Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Evaluating the Effectiveness of a Clinical Practice Intervention in Increasing Obesity Data Recording at a Western Australian Country Health Service Hospital: A Quasi-Experimental Controlled Trial
Authors McClean K , Cross M , Reed S
Received 24 June 2021
Accepted for publication 19 August 2021
Published 11 September 2021 Volume 2021:14 Pages 2501—2512
DOI https://doi.org/10.2147/JMDH.S325903
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Kim McClean, Martyn Cross, Sue Reed
Occupational Safety and Health Department, Edith Cowan University, Joondalup, Western Australia, Australia
Correspondence: Kim McClean Email [email protected]
Purpose: Identification and mitigation of obesity-related risks to staff and healthcare organisations can occur using patient obesity data; however, a 2017/18 audit of obesity data accuracy was assessed to be poor. This study investigates the results of an intervention to improve obesity data recording and coding accuracy at an Australian hospital.
Background: Increasing population obesity rates result in increased organisational and financial risks to hospitals. Australian obesity prevalence has steadily increased since 1995, and 42% of the Australian population is predicted to be obese in 2035. To reduce risks to healthcare staff who care for obese patients, complete and accurate obesity recording is required.
Methods: Following a previous audit of obesity recording and coding accuracy of patients admitted to hospital with Type II diabetes, a 12-month intervention was undertaken, comprising staff education, introduction of tape measures and obesity decision-making tools, recording of patient volunteered height, regular reinforcement of obesity recording requirements and enhanced clinical coding of obesity. A re-audit was subsequently conducted to determine if the intervention impacted obesity recording and coding at the previously audited site.
Results: Improved recording of obesity-related measures and obesity data accuracy were observed, including increased patient BMI, impacted by increased patient height measurements and increased patient weight measurements. Obesity recording accuracy increased due to the intervention, including increased sensitivity, increased negative predictive values and reduced false negatives.
Conclusion: The obesity recording intervention was successful; however, as hospitals increasingly use electronic health records, improvement opportunities should be considered such as compulsory recording of patient weight and height, embedded BMI calculators and “check boxes” for recording impacts of obesity conditions on treatment. Immediate improvement of obesity recording in manual patient files can be achieved in the meantime by implementing targets of 100% weight, height and BMI recording, introducing education programs and auditing compliance.
Keywords: obesity, obese, patient handling, coding, administrative data, intervention, training
Introduction
Pressure on Australia’s healthcare system is increasing annually partially due to the ageing population of Baby Boomers and increases in chronic conditions such as obesity. Obese patients are demonstrated to have a higher likelihood of requiring clinical care than patients who are within healthy weight ranges.1,2 Obesity also contributes to the increased risk of developing other chronic health conditions such as heart disease, diabetes, stroke, kidney disease, cancers and mental health conditions, all of which may also require hospital admission.3 Managing obese patients results in increased risk of injuries to healthcare staff and organisations4 and, although “no lift” approaches have been implemented in some Australian hospitals, musculoskeletal injuries continue to occur due to care requirements to move obese (bariatric) patients, particularly to nurses and other staff providing care to obese patients.
A high prevalence of obesity within the Australian population is well documented, with the Australian Bureau of Statistics’ (ABS) National Health Survey 2017–185 revealing that 31.3% of Australians aged 18 years and over were obese. Australian obesity rates have consistently increased, from 18.7% in 1995, to 24.4% in 2007–08 and 31.3% in 2017–18.5–7 Concerningly, 42% of the Australian population is predicted to be obese in 2035.8 Correlations between population obesity rates and hospital admissions of obese patients have been demonstrated, which presents ongoing risks for healthcare workers and requirements for obesity risk reduction initiatives by healthcare organisations.1,9–11
While recording and measuring obese patient healthcare requirements is important from a staff safety perspective, it is also important for public health information which may inform obesity-related education and targeted treatment campaigns. The obesity condition cost the Australian economy $8.6 billion in 2011/12 in direct and indirect costs and is anticipated to rise by $87.7 billion between 2015 to 2025 if no public health action is taken to curb obesity.11 Increased recording of obese patients admitted in hospitals will increase focussed obesity-related treatment such as engagement of dieticians, social workers and other allied health workers. Conversely, increased weight, height and BMI recording will also identify patient malnutrition and inform engagement of similar hospital services.
McClean, Cross and Reed’s 2020 literature review4 identified risks to healthcare staff and organisations who manage obese patients including increased back, wrist, knee and shoulder injuries to nurses. Caring for obese patients requires more time, is more labour intensive and requires more staff and increased patient handling skills and solutions than managing normal-weight patients, all of which can be problematic in time- and resource-poor hospitals. Additionally, hospitals that treat obese patients were found to experience high liability and financial risks as a result of increased workers’ compensation and common law claims by injured staff and potential medical negligence claims by patients with obesity.4
Work, health and safety obligations require healthcare organisations to manage risks to their staff as far as practicable. In order to adopt sound risk management practices to protect staff managing obese patients, accurate obesity data is required. Inaccurate or unavailable patient obesity data may make it difficult for healthcare organisations to design and implement evidence-based proactive risk management approaches. Additionally, incompleteness of obesity data may result in either organisational ignorance of obesity risks or organisational reliance on anecdotal awareness of obese patient risks. Use of data to reduce organisational risks is promoted by Stanfill et al,12 who recognise significant advancements in healthcare data requirements and data analysis, including accurate coding and reporting of health diagnosis and conditions.
Increased admission of obese patients will occur in country hospitals due to obesity rates being generally higher in country locations than metropolitan locations.13 This will also result in higher injury risks to healthcare workers in country hospitals. In order to identify and reduce obesity-related risks to staff in country hospitals, assurance of accurate obesity data is required. The Western Australian Country Health Service (WACHS) was selected for this study as it is the largest country (rural) health system in Australia, which provides an extensive range of health services across an area of 2.53 million square kilometres for an estimated population of 531,000 people.14
Several international studies have examined the accuracy of obesity data and coding;for example, Martin et al15 and Quan et al16 both assessed variability between obesity coding and patient charts and found large inconsistencies. McClean, Cross and Reed’s 2019 retrospective audit17 examined accuracy of admission records of obese patients in four WACHS hospitals, which revealed poor recording of weight (67%), height (24%) and body mass index (BMI) when weight and height measurements were recorded (38%). Poor obesity data accuracy was also determined by low sensitivity results (40%) and high false negative results (60%). This analysis of obesity recording and accuracy revealed that improvement is required to accurately reflect the frequency of obese patients treated in WACHS hospitals and inform risk management strategies to protect staff from patient handling injuries when managing obese patients. Therefore a broad intervention was undertaken to raise awareness of the requirement to record obesity and enhance methods to record obesity at one WACHS hospital. To assess whether this strategy had made any impact on obesity recording or data accuracy, a repeat audit of obese patients' records was conducted and compared to the original audit. Here, we report on the results of the second audit.
Methods
Intervention Design
The hospital-wide intervention at site A to address improved obesity recording and coding was conducted over 12 months. Site A had previously participated in the preceding retrospective audit17 which provided a baseline for this intervention. The intervention included several approaches aimed to improve obesity data recording and coding:
- education sessions for medical, nursing staff and clinical coding staff to emphasise the importance of accurate obesity data recording for both clinical and safety decision making, recording locations within medical charts for height, weight and BMI measurements and evidence-based methods to measure height of patients who are bed-ridden or unable to stand due to their health conditions;
- introduction of tape measures to nursing staff to undertake height measurements of bed-ridden patients;
- introduction of obesity decision-making tools such as BMI charts and measurement tools in emergency departments, wards and clinical coding offices to allow easy identification of obesity;
- recording of patient-volunteered height measurements, if known, if patient height could not be measured in the hospital;
- education in the above obesity recording improvements for all newly employed clinical staff;
- regular email, newsletter and patient file reminders (flags) to clinical staff reinforcing the requirement for patient height, weight and BMI recording in medical charts; and
- enhancements to clinical coding instructions to allow the determination of obesity by coding staff by calculating BMI if recorded height and weight measurements are available.
The education sessions for medical, nursing staff and clinical coding staff occurred prior to the commencement of the intervention and involved 16 dedicated sessions with hospital leaders, ward staff, dieticians, allied health staff and coding staff. Following the education sessions, clinical shift co-ordinators conducted obesity recording reminders at shift changes. Manual BMI calculators and tape measures were distributed to nursing stations and allied health offices and education posters on obtaining height by using the ulnar (forearm) length method were distributed in nursing stations, allied health offices and near all patient scales. Three email reminders written by hospital executives were sent to all hospital staff each quarter prompting staff to record weight, height and BMI and included: (i) justification of why BMI recording was required, (ii) recording locations in medical charts and (iii) links to BMI online tools. Additional BMI-related information was included in a staff newsletter and manual reminder flags were placed in patient files.
Audits
Obesity recording and accuracy of coding was examined 2 months post the 12-month intervention timeframe to allow records to be coded. Inclusion and exclusion criteria for the intervention were identical to the criteria of the original audit.17 Inclusion criteria comprised records for patients who were admitted to hospital for 5 days or more between 17 February 2020 and 16 February 2021, patients who were over the age of 18 at the time of hospital admission, and who had principal or additional diagnosis of “diabetes mellitus”, which includes Type II diabetes. Diagnoses of Type II diabetes was selected as an inclusion criterion as it has a confirmed link with obesity.18,19 Records of patients who were admitted to hospital more than once in the audit period were included. Exclusion criteria included records of patient boarders such as palliative care, and patients who use other health services such as outpatient treatments, patients diagnosed with Type 1 diabetes mellitus, those with a family history of diabetes mellitus or pre-existing diabetes mellitus, and keywords relating to Type 1, or “in pregnancy”. Further details of data collection are reported in the original audit.17 Site E was nominated as a control site due to no involvement in the original audit or intervention and was also audited using the same criteria and methods.
WACHS health information managers determined patients and their corresponding hospital admission episodes that fell within the study inclusion criteria. The audit process included a visual examination of the medical files to examine the inclusion or absence of obesity recording and weight, height and BMI recording. Comparison between electronically-coded obesity data and obesity recording in medical files was then conducted. The principal researcher undertook training on medical file examination techniques prior to the original audit to ensure sound data extraction methods were adhred to.
Data Analysis
Statistical analysis, equivalent to the original audit,17 was performed using Statistical Package for the Social Sciences (SPSS) version 27, which is common methodology used in clinical examinations of interventions and comparisons. Seven quantitative obesity recording measures were examined:
- percentage coded as obese,
- weight recorded,
- height recorded,
- BMI calculated using the Quetelet index (mass (kg)/height (m)2),
- height and weight recorded with no BMI,
- Obesity or BMI notations recorded, and
- Obesity or BMI notations recorded but height and weight not recorded.
Accuracy of clinical recording and coding of obesity-related conditions was examined by the analysis of seven additional measures:
- sensitivity,
- specificity,
- positive predictive values (PPVs),
- negative predictive values (NPVs),
- false positives,
- false negatives, and
- Cohen’s kappa values.
These seven analysis measures are commonly used in clinical examinations of interventions and comparisons, and are supported by several clinical research projects, including Ho et al20 and Lee et al.21 Sensitivity determined the degree of obesity recording in the patient admission data when it was first present in the medical files, while specificity measured the absence of obesity conditions in the patient admission data if the condition is absent in the medical files. PPVs examined cases that were coded as obese and then examined the occurrences of obesity notations in medical files; conversely, NPVs examined absence of obesity coding and then examined the absence of obesity notations in medical files. Analysis of false positives determined records coded as obese despite the obesity condition not being recorded and analysis if false negatives determined records not coded as obese despite the obesity condition being recorded. Cohen’s kappa values determined the agreement between the patient admission data and the obesity data within clinical records.
Results
A total of 166 patient records met the inclusion criteria and were assessed in the pre-intervention audit in September 2017 and 166 records were similarly assessed in the post-intervention audit between March and April 2021. The pre-intervention audit included records consisting of 87 males (52%) and 79 females (48%) aged between 25 and 98 years. A summary of the results of the statistical analysis of obesity data recording and accuracy is shown in Tables 1 and 2.
 |
Table 1 WACHS Patient Admission Obesity Accuracy and Inter-Rater Reliability Analysis |
 |
Table 2 WACHS Patient Obesity Recording Characteristics and Intervention Outcomes |
Pre-Intervention Obesity Recording and Coding
Obesity was coded in 8.4% of all patients, with weight being recorded in 56.6% of all patients and height being recorded in 12.6% of patients. BMI was calculated in 6% of all patients, and, of the patients who had height and weight recorded, 57.1% of patients did not have BMI recorded. Obesity or BMI notations were recorded in 16.2% of all patients; however, 12.6% of obesity or BMI notations were not supported by height or weight records. Sensitivity and specificity between obesity coding and obesity recordings in medical files resulted in 48.1% and 99.3%, respectively. Analysis of PPVs and NPVs resulted in 92.9% and 90.8%, respectively. Recorded false positives were 0.7%, while recorded false negatives were 51.9%. The Cohen’s kappa value was 0.59.
Post-Intervention Obesity Recording and Coding
The post-intervention audit included records consisting of 76 males (46%) and 90 females (54%) aged between 19 and 96 years. Obesity was coded in 10.2% of all patients, with weight being recorded in 57.8% of all patients and height being recorded in 33.1% of all patients. BMI was calculated in 33.7% of all patients, and, of the patients who had height and weight recorded, 21.8% did not have BMI recorded. Obesity or BMI notations were recorded in 13.2% of all patients; however, 12.6% of obesity or BMI notations were not supported by height or weight records. Sensitivity and specificity between obesity coding and obesity recordings in medical files resulted in 59.1% and 96.5%, respectively. Analysis of PPVs and NPVs resulted in 72.2% and 93.9%, respectively. Recorded false positives were 3.5%, while recorded false negatives were 40.9%. The Cohen’s kappa value was 0.6.
Figure 1 displays a histogram summary of the pre-intervention and post-intervention obesity recording results. Figure 2 displays the pre-intervention and post-intervention sensitivity and specificity results, including an aspirational specificity and sensitivity target established by the study authors of 100% in order to support enhanced obesity coding accuracy.
 |
Figure 1 WACHS obesity recording pre- and post-intervention. |
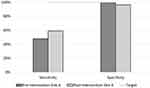 |
Figure 2 WACHS obesity data sensitivity and specificity: pre- and post-intervention. |
Discussion
Generally, the 12-month intervention at site A resulted in great improvements in the recording of obesity-related measures and obesity data accuracy. An increase from 6% to 33% in patient BMI recordings resulted, impacted by an increase from 12% to 33% in patient height measurements and an increase from 56% to 58% in patient weight measurements being obtained. Completeness of BMI recording was also positively demonstrated by a 35% reduction in cases where BMI was achievable using weight and height measurements but was not recorded. Written notations in clinical files of obesity or BMI also reduced by 3%, indicating increased use of BMI measurements to indicate obesity by clinicians rather than visual observation of obesity. Increasing use of BMI data to indicate obesity was also demonstrated in a reduction in cases of written notations in clinical files of obesity or BMI despite height and weight measurements not being obtained; a reduction of 7 cases occurred as well as reductions in cases where height and weight were not recorded.
Obesity accuracy results also generally improved due to the intervention, including sensitivity increases from 48% to 59%, NPV from 90% to 94% and reduction in false negatives from 52% to 41%. The Cohen’s kappa value also increased slightly, by 0.01%. The sensitivity result demonstrates that, where obesity was recorded in patient files, 59% were coded as obese; similarly, the NPV result of 94% demonstrated that, of all “normal weighted” coded patients, 94% did not have obesity notations recorded in medical files. The slight increase in the Cohen’s kappa value demonstrated moderate correlation between occurrences of coded obesity and the recorded obese patient notations in the medical files.
Conversely, the small reduction in specificity, from 99% to 96%, resulted in a slight reduction in accuracy when coding non-obese patients as “normal weighted”. A specificity measurement of 96% does, however, demonstrate very good accuracy. Similar to the reduced specificity result, a reduction in PPV was recorded, from 93% to 72%, which demonstrated a reduction in accuracy of the percentage of patients coded as obese who actually were obese. PPV outcomes are influenced by the prevalence of obesity in the patient population, which is very low in both the pre-intervention and post-intervention results, at 8% and 10%, respectively. The 21% reduction in PPV was due to an increase of 4 cases of false positives, where patients were incorrectly coded as obese despite no clinical recording of obesity in the patient files. Due to the low prevalence of 18 cases of obesity recording, a minor increase of 4 cases of false positives resulted in the large decrease in PPV. The 3% increase of false positives was also demonstrated in the results, which is a low measurement of false positives.
Control site E was also analysed to determine if external factors impacted obesity recording and accuracy during the intervention timeframe. The control site was not included in the pre-intervention analysis and did not receive obesity-related coaching or information. Site E demonstrated generally high levels of obesity recording and accuracy, with 14% of patients coded as obese, 87% of patient weights recorded and 37% of patient heights recorded. However, low translation to BMI measurements resulted in only 10% of total cases having BMI measurements recorded and 74% of cases with height and weight measurements not recording BMI measurements. Sensitivity, specificity, NPV and PPV measurements were relatively high, at 72%, 97%, 95% and 81% respectively. Both false positives and false negatives were relatively low at 3% and 28%, respectively. The Cohen’s kappa measurement was 0.7, which demonstrates good agreement between clinical files and coded obesity data. The control site obesity recording and coding accuracy results demonstrate site variability in processes and methods of recording obesity, which can be affected by site leadership, occupational functions or internal training. Site E demonstrated strong allied health obesity recording, mostly by dieticians, occupational therapists or physiotherapists. These functions were represented at all other examined sites; however, methods and levels of detail of recording differed and high levels of obesity recording appeared to be dependent on fastidious staff. While Site E demonstrates strong recording of obesity and coding accuracy, Table 1 demonstrates fluctuations across the five sites, likely due to variability of local instructions, processes and individual recording practices of staff.
Instruction to staff by healthcare leaders on requirements for obesity recording and education for staff on methods/tools to measure obesity, how obesity is used and recording locations within clinical files is essential for improved recording and accuracy of obesity data. Depending on the clinical presentation of the patient, there may be up to nine locations in patient files where obesity-related data can be captured, which may create confusion and reporting fatigue for staff. Staff may also not be aware of the importance of and uses of obesity data, such as staff safety approaches, clinical malnutrition or ABF/financial implications. Staff may not be aware of location of scales, particularly bariatric scales, or how to accurately measure height of bed-ridden patients using the ulna length method, demi-span method or knee height method.22–24
Organisational reinforcement of requirements for obesity recording is required and has been demonstrated to successfully influence obesity recording improvements in the intervention. Education and emphasis on obesity recording requirements should be conducted at site inductions for new staff and on an ongoing schedule in a variety of methods to ensure clinical understanding and compliance. While the intervention resulted in a 27% increase in BMI recording, which is a positive result, aspirational targets of 100% should be set by hospitals to support a mandatory reporting requirement. Quality improvement processes such as audits of clinical files to ensure accuracy and completeness of clinical data does occur within hospitals but these processes should be expanded to also include reviews of obesity recording. These improvement actions will increase obesity recording and coding in busy hospital environments where potential competing priorities such as immediate treatment needs, heavy workloads and lack of staff may be present.
In country hospitals where patients may be individually known to staff due to community interaction or repeated hospital admissions, a patient’s obesity status and history may be well known to staff but undocumented in patient files. This represents risks to both unfamiliar staff and the healthcare organisation. Furthermore, as obesity is higher in rural locations,14 country hospital staff are at risk of normalising obesity25 and accepting both visual and clinical indications of obesity as “normal” and therefore underestimating BMI. Indications of visual weight observations occurring was indicative in the intervention data, with 12.5% of BMI recordings being in the obese category and 39% being in the underweight or healthy weight categories. Under-reporting of obesity was also observed, predominantly in cases where patients were obese but able to move independently and obese patients admitted with mental health crises.
Although immediate improvement of obesity recording can be improved by implementing hospital education programs and auditing compliance, mandatory recording fields for patient height and weight should be considered as Australian hospitals move towards adoption of electronic health records. Electronic fields for recording obesity data should be made available and easily located by clinicians, which will reduce confusion around recording requirements and duplication. BMI calculations can be automated using height and weight measurements, and indicators or a “check box” should be designed for obese patients where the obesity condition impacts the patient’s management during their hospital admission, which will meet coding requirements for clinical coders to code the obesity condition. Studies in the United States have determined that identification of patient obesity has increased with the adoption of electronic health records, along with the ability to record frequency of obese patient hospitalisations and obesity treatment provided.26 This potential recording and coding improvement will also automate and address low BMI recording, where clinical coders currently are unable to code obesity if weight and height are available within the medical record but BMI is not calculated. Although the intervention improved clinical recording of BMI when weight and height measurements were obtained, 22% of records still did not record BMI despite availability of weight and height measurements.
Improved obesity data, including BMI, will indicate if both clinical risks and staff safety risks may be present and can inform bariatric risk management plans. Requirements for mobility assistance, additional staff support and bariatric equipment can all be documented in one clinical location within the bariatric risk management plan. During the pre- and post-intervention analyses, much of the clinical planning for bariatric support and required documentation/records were in a variety of locations in the patient file, including the general notes section. Risks can be present for staff, the patient and the organisation if the documented hazards and care plans are not easily located and understood by nursing staff. Increased obesity recording and accuracy of obesity data will result in improved ability to identify risks to both obese patients and staff who manage them and will allow risk management strategies to be implemented. This will reduce risks of injuries to healthcare staff and allow healthcare organisations to meet their workplace health and safety obligations, reduce workers’ compensation claims and maintain staff resourcing levels.
Finally, improved obesity recording and coding will positively impact healthcare funding. Hospital funding is partially generated by the Activity Based Funding (ABF) system, which provides payment for patient care that can vary significantly due to the complexity of patient treatment and length of stay. In cases of obesity, if the patient treatment is modified due to the obesity condition being present and poor obesity recording occurs, the hospital will not receive correct financing relating to the case. This can mean that treatment requirements such as staffing increases to safely accommodate lifting, turning or toileting of obese patients, requirements for bariatric equipment, increased medication or anaesthetic doses, increased rehabilitation requirements and increased clinical requirements for obese maternity patients will not be included in ABF reimbursements. Further exploration of financial impacts on hospitals due to lack of obesity recording or inaccurate coding should also be considered.
Case Studies of Inaccurate Obesity Recording/Coding
A 66-year-old male admitted with an anal abscess for treatment. Patient weight recorded as 118 kilograms, no height, BMI or obesity notations recorded. One to two staff required to assist in bed mobility tasks, sheet changes and washing of patient. Patient showered on trolley bath with two staff assisting. Patient transfers from bed using ceiling hoist and three staff to assist. Patient also hoisted to wheelchair with three staff to assist; clinically noted that positioning patient in wheelchair is challenging due to his increased weight. Patient hoisted back to bed with two staff assisting and use of ceiling hoist. Obesity not coded by clinical coders.
A 79-year-old female admitted with cellulitis of lower limb requiring treatment. Patient weight recorded as 134 kilograms, no height, BMI or obesity notations recorded. Patient required transfer from bed to toilet using one staff member to assist her and patient also required one staff member to assist her to lift legs back into bed. Patient was not able to turn herself in bed and required two staff to assist her with repositioning in bed. She also needed two staff to assist with “sit to standing” movement. Use of a standing hoist and two staff was required to transfer the patient from the toilet back to bed. Obesity not coded by clinical coders.
An 82-year-old female admitted with motor neurone disease requiring treatment. Patient weight recorded as 90 kilograms, no height, BMI or obesity notations recorded. Patient presented with mobility issues and clinical notes stated, “heavy transfer, will need to be a full hoist”. Obesity not coded by clinical coders likely as insufficient obesity recording to code obesity.
Limitations
The obesity recording and coding intervention commenced in February 2020, 3 weeks after the first cases of COVID-19 in Australia and approximately a month prior to COVID-19 restrictions and impacts in Western Australia. During the entire 12 months of the intervention significant healthcare planning for COVID-19 patient surges occurred and staff anxiety relating to COVID-19 was high. While the intervention was successful, it is very likely that obesity recording compliance of some staff was affected by the impacts of COVID-19.
Similarly, competing priorities and constraints relating to increased clinical workload, resourcing limitations and hospital pressures were present during the intervention. WACHS, and many other Western Australian hospitals, experienced increased hospital admissions and emergency department presentations due to a variety of factors such as increased mental health cases linked to illicit substance abuse, compounded during the intervention as a result of delays in mental health treatment due to COVID-19 restrictions. Increased workload and pressures potentially affected completeness of obesity recording and accuracy of obesity coding at higher than normal occurrences.
An additional limitation of this study is the inclusion of only patients with Type II diabetes. This health condition inclusion was selected as diabetes is strongly linked to obesity, and it is possible that rates of obesity recording in the data of patients with diabetes may be higher than in the general population. A broader examination of obesity recording accuracy of the general patient population may be made available by expanding the patient inclusion criteria. The accuracy of clinical data within patient files is also outside the scope of this study; this clinical data is recorded by trained clinical staff and is considered to be the gold standard for analysis and comparison.
Finally, researcher availability was also a limitation of this study. Sizable distances between WACHS hospitals and metropolitan locations impacted researcher ability to conduct manual file examinations. While the data collection and analysis demonstrated successful results, increased data collections and increased researcher availability should be considered for future similar research. The adoption of electronic health records by healthcare organisations will reduce this limitation by allowing researchers to examine patient files remotely.
Conclusion
The identification of obese patients admitted to hospitals is important for management of patient treatment, management of staff safety and reduction of organisational risks.4 Methods to increase obesity recording by clinical staff and accuracy of obesity coding by clinical coders were demonstrated by this successful intervention; however, more must be done to reduce risks to healthcare organisations, patients and staff. Due to high clinical workloads and timely patient treatment requirements, methods of obesity recording are required to be simple and user-friendly. Organisational progression in adoption of electronic health records will help to improve obesity recording, including mandatory recording of weight and height, automated BMI calculations and “check boxes” to indicate obesity impacts on patient care requirements. Until electronic health records are adopted by healthcare organisations, promotion of obesity data recording requirements should occur, including potential uses of this data for non-clinical purposes such as obese patient handling risk mitigation and ABF reimbursements. Auditing of obesity recording should occur, which could inform training and improvement strategies. In addition to staff safety improvements, increased obesity recording and coding accuracy will also increase accuracy of funding allocations to hospitals and reduce the necessity for hospitals to pay for costly obesity management requirements such as increased staffing and bariatric equipment out of operational hospital funds.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, Kim McClean, upon reasonable request.
Ethics Approval and Informed Consent
This study is approved by the Human Research Ethics Committee of Edith Cowan University (Ethics approval number: 2019-00051-MCCLEAN) and the Human Research Ethics Committee of the WA Country Health Service (Ethics approval number: RGS1359). A waiver of consent under section 2.3.10 of the National Statement on Ethical Conduct in Human Research (Australia) was approved by the Edith Cowan University Human Research Ethics Committee and the WA Country Health Service Human Research Ethics Committee.
Acknowledgments
We are grateful for the assistance and information gained from staff of the WA Country Health Service, particularly the Health Information Managers and Coding staff, and Ms. Meegan Kidd, Project Officer Clinical Coding.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Galinsky T, Hudock S, Streit J. Addressing the need for research on bariatric patient handling. Rehabil Nurs. 2010;35(6):242–247. doi:10.1002/j.2048-7940.2010.tb00054.x
2. Australian National Preventative Health Agency. Obesity: prevalence trends in Australia; 2014. Available from: http://sydney.edu.au/medicine/research/units/boden/ANPHA%20Obesity%20Prevalence%20Trends.pdf.
3. Department of Health Western Australia. WA Healthy Weight Action Plan 2019–2024; 2019. Available from: https://ww2.health.wa.gov.au/-/media/Files/Corporate/general-documents/Health-Networks/WA-Healthy-Weight-Action-Plan/PDF/Healthy-Weight-Action-Plan-2019-2024.pdf.
4. McClean K, Cross M, Reed S. Risks to healthcare organizations and staff who manage obese (Bariatric) patients and use of obesity data to mitigate risks: a Literature Review. J Multidiscip Healthc. 2021;14(1):577–588. doi:10.2147/JMDH.S289676
5. Australian Bureau of Statistics. National health survey: first results, 2017–2018 (cat. no. 4364. 0.55.001). Available from: https://www.abs.gov.au/ausstats/[email protected]/Lookup/by%20Subject/4364.0.55.001~2017-18~Main%20Features~Overweight%20and%20obesity~90.
6. Australian Bureau of Statistics. National health survey: first results, 1995 (cat. no. 4392.0); 1996. Available from: https://www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4392.0Main+Features11995?OpenDocument.
7. Australian Bureau of Statistics. Overweight and obesity in adults in Australia: a snapshot, 2007–08 (cat. no. 4842. 0.55.001); 2011. Available from https://www.abs.gov.au/ausstats/[email protected]/mf/4842.0.55.001/.
8. Walls HL, Magliano DJ, Stevenson CE, Backholer K, Mannan HR, Shaw JE. Projected progression of the prevalence of obesity in Australia. Obesity. 2012;20(4):872–878. doi:10.1038/oby.2010.338
9. Australian National Preventative Health Agency. Obesity: prevalence trends in Australia; 2014. Available from: http://sydney.edu.au/medicine/research/units/boden/ANPHA%20Obesity%20Prevalence%20Trends.pdf.
10. Pieracci F, Barie P, Pomp A. Critical care of the bariatric patient. Crit Care Med. 2006;34(6):1796–1804. doi:10.1097/01.CCM.0000217216.84983.0A
11. Australian Institute of Health and Welfare 2017. A picture of overweight and obesity in Australia 2017. Cat. no.PHE 216. Available from: https://www.aihw.gov.au/getmedia/45f6ecc6-0caf-4af4-9ffc-a44c885b33d2/aihw-phe-216.pdf.aspx?inline=true.
12. Stanfill MH, Williams M, Fenton SH, Jenders RA, Hersh WR. A systematic literature review of automated clinical coding and classification systems. J Am Med Inform Assoc. 2010;7(6):646–651. doi:10.1136/jamia.2009.001024
13. Australian Bureau of Statistics. Overweight and obesity in adults, Australia, 2004–05 (cat. no. 4719.0); 2008 Available from: http://www.abs.gov.au/ausstats/[email protected]/mf/4719.0/.
14. Western Australian Country Health Service. About Us: regional Health Services; n.d. Available from: https://www.wacountry.health.wa.gov.au/About-us/Overview.
15. Martin B, Chen G, Graham M, Quan H. Coding of obesity in administrative hospital discharge abstract data: accuracy and impact for future research studies. BMC Health Serv Res. 2014;14(70):1–8. doi:10.1186/1472-6963-14-70
16. Quan H, Li B, Saunders D, Parsons GA, Nilsson CI, Alibhai A. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43(4):1424–1441. doi:10.1111/j.1475-6773.2007.00822.x
17. McClean K, Cross M, Reed S. An audit of obesity data and concordance with diagnostic coding for patients admitted to Western Australian Country Health Service hospitals. Aust J Adv Nurs. 2020;38(1):45–52. doi:10.37464/2020.381.99
18. American Society for Metabolic and Bariatric Surgery. Fact sheet: obesity in America. American Society for Metabolic and Bariatric Surgery; 2013. Available from https://asmbs.org/app/uploads/2014/06/Obesity-in-America-1.pdf.
19. Medical Research Council United Kingdom. Diabetes: facts and stats. Diabetes UK; 2015. Available from https://www.mrc.ac.uk/documents/pdf/diabetes-uk-facts-and-stats-june-2015.
20. Ho ML, Lawrence N, Van Walraven C, et al. The accuracy of using integrated electronic health care data to identify patients with undiagnosed diabetes mellitus. J Eval Clin Pract. 2012;18(3):606–611. doi:10.1111/j.1365-2753.2011.01633.x
21. Lee YYC, Roberts CL, Young J, Dobbins T. Using hospital discharge data to identify incident pregnancy-associated cancers: a validation study. BMC Pregnancy Childbirth. 2013;13(37):1–6. doi:10.1186/1471-2393-13-37
22. Han TS, Lean ME. Lower leg length as an index of stature in adults. Int J Obes Relat Metab Disord. 1996;20(1):21–27.
23. Hickson M, Frost G. A comparison of three methods for estimating height in the acutely ill elderly population. J Hum Nutr Diet. 2003;16(1):13–20. doi:10.1046/j.1365-277x.2003.00416.x
24. Jarzem PF, Gledhill RB. Predicting height from arm measurements. J Pediatr Orthop. 1993;13(6):761–765. doi:10.1097/01241398-199311000-00014
25. Maynard LM, Serdula MK, Galuska DA, Gillespie C, Mokdad AH. Secular trends in desired weight of adults. Int J Obes. 2006;30(9):1375–1381. doi:10.1038/sj.ijo.0803297
26. Mattar A, Carlston D, Sariol G, et al. The prevalence of obesity documentation in Primary Care Electronic Medical Records. Are we acknowledging the problem? Appl Clin Inform. 2017;8(1):67–79.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
