Back to Journals » Risk Management and Healthcare Policy » Volume 17
Evaluating the Impact of Interventions and Improvements in Outpatient Intravenous Infusion Therapy at a Hospital in China: A Comprehensive Analysis of Prescription Patterns and Safety Measures
Authors Sang R, Jiang M, Zhao Q, Kong L
Received 23 November 2023
Accepted for publication 22 February 2024
Published 8 March 2024 Volume 2024:17 Pages 525—533
DOI https://doi.org/10.2147/RMHP.S451516
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Ran Sang,1,2 Manxue Jiang,1,2 Qiuju Zhao,2 Lingti Kong1,2
1Department of Pharmacy, The First Affiliated Hospital of Bengbu Medical University, Bengbu, 233004, People’s Republic of China; 2School of Pharmacy, Bengbu Medical University, Bengbu, 233030, People’s Republic of China
Correspondence: Lingti Kong, Department of Pharmacy, The First Affiliated Hospital of Bengbu Medical University, 287 Changhuai Road, Longzihu District, Bengbu, Anhui, 233004, People’s Republic of China, Tel +865523086297, Email [email protected]
Background: The excessive use of intravenous infusion in China was once a serious problem, but in recent years, attention has been paid to the phenomenon, and the government has implemented several policies to solve the problem, which has been gradually improved.
Aim: This study focuses on evaluating the impact of ongoing interventions and improvements in outpatient intravenous infusion therapy.
Methods: From January 2016 to December 2022, we conducted a study to gather annual data on intravenous infusion prescriptions. A data questionnaire, encompassing information on departments, clinical diagnosis, and infusion drugs, was developed for this purpose. We analyzed the changing trends of Top 10 clinical departments with higher intravenous infusion usage rates and Top 10 drugs used. We also evaluated the compliance of intravenous infusion prescriptions with management regulations and drug instructions, for further intervention in the future.
Results: The analysis of intravenous infusion prescription rates revealed a gradual decrease from 10.89% to 5.63%. This reduction was statistically significant (P < 0.05). High levels of intravenous infusion use were consistently observed in emergency surgery and emergency medicine. Commonly administered drugs via infusion included antibacterial drugs, tumor medications, proton pump inhibitors, and injections of traditional Chinese medicine. Inappropriate prescriptions are often characterized by issues related to drug dosage, usage, indication, and selection. Trend analysis of unreasonable types revealed significant improvements in “Diagnosis incomplete/unwritten”, “Solvent selection”, “Dosing frequency”, and “Treatment without indication” (P < 0.05).
Conclusion: The findings of this study indicate a gradual improvement in the situation regarding intravenous infusion. However, there are still prevalent instances of unreasonable practices that need to be addressed.
Keywords: cross-sectional study, evaluation, analysis, intravenous infusion prescriptions, outpatient
Introduction
In hospitals throughout China, intravenous infusion is widely utilized as a significant method of clinical treatment.1–4 Reports indicate that in 2019, China consumed a staggering 10.5 billion medical infusion bags, equivalent to 7.5 bottles per person per year, significantly exceeding the international average. The 2020 National Adverse Drug Reaction Monitoring Annual Report reveals that injection administration accounts for 56.7% of all reported adverse drug reactions, with intravenous administration alone contributing to 91.1% of these reactions.5 Moreover, injections represent 57.0% of the total dosage form, with severe adverse reactions reported in 73.0% of injection cases.5 Evidently, intravenous administration poses significant risks and potential safety hazards, leading to a higher incidence of adverse reactions during clinical use.6–9
Furthermore, studies have highlighted the excessive and irrational use of intravenous infusion in China involving antibiotics, traditional Chinese medicine, adjuvant drugs, and parenteral nutrition.1,4 In a tertiary children’s hospital, approximately 30.5–50.1% of intravenous antibiotic prescriptions were inappropriately used for pneumonia, acute bronchitis, fever, and acute upper respiratory infection.3
In recent years, substantial efforts have been made to enhance medical safety in China. The National Health Commission and various provinces and cities have issued numerous notices aimed at promoting the rational use of medication.10 The goal is to standardize hospital practices and address the excessive and unjustified use of intravenous infusion to reduce medical risks and alleviate patients’ healthcare costs.
In 2014, the Anhui Health Commission issued a notice to strengthen supervision of intravenous infusion practices in medical facilities. This notification included a list of 53 prevalent ailments commonly encountered in outpatient and emergency departments that do not require treatment via intravenous infusion.11 The objective is to mandate healthcare facilities at all levels to establish uniform protocols for managing intravenous infusion procedures, enhance oversight of medical safety measures, and reduce unnecessary infusion practices.
Recently, the National Health Commission released a “Notice on Issuing the National Medical Quality and Safety Improvement Goals for 2021”, which includes reducing the usage of intravenous infusion in hospitalized patients as one of the top ten goals for enhancing national medical quality and safety improvement goals.12 This marks the first time such a goal has been established on this list.
Within our hospital setting, the Pharmacy Department, Medical Management Department, and Quality Management Department are actively engaged in ongoing interventions concerning intravenous infusion prescriptions. This study aims to analyze outpatient intravenous infusion prescriptions and evaluate the impact of our continuous intervention efforts.
Materials and Methods
Study Design
Between January 2016 to December 2022, a retrospective descriptive study was conducted. Intravenous infusion prescriptions for outpatients were collected, to analyse trends in prescription use in recent years.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the First Affiliated Hospital of the Bengbu Medical College. As this study was a retrospective analysis and patient information was anonymized, this study ensured that no harm was done to the authors and that the information was kept strictly confidential. The Ethics Committee waived the patient’s informed consent.
Data Collection
All information was obtained from the Hospital Information System (HIS) system. To gather pertinent information on intravenous infusion prescriptions, we developed annual data questionnaires, including the patient’s medical department, drug variety, quantity, dosage, indications, etc.
We randomly selected the number 15, during this survey, we collected all intravenous infusion prescriptions in outpatient patients on the 15th day of each month (or the first working day after weekends and holidays) as research data. We then analyzed the trends and rationality of intravenous infusion prescription usage over times.
Interventions
To enhance the rational utilization of medications, the hospital’s Pharmacy, Medical Management, and Quality Management departments have implemented a range of measures, including:
Pharmacy Department: Providing training for doctors, promoting rational drug use among medical staff and patients, conducting prescription audits, and performing prescription evaluations.
Medical Management Department: Organizing training sessions, developing management protocols, issuing notifications, and implementing penalties for inappropriate prescriptions.
Quality Management Department: Coordinating prescription evaluations and enforcing penalties for unjustified prescriptions.
These interventions have been ongoing from August 2015 to the present.
Statistical Analysis
Based on questionnaires, we analyzed the changing trends of the top 10 clinical departments with higher intravenous infusion usage rates and the top 10 drugs used. We also evaluated the compliance of intravenous infusion prescriptions with the management regulations and drug instructions. To ensure the accuracy of the results, a pharmacist conducted a preliminary analysis of the rationality of the prescription, which was then revalidated by another pharmacist. SPSS analysis was conducted a statistical analysis, and the counting data were presented in the form of ratios or percentages. After frequency weighting, we performed a chi-square trend test on the proportion of unreasonable prescription types in different years.
Results
Changes in the Prescription Rate of Intravenous Infusion
The analysis included 14,081 prescriptions. Figure 1 displays the changes in intravenous infusion prescription rates for outpatients between 2016 and 2022. The data indicates that there was a gradual decline in intravenous infusion rates from 10.89% to 5.63%.
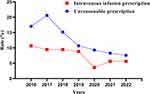 |
Figure 1 Annual change trend of intravenous infusion prescription rate and unreasonable prescription rate in 2016–2022. |
Top 10 Clinical Departments with Intravenous Infusion Prescriptions
Table 1 displays the top 10 clinical departments that prescribed intravenous infusions, revealing that emergency surgery and emergency medicine had consistently high proportions of intravenous infusion prescriptions. Specifically, the intravenous infusion rate in emergency medicine ranged from 13.36% to 31.94%, with the median of 25.09%; while the intravenous infusion rate in emergency surgery from 2016–2022 was 9.09% to 25.62%, with a median of 13.93%. Conversely, the proportion of intravenous infusion prescriptions in pediatrics, and neurology departments decreased significantly. However, the proportion of intravenous infusion prescriptions in oncology department is gradually increasing.
 |
Table 1 The Top 10 Clinical Departments with Intravenous Infusion Prescriptions from 2016 to 2022 |
Top 10 Drugs Used in Intravenous Infusion Prescriptions
Table 2 reveals that the primary medications administered through intravenous infusion in our hospital comprise antibacterial drugs, tumor medications, proton pump inhibitors, and traditional Chinese medicine injections.
 |
Table 2 The Top 10 Intravenous Medications Used from 2016 to 2022 |
Evaluation results of Intravenous Infusion Prescriptions
As shown in Table 3, the assessment of intravenous infusion prescriptions indicates a noteworthy improvement in the unreasonable prescription of intravenous infusions. The overall rate decreased from 19.65% (469/2387) in 2016, to 7.59% (154/2029) in 2022. Specifically, the rate of irregular prescriptions decreased from 4.02% (96/2387) to 0.2% (4/2029), while the rate of unsuitable and excessive prescriptions decreased from 15.63% (373/2387) to 7.39% (150/2029). Trend analysis of unreasonable types revealed significant improvements in “Diagnosis incomplete/unwritten”, “Solvent selection”, “Dosing frequency”, and “Treatment without indication” (P < 0.05).
 |
Table 3 The Unreasonable Type from 2016 to 2022 |
Discussion
Based on the statistical data of outpatient and emergency intravenous infusion between 2016 and 2022 in our hospital (Figure 1), a significant decline in the rate of intravenous infusions is evident, indicating effective control over excessive usage. In 2019, the rate of intravenous infusion decreased to 8.93%. Moreover, there was a remarkable reduction in the rate of intravenous infusion in 2020 (3.62%), which can be attributed to the impact of the COVID-19 pandemic.13–18 Restriction measures imposed by hospitals and patient concerns about contracting COVID-19 resulted in decreased hospital visits.15–18 However, the rate of intravenous infusion has since rebounded.
As shown in Table 1, departments such as emergency, pediatrics, oncology, and neurology demonstrate higher rates of intravenous infusion. The emergency department presents the highest percentage since critically ill patients require rapid-acting medication that achieves therapeutic concentration more effectively through intravenous infusion—a primary treatment method. In pediatrics, where fever predominates among patients, factors such as drug formulation, taste, and duration of action impact treatment outcomes for children. Intravenous infusion is often chosen due to eagerness and incomplete understanding by patients or their family members.19,20 The oncology department is responsible for diagnosing and treating tumor patients. Intravenous infusion is commonly used for chemotherapy administration when formulating treatment plans. Furthermore, our hospital schedules daytime chemotherapy sessions for tumor patients at the outpatient department to optimize ward utilization—another contributing factor to high intravenous infusion rates. In the neurology department, frequent utilization of intravenous infusion can be attributed to the patient demographic consisting mainly of middle-aged and elderly individuals with complex conditions, for whom intravenous infusion is often favored to expedite recovery.
Based on the observed changes in the proportion of intravenous infusion prescriptions, there has been a noticeable decrease in the utilization of intravenous infusion in pediatrics, oncology, and neurology departments. However, in the emergency department, the rate of intravenous infusion has either remained high or even increased. Therefore, the findings suggest that intervention efforts should focus on addressing intravenous infusion practices specifically in the emergency department. Table 2 illustrates alterations in intravenous infusion medications. Notably, there has been a steady decrease in the proportion of antibacterial drugs used in intravenous infusions, indicating progress in reducing their overuse. However, there are still concerns regarding inappropriate selection of antibacterial drugs. For instance, conditions like acute viral tonsillitis and acute bronchitis typically do not require antibiotics. Clinicians should exercise greater caution when selecting appropriate antibacterial drugs to minimize or delay bacterial resistance.21,22 Additionally, there is a lack of standardization in dosage and frequency for antibacterial drugs. Many prescriptions call for once-A-day administration instead of the recommended three to four times daily for optimal therapeutic effect. This discrepancy can negatively impact treatment outcomes. These findings highlight the need for further attention towards standardized use of antibacterial drugs.
Based on the assessment outcomes of intravenous infusion prescriptions (as presented in Table 3), it is evident that inappropriate prescription practices have significantly improved, but still persist to some extent. For example, improper dosing frequency occurs most frequently with antibiotics, where once-A-day dosing is prevalent instead of the recommended 2–3 times daily.21 Trend analysis of unreasonable types in recent years revealed significant improvements in “Diagnosis incomplete/unwritten”, “Solvent selection”, “Dosing frequency”, and “Treatment without indication” (P < 0.05). However, further control is needed for “Date exceeded”, “Medication indications”, “Selection of drugs”, “Dosage”, and “Dose course”.
Intravenous infusion, as a treatment method, can be considered a “double-edged sword.” While it can effectively cure diseases, it also poses various risks and potential adverse events that can harm patients. In recent years, hospitals have introduced management processes and implemented their own methods to control outpatient infusion, with some hospitals even discontinuing the practice altogether. However, simply reducing the usage rate of intravenous infusion is an insufficient measure for assessing its rational use. We emphasize the importance of hospitals strengthening supervision and guidance, fully utilizing the expertise of hospital pharmacists, and intensifying the prescription review process to ensure appropriate indications, usage, and dosage of intravenous infusion.
Conclusions
In conclusion, the outpatient department of our hospital has shown a gradual improvement in the status of intravenous infusion. However, there are still instances of unreasonable infusion practices that need to be addressed. To mitigate these issues, it is crucial for the hospital to enforce prescription guidelines for healthcare providers and involve pharmacists in reviewing and verifying prescriptions. This collaboration will help minimize incidents of inappropriate intravenous infusion and ensure the provision of safe and effective treatment.
Funding
The talent training plan of Bengbu Medical College (No. by51201316); The Anhui Province key clinical specialty construction project. (unnumbered) New era education quality project-post graduate education of Anhui Province (No.2022zyxwjxalk148).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yuan S. China should reduce the overuse of intravenous infusion. BMJ. 2014;348:g1262. PMID: 24495923. doi:10.1136/bmj.g1262
2. Zhang Z, Hu Y, Zou G, et al. Antibiotic prescribing for upper respiratory infections among children in rural China: a cross-sectional study of outpatient prescriptions. Glob Health Action. 2017;10(1):1287334. PMID: 28462635. doi:10.1080/16549716.2017.1287334
3. Lan MJ, Yao DF, Zhu LL, et al. The rate of infusion represents an important aspect of administering anticancer agents. Risk Manag Healthc Policy. 2023;16:2531–2541. PMID: 38024501. doi:10.2147/RMHP.S442692
4. Zeng S, Wang D, Liu W, et al. Overuse of intravenous infusions in China: focusing on management platform and cultural problems. Int J Clin Pharm. 2019;41(5):1133–1137. PMID: 31468253. doi:10.1007/s11096-019-00898-0
5. National adverse drug reaction monitoring annual report; 2020. Available from: https://www.nmpa.gov.cn/directory/web/nmpa/xxgk/fgwj/gzwj/gzwjyp/20210325170127199.html?ivk_sa=1024320u.
6. Yao JJ, Jurgensmeier K, Woodhead BM, et al. The use and adverse effects of oral and intravenous antibiotic administration for suspected infection after revision shoulder arthroplasty. J Bone Joint Surg Am. 2020;102(11):961–970. PMID: 32079886. doi:10.2106/JBJS.19.00846
7. Ternullo S. Acetadote (intravenous acetylcysteine): adverse effects more significant than with oral acetylcysteine. J Emerg Nurs. 2006;32(1):98–100. PMID: 16439302. doi:10.1016/j.jen.2005.09.015
8. Sasijareonrat N, Jahn N, Ungprasert P, et al. Efficacy and the adverse effects of oral versus intravenous arsenic for acute promyelocytic leukemia: a meta-analysis of randomized-controlled studies. Technol Cancer Res Treat. 2020;19:1533033820937008. PMID: 32583728. doi:10.1177/1533033820937008
9. Zeng S, Wang D, Yan Y, et al. Single-center analysis of the potential inappropriate use of intravenous medications in hospitalized patients in China. Clin Ther. 2019;41(8):1631–1637.e4. PMID: 31174860. doi:10.1016/j.clinthera.2019.05.009
10. Wang X, Wu D, Xuan Z, et al. The influence of a ban on outpatient intravenous antibiotic therapy among the secondary and tertiary hospitals in China. BMC Public Health. 2020;20(1):1794. PMID: 33239002. doi:10.1186/s12889-020-09948-z
11. The notice on strengthening the management of intravenous infusion in medical institutions. Available from: http://www.yingquan.gov.cn/xxgk/detail/content/549254837f8b9a9a2e349d5f.html.
12. Notice on issuing the national medical quality and safety improvement goals for 2021. Available from: http://www.nhc.gov.cn/yzygj/s7657/202102/8c53313663284a7ba146648509538ee2.shtml.
13. Sakamoto D, Hamaguchi T, Nakayama Y, et al. Changes in motor paralysis involving upper extremities of outpatient chronic stroke patients from temporary rehabilitation interruption due to spread of COVID-19 infection: an observational study on pre- and post-survey data without a control group. PLoS One. 2021;16(12):e0260743. PMID: 34882736. doi:10.1371/journal.pone.0260743
14. Cho SK, Mattke S, Sheridan M, et al. Outpatient wound clinics during COVID-19 maintained quality but served fewer patients. J Am Med Dir Assoc. 2022;23(4):660–665.e5. PMID: 34861225. doi:10.1016/j.jamda.2021.11.001
15. Machado KLC, Rosa STD, Dobner S, et al. Warfarin anticoagulation in the Covid-19 pandemic: telephone-based management at a regional hematology outpatient center in Joinville, Brazil. Thromb Res. 2021;205:81–83. PMID: 34265606. doi:10.1016/j.thromres.2021.07.006
16. Knörr V, Dini L, Gunkel S, et al. Use of telemedicine in the outpatient sector during the COVID-19 pandemic: a cross-sectional survey of German physicians. BMC Prim Care. 2022;23(1):92. PMID: 35461212. doi:10.1186/s12875-022-01699-7
17. Belleudi V, Finocchietti M, Fortinguerra F, et al. Drug prescriptions in the outpatient management of COVID-19: evidence-based recommendations versus real practice. Front Pharmacol. 2022;13:825479. PMID: 35401220. doi:10.3389/fphar.2022.825479
18. Winglee K, Hill AN, Langer AJ, et al. Decrease in tuberculosis cases during COVID-19 pandemic as reflected by outpatient pharmacy data, United States, 2020. Emerg Infect Dis. 2022;28(4):820–827. PMID: 35318920. doi:10.3201/eid2804.212014
19. Pate J, Mooney J, Katz E, et al. Efficacy of outpatient infusion therapy in pediatric patients with postconcussive headaches. Childs Nerv Syst. 2022;38(1):103–108. PMID: 34671849. doi:10.1007/s00381-021-05383-6
20. Park J, You SB, Kim H, et al. Experience of nurses with intravenous fluid monitoring for patient safety: a qualitative descriptive study. Risk Manag Healthc Policy. 2022;15:1783–1793. PMID: 36171867. doi:10.2147/RMHP.S374563
21. Adegbite BR, Edoa JR, Schaumburg F, et al. Knowledge and perception on antimicrobial resistance and antibiotics prescribing attitude among physicians and nurses in Lambaréné region, Gabon: a call for setting-up an antimicrobial stewardship program. Antimicrob Resist Infect Control. 2022;11(1):44. PMID: 35241171. doi:10.1186/s13756-022-01079-x
22. Sannathimmappa MB, Nambiar V, Aravindakshan R. Antibiotics at the crossroads - Do we have any therapeutic alternatives to control the emergence and spread of antimicrobial resistance? J Educ Health Promot. 2021;10:438. PMID: 35071644. doi:10.4103/jehp.jehp_557_21
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
