OH,USA
Correspondence: Ruifang Wu; Hui Du
Department of Obstetrics and Gynecology, Peking University Shenzhen Hospital, No. 1120 Lianhua Road, Shenzhen, Guangdong 518036, People’s Republic of China
Email [email protected]; [email protected]
Purpose: When used for cervical cancer primary screening, liquid-based cytology (LBC) has a high specificity but a low sensitivity. For histological diagnosis of high-grade lesions, p16INK4a immunostaining has proven to be useful. Therefore, our objective was to evaluate the use of p16INK4a immuno-cytology as a primary screen and a secondary screen after primary high-risk human papillomavirus (hrHPV) screening or LBC screening.
Methods: A total of 1197 cytology slides were immuno-stained using automatic p16INK4a staining system (PathCIN®p16INK4a) in two studies from cervical screening programs. In the primary screening study, 875 slides were randomly selected and analyzed for p16INK4a. In the secondary screening study, 322 of the remaining slides were chosen by virtue of being HPV 16/18+, other hrHPV+/LBC≥ASC-US, or HPV-negative/LBC ≥LSIL. The sensitivity and specificity for detection of cervical intraepithelial neoplasia 2/3 or worse (CIN2+/CIN3+) were compared based on p16INK4a, LBC and HPV test results.
Results: In combining two studies, there were 431 cases with biopsy pathology. They included 83 cases with CIN2+ and 41 cases with CIN3+. The p16 positivity rate increased with pathologic and cytologic severity (P< 0.0001). For primary screening: p16 immuno-cytology was more specific than HPV testing and was similar in sensitivity. Also, p16 immuno-cytology compared favorably with routine LBC (≥ASC-US or ≥LSIL) in sensitivity and specificity. For secondary screening: after LBC screening, “Triaging ASC-US with p16” gave a higher specificity and a similar sensitivity as compared to the “Triaging ASC-US with hrHPV” algorithm. After HPV primary screening, p16 immuno-cytology was more specific than LBC (≥ASC-US); the calculated colposcopy referral rate was also decreased by using p16 immuno-cytology as triage. Triage of “HPV16/18 and p16” had higher specificity and similar sensitivity as compared to triage of “HPV16/18 and LBC ≥ASC-US”.
Conclusion: For primary screening, p16INK4a immuno-cytology compares favorably to routine LBC and HPV testing. p16INK4a immunostaining could be an efficient triage to reduce the colposcopy referral rate after primary hrHPV screening or LBC screening. Therefore, p16INK4a immuno-cytology may be applicable as a favorable technology for cervical cancer screening.
Keywords: cervical intraepithelial neoplasia, human papillomavirus, p16, immunochemical staining, cervical cancer screening
Introduction
Cervical cancer is a serious threat to women’s health. Fortunately, cervical cancer is highly preventable via comprehensive prevention strategies due to the well-established etiology of high-risk human papillomavirus (hrHPV) infection. In the vaccine era, organized cervical cancer screening remains one of the most effective measures to reduce cervical cancer incidence and mortality.1 Liquid-based cytology (LBC) and HPV test are the two most common cervical screening strategies. In spite of the inherent advantages of LBC in cervical screening, the low sensitivity of LBC often causes missed diagnosis.2 The effectiveness of HPV tests in cervical screening has been widely confirmed, 3–5 but the low specificity of HPV test may lead to unnecessary colposcopy referral and treatment, increases health costs and causes anxiety for women involved.6 Furthermore, with the approval and application of current vaccines, cervical screening will face challenges due to declining trends in the prevalence of HPV genotypes covered by vaccines, and a key issue will be how to adapt screening algorithms for increasingly vaccinated cohorts.7 Therefore, there is an urgent need for development of alternative biomarkers, which reflects disease progression, to improve cervical cancer screening.
p16INK4a (henceforth p16) is a cyclin-dependent kinase inhibitor that prevents phosphorylation of retinoblastoma protein (RB) and thus regulates the cell cycle. p16 Expression is negatively controlled by the RB1 gene product, and is at very low concentrations in normal cells, whereas it is strongly overexpressed in HPV-associated tumors, in which RB has been functionally inactivated by the hrHPV E7 oncoprotein.8 Therefore, p16 overexpression can be considered as a marker of HPV infection, and activated expression of viral oncogenes and virus-induced deregulation of the cell cycle.8,9 Currently, p16 immunostaining conducted in cervical biopsies or excision samples serves as an adjunctive diagnostic method to improve the accuracy of cervical intraepithelial neoplasia (CIN) diagnosis.10 This study used p16 immuno-cytology technology to detect p16 expression in cervical brushing samples, and evaluated the performance of p16 staining as an alternative marker for primary screen and secondary screen after HPV primary screening or LBC-based screening, in order to provide guidance for the prevention and control of cervical cancer.
Materials and Methods
Study Population and Design
Between May 2016 and Oct 2019, 904 women participating in primary cervical cancer screening (Primary screening population) and 359 women attending colposcopic examination (Colposcopy referral population) from cervical screening programs were recruited at Shenzhen and surrounding areas, Guangdong Province, China (Figure 1). All the nonpregnant women signed the written informed consent and met the following criteria: aged 21–69 years with a sexual history, had no history of cervical cancer or precancerous lesions, had no cervical resection or radiotherapy. Eligible participants underwent cervical cancer screening via LBC/Cobas4800 HPV cotesting. Moreover, women with complete data on LBC, HPV, p16 staining and pathologic results were analyzed. The study was conducted in accordance with the 2013 Declaration of Helsinki. The study protocol was approved by the ethics committee of Peking University Shenzhen Hospital (PUSH), Shenzhen, China (No. 2,016,001).
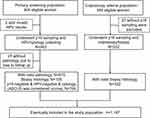 |
Figure 1 Selection of the study population. |
LBC and HPV Detection
Each participant underwent routine gynecological examination to collect cervical exfoliation cell specimens using a cervical brush, and the sample brush was placed in a SurePath vial (TriPath Imaging Inc.) for AutoCyte® thin-layer cytology test (TriPath Imaging Inc.) and Cobas®4800 HPV assay (Roches, USA). The LBC results were interpreted according to the Bethesda 2014 classification system11 and divided into the following categories: negative for intraepithelial lesions or malignancy (NILM), atypical squamous cells of undetermined significance (ASC-US), atypical squamous epithelial cells that cannot exclude high-grade lesions (ASC-H), low-grade squamous intraepithelial lesions (LSIL), and high-grade squamous intraepithelial lesion (HSIL). Cobas®4800 HPV assay provides HPV16, HPV18 and pool 12 genotypes of hrHPV (Other hrHPV, HPV31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68) results.
p16INK4a Immunocytochemical Staining
Among 904 screened women in the primary screening study, two cervical samples were collected at the initial screening. One was used for hrHPV/LBC detection we described previously, and the other was placed in the p16 cell preservation solution (Senying Biotechnology Co., Ltd., Shenzhen, China) for p16 detection. The sample for hrHPV/LBC tests and the sample for p16 detection were collected alternately to avoid the influence of sampling order on the results. For the remaining 359 women, cervical exfoliated cells were collected for p16 detection when they were called-back for colposcopy due to positive screened results (Figure 1). For immunostaining, we used a p16INK4a monoclonal antibody (clone 18A8-10) at a dilution of 1:500 via the automatic immunocytochemical staining system (PathCINp16INK4a, Senying Biotechnology Co., Ltd.) according to the manufacturer’s protocol. p16 Staining slides were reviewed by two senior cytologists from PUSH blinded to other test results. p16 Staining is localized in the nucleus or cytoplasm, a positive finding of p16 staining was defined as one or more epithelial cells stained brown or yellow regardless of the morphological appearance of the cells (Figure 2).
Colposcopy-Directed Biopsy and Pathologic Diagnoses
In the primary screening study, women positive for hrHPV, or with LBC ≥LSIL, or positive for p16 staining were referred to colposcopy. In the secondary screening study, women were offered colposcopy due to positive for HPV16/18, or other hrHPV/LBC ≥ASC-US, or LBC ≥LSIL. The Preventive Oncology International (POI) biopsy protocol of directed and random biopsies plus endocervical curettage (ECC) were performed under colposcopy.12 Pathologic diagnosis was determined by two experienced pathologists and categorized into five general groups: benign (including cervicitis, HPV infection without sign of CIN), CIN1, CIN2, CIN3, and cancers. In patients who had more than one tissue sample, the worst pathologic diagnosis was recorded. Women with a result of CIN2 or worse (CIN2+) were treated according to the clinical management of PUSH. Histology was defined as normal when women met all the following results: HPV negative, p16 negative and LBC ≤ASC-US.
Statistical Analysis
Counting data are described as rates. The chi-squared test for trend was performed to evaluate the trend of rates. Accuracy of p16 staining for primary and secondary screening was evaluated by using histology as the gold standard and CIN2+/CIN3+ as the study endpoints.13 The differences in sensitivity and specificity were compared using McNemar’s test. IBM SPSS 24.0 software (SPSS, Inc. Chicago, IL, USA) was used for statistical analysis. P <0.05 was considered statistically significant.
Results
Characteristics of Study Population
In the primary screening study, two women with invalid HPV results and 27 without histology due to loss to follow-up were excluded, leaving 875 slides randomly selected from the general population and analyzed for p16 assay; among them, 109 women underwent colposcopic biopsy because met any criteria of HPV-positive, or LBC ≥LSIL, or p16-positive (Figure 1). In the secondary screening study, 37 women without p16 sampling were excluded, leaving 322 of the remaining slides chosen by virtue of being HPV16/18 positive, or other hrHPV-positive/LBC ≥LSIL, or HPV negative/LBC ≥LSIL; among them, 222 came from the general population, and 100 from the gynecological clinic. In combining the two studies above, a total of 1197 cytology slides examined by p16INK4a immunostaining were included eventually (Figure 1), with an average age of 42.1 years (range: 22–67 years). Among them, a total of 431 cases had biopsy pathology, where 293 cases were diagnosed as normal, 55 as CIN1, 42 as CIN2, 38 as CIN3, and 3 cases as cancer. In total, 83 cases of CIN2+ and 41 cases of CIN3+ were identified.
p16 Staining, HPV Results by Different Cytologic and Pathologic Grades
The rates of p16 staining positivity, HPV positivity, and HPV16/18 positivity each showed an increasing trend with the severity of pathologic grades (Ptrend <0.0001), as well as with the severity of LBC abnormality (Ptrend <0.0001) (Table 1).
 |
Table 1 Positive Rates of P16, HPV, and Genotypes in Each Grade Lesion (N/%) |
Accuracy of p16 Staining in Primary Screening
For primary screening, p16 staining was more specific than HPV testing and was similar in sensitivity (for CIN2+, p=0.057; for CIN3+, p=1.000). p16 Staining was comparable to LBC ≥LSIL in specificity, and more favorable in sensitivity (for CIN2+, p=0.017; for CIN3+, p=0.688). Besides, p16 staining had higher specificity and similar sensitivity as compared to LBC (≥ASC-US) (Table 2).
 |
Table 2 Primary Screening Algorithms for the Detection of CIN2+/CIN3+, % (95% CI) |
p16 Staining in the Secondary Screening After Primary LBC Screening
“LBC with reflex p16 (ASC-US triage)” had a higher specificity and a similar sensitivity for detecting CIN2+/CIN3+ as compared to the “LBC with reflex hrHPV (ASC-US triage)” algorithm. However, “LBC with reflex HPV16/18 genotyping (ASC-US triage)” had a worse sensitivity (for CIN2+, p=0.002; for CIN3+, p<0.0001), and a favorable specificity as compared to the “LBC with reflex hrHPV (ASC-US triage)” algorithm (Table 3).
 |
Table 3 Secondary Screening After Primary LBC Screening, % (95% CI) |
Secondary Screening After Primary hrHPV Screening
After HPV primary screening, p16 staining was more specific than LBC (≥ASC-US) for detecting CIN2+/CIN3+, achieving a similar sensitivity and a decreased colposcopy referral rate. While p16 staining had a favorable sensitivity and a similar specificity as compared to LBC (≥LSIL). In addition, triage of “HPV16/18 and reflex p16” was comparable to triage of “HPV16/18 and reflex LBC≥LSIL” in sensitivity and specificity, while had a higher specificity and a similar sensitivity for CIN3+as compared to triage of “HPV16/18 and reflex LBC ≥ASC-US”. Moreover, the sensitivity of p16 alone was comparable to that of “HPV16/18 and p16” for the detection of CIN2+/CIN3+, while the specificity of p16 alone was significantly higher and the referral rate decreased (Table 4). Application of three triage tests as cotests (HPV 16/18 genotyping, p16 staining and LBC ≥LSIL) was comparable to LBC ≥ASC-US alone in sensitivity and specificity. While combination of three triage tests (HPV 16/18 genotyping, p16 staining and LBC ≥ASC-US) had a favorable sensitivity than LBC ≥ASC-US alone, but with a worse specificity.
 |
Table 4 Secondary Screening After Primary hrHPV Screening |
Discussion
There is no doubt about the high specificity of cytological screening, but in low-resources areas lacking infrastructure and cytologists, a high-quality cytological test is often difficult to carry out. On the other hand, LBC was not sensitive enough for the early detection of cervical lesions compared with molecular markers.14 hrHPV detection as a method of primary cervical screening has advantages over LBC, but the hrHPV test alone does not discriminate between transient infections and persistent infections, leading to its low specificity.6 Therefore, the development of alternative markers for cervical cancer screening is essential for cervical cancer prevention and control.
p16 overexpression reflects the host cell’s response to hrHPV infection and HPV pathogenic activity in cervical squamous lesions.15,16 An increasing number of studies have reported the role of p16 immunostaining in differentiating persistent infections from transient infections of hrHPV, as well as in the distinction of HSIL from LSIL.2,17 Consequently, combining cytomorphology with p16 molecular detection might have a broad application prospect in the early diagnosis of cervical cancer.2 This study found that the rate of p16 overexpression, which was detected by p16INK4a immunostaining, increased with the severity of cervical abnormality, indicating that p16 overexpression could reflect the potential of malignant transformation of cervical epithelial cells caused by hrHPV infection and may be a promising marker for screening high-grade lesions.
In this study, when used as a primary screening method, p16 staining maintains a good sensitivity and significantly improves the specificity and colposcopy referral relative to HPV test, and its specificity is comparable to LBC, which is consistent with prior studies.15,18 After LBC-based screening, for women with ASC-US, a triage is still needed to determine whether the women should be referred for colposcopy. HPV-based triage of ASC-US has proven to be accurate in identifying those who need a referral, and has been recommended in guidelines.19 However, this study confirmed that p16-based triage of ASC-US was more specific for detecting CIN2+/CIN3+ as compared to the hrHPV-based triage of ASC-US algorithm, and achieved a similar sensitivity as well as a superior colposcopy referral rate. Therefore, p16 staining is able to detect HPV-infected cells, and enhances the ability to identify the atypical hyperplasia cells and to accurately detect underlying high-grade cervical lesions.9
Currently, LBC and HPV16/18 genotypes are two most commonly used triage indicators after HPV primary screening.6 However, HPV16/18 genotypes alone show a low sensitivity for the detection of cervical cancer or precancer after HPV screening.20 In addition, the application of LBC as the triage has been limited by the complex and subjective diagnostic categories, which requires high expertise. Besides LBC and HPV16/18 genotyping, p16 staining is one of the most promising triage indicators. Interpretation of p16 staining slides is less morphology-dependent than cytological diagnosis. Since p16 staining reduces the influence of subjective factors, it is less dependent on the experience of the cytologists, and can be executed by non-pathologists after a certain amount of training. The results of the study showed that triage with p16 staining achieved a similar sensitivity and a superior specificity for the detection of CIN2+/CIN3+ as compared to LBC triage after HPV screening. Carozzi et al found that, compared with LBC as the triage, p16 triage significantly improved the sensitivity for the detection of CIN2+, but did not significantly increase the colposcopy referral rate.21 Therefore, p16 staining is expected to be an alternative to routine LBC in improving the triage management of HPV primary screening, and it may be more suitable for population-based screening.
The 2015 interim guidelines for cervical cancer screening recommend triage of hrHPV-positive women using a combination of HPV16/18 genotypes and reflex LBC for women positive for the other hrHPV genotypes.22 In comparison with the guideline algorithm, “HPV16/18 genotypes and reflex p16 staining” after HPV primary screening showed a similar sensitivity for detecting CIN3+ lesions, but with a superior specificity and a reduced colposcopy referred rate. Moreover, compared with “HPV16/18 genotypes reflex p16 staining”, p16 alone showed a similar sensitivity, while achieved a favorable specificity, and a lower colposcopy referral rate, indicating that p16 staining alone had a unique advantage in the secondary screening after HPV primary screening as well.
To the best of our knowledge, although there were several previous studies exploring the value of p16 immunocytochemical staining in the detection of cervical lesions, a large-scale study of p16 staining in cervical cancer screening is still lacking in China, and the previous studies were limited due to either that the sample size was small, or that studies evaluated the different screening tests individually, and there was little data to compare various screening strategies or triage algorithms based on combination p16 staining and HPV genotypes.2,18,21 This study, which further complements prior studies, used a newly developed commercially available p16 staining kit. In the present study, p16 immunostaining was used for detecting p16 expression in the cytology specimens. The mature technology can be performed automatically with a clean background, and the results being easy to interpret; therefore, it may be suitable for large-scale cervical cancer screening program. Moreover, p16 staining could be detected at a high-throughput with a low cost by using p16INK4a immuno-cytology assay, which can be carried out in low-resource areas and in primary hospitals.
One limitation of this study was that women with a result of HPV-negative, LBC ≤ASC-US and p16-negative did not undergo pathologic assessment. However, the expected prevalence of underlying high-grade dysplasia in this subgroup is low.18 A cohort study showed that incidence of CIN3+ in p16-positive and p16-negative women were 4.4% and 1.3%, respectively, indicating that HPV-positive, p16-positive women required an immediate colposcopy, but the HPV-positive, p16-negative women could avoid immediate colposcopy in 2–3 years.23 Another limitation was that the combined study population was not all from population-based screening programs. Consequently, the results of this study might not be extrapolated to the general population. However, all the women included in the study population came from close areas during similar periods, underwent primary screening via the same HPV/LBC cotesting, and received standardized POI schemes for colposcopy/biopsy due to abnormal screened results, which makes the evaluation of different screening strategies comparable and accurate.
Conclusions
In summary, p16 overexpression was associated with malignant transformation of cervical epithelial cells and neoplastic progression in cervical precancers. For primary screening, p16 immuno-cytology achieved a similar sensitivity to the HPV test, and a comparable specificity to routine LBC (≥LSIL). Also, it had a unique advantage in the triage of primary HPV screening or LBC-based screening. Therefore, p16INK4a immuno-cytology assay may be an optimal technology for large-sample cervical screening program due to its advantages of high accuracy for primary screening, and excellent performance for secondary screening as well as easy-to-interpret results. In the future, large-scale long-term prospective studies are still required to elucidate its role in predicting the outcome of cervical lesions.
Abbreviations
LBC, liquid-based cytology; hrHPV, high-risk human papillomavirus; CIN, cervical intraepithelial neoplasia; CI, confidence interval; CIN2+/CIN3+, cervical intraepithelial neoplasia grade 2/3 or worse; PPV, positive predictive value; NPV, negative predictive value; NILM, negative for intraepithelial lesions or malignancy; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous epithelial cells that cannot exclude high-grade lesions; LSIL, low-grade squamous intraepithelial lesions; HSIL, high-grade squamous intraepithelial lesion.
Acknowledgments
We really appreciate the technical support for p16 staining from Senying Biotechnology Co., Ltd., and all the women participated in this study. We sincerely thank Jim Byrd for his advice on revising the manuscript. Interim findings of this paper were presented in part as oral presentations at the 2019 ASCCP (Atlanta, Georgia, USA, April 2019), and the 2019 EUROGIN conference (Monaco, December 2019).
Funding
This work was supported by Shenzhen Sanming Project (No. SZSM2020); Shenzhen Key Medical Discipline Construction Fund (No. SZXK027); Shenzhen Health Family Planning Commission, Shenzhen, PR China (No. SZLY2017005). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Jansen EEL, Zielonke N, Gini A, et al. Effect of organised cervical cancer screening on cervical cancer mortality in Europe: a systematic review. Eur J Cancer. 2020:127. doi:10.1016/j.ejca.2019.12.013
2. Wu MZ, Wang S, Zheng M, et al. The diagnostic utility of p16 immunostaining in differentiating cancer and HSIL from LSIL and benign in cervical cells. Cell Transplant. 2018;28(2):1–6. doi:10.1177/0963689718817478
3. Ronco G, Dillner J, Elfstrom KM, et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383(9916):524–532. doi:10.1016/S0140-6736(13)62218-7
4. Gage JC, Schiffman M, Katki HA, et al. Reassurance against future risk of precancer and cancer conferred by a negative human papillomavirus test. J Natl Cancer Inst. 2014;106(8):dju153. doi:10.1093/jnci/dju153
5. Sroczynski G, Schnell-Inderst P, Mühlberger N, et al. Cost-effectiveness of primary HPV screening for cervical cancer in Germany–a decision analysis. Eur J Cancer. 2011;47(11):1633–1646. doi:10.1016/j.ejca.2011.03.006
6. Wentzensen N. Triage of HPV-positive women in cervical cancer screening. Lancet Oncol. 2013;14(2):107–109. doi:10.1016/s1470-2045(12)70568-5
7. Sundstrom K, Elfstrom KM. Advances in cervical cancer prevention: efficacy, effectiveness, elimination? PLoS Med. 2020;17(1):e1003035. doi:10.1371/journal.pmed.1003035
8. McLaughlin-Drubin ME, Park D, Munger K. Tumor suppressor p16INK4A is necessary for survival of cervical carcinoma cell lines. Proc Natl Acad Sci USA. 2013;110(40):16175–16180. doi:10.1073/pnas.1310432110
9. Sano T, Oyama T, Kashiwabara K, Fukuda T, Nakajima T. Expression status of p16 protein is associated with human papillomavirus oncogenic potential in cervical and genital lesions. Am J Pathol. 1998;153(6):1741–1748. doi:10.1016/S0002-9440(10)65689-1
10. Goyal A, Ellenson LH, Pirog EC. p16 positive histologically bland squamous metaplasia of the cervix: what does it signify? Am J Surg Pathol. 2019. doi:10.1097/PAS.0000000000001364
11. Nayar R, Wilbur DC, The Pap Test and Bethesda 2014. “The reports of my demise have been greatly exaggerated.” (after a quotation from Mark Twain). Acta Cytol. 2015;59(2):121–132. doi:10.1159/000381842
12. Belinson JL, Pretorius RG, Standard A. Protocol for the colposcopy exam. J Low Genit Tract Dis. 2016;20(4):e61–e62. doi:10.1097/LGT.0000000000000239
13. Luttmer R, Dijkstra MG, Snijders PJ, et al. p16/Ki-67 dual-stained cytology for detecting cervical (pre)cancer in a HPV-positive gynecologic outpatient population. Mod Pathol. 2016;29(8):870–878. doi:10.1038/modpathol.2016.80
14. Adcock R, Cuzick J, Hunt WC, McDonald RM, Wheeler CM. Role of HPV genotype, multiple infections and viral load on the risk of high-grade cervical neoplasia. Cancer Epidemiol Biomarkers Prev. 2019;28(11):1816–1824. doi:10.1158/1055-9965.EPI-19-0239
15. Bergeron C, Ronco G, Reuschenbach M, et al. The clinical impact of using p16(INK4a) immunochemistry in cervical histopathology and cytology: an update of recent developments. Int J Cancer. 2015;136(12):2741–2751. doi:10.1002/ijc.28900
16. Ishikawa M, Fujii T, Saito M, et al. Overexpression of p16 INK4a as an indicator for human papillomavirus oncogenic activity in cervical squamous neoplasia. Int J Gynecol Cancer. 2006;16:1. doi:10.1111/j.1525-1438.2006.00355.x
17. Miralpeix E, Genovés J, Maria Solé-Sedeño J, et al. Usefulness of p16INK4a staining for managing histological high-grade squamous intraepithelial cervical lesions. Mod Pathol. 2016;30(2):304–310. doi:10.1038/modpathol.2016.168
18. Samarawardana P, Dehn DL, Singh M, et al. p16(INK4a) is superior to high-risk human papillomavirus testing in cervical cytology for the prediction of underlying high-grade dysplasia. Cancer Cytopathol. 2010;118(3):146–156. doi:10.1002/cncy.20078
19. Arbyn M, Anttila A, Jordan J, et al. European guidelines for quality assurance in cervical cancer screening. Second edition–summary document. Ann Oncol. 2010;21(3):448–458. doi:10.1093/annonc/mdp471
20. Cox J, Castle PE, Behrens CMSA, Wright TC, Cuzick J, Athena HPV Study Group. Comparison of cervical cancer screening strategies incorporating different combinations of cytology, HPV testing, and genotyping for HPV 16/18: results from the ATHENA HPV study. Am J Obstet Gynecol. 2013;208(3):
21. Carozzi F, Confortini M, Palma PD, et al. Use of p16-INK4A overexpression to increase the specificity of human papillomavirus testing: a nested substudy of the NTCC randomised controlled trial. Lancet Oncol. 2008;9(10):937–945. doi:10.1016/s1470-2045(08)70208-0
22. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Gynecol Oncol. 2015;136(2):178–182. doi:10.1016/j.ygyno.2014.12.022
23. Carozzi F, Gillio-Tos A, Confortini M, et al. Risk of high-grade cervical intraepithelial neoplasia during follow-up in HPV-positive women according to baseline p16-INK4A results: a prospective analysis of a nested substudy of the NTCC randomised controlled trial. Lancet Oncol. 2013;14(2):168–176. doi:10.1016/s1470-2045(12)70529-6
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

