Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Evaluating the Effect of COVID-19 on Outpatient Opioid Utilization Among Health First Colorado Members and a National Non-Medicaid Cohort: An Interrupted Time Series Analysis
Authors Anderson HD , Patterson VP, Wright G , Rawlings JE, Moore GD, Leonard J, Page RL II
Received 1 July 2023
Accepted for publication 26 August 2023
Published 18 September 2023 Volume 2023:19 Pages 745—753
DOI https://doi.org/10.2147/TCRM.S424961
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Heather D Anderson,1 Vanessa Paul Patterson,1 Garth Wright,1 Julia E Rawlings,1 Gina D Moore,1 Jim Leonard,2 Robert L Page II1
1Department of Clinical Pharmacy, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Anschutz Medical Campus, Aurora, CO, USA; 2Colorado Department of Health Care Policy and Financing, Denver, CO, USA
Correspondence: Robert L Page II, Clinical Pharmacy, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, 12850 E. Montview Blvd, Mail Stop C238, Aurora, CO, 80045, USA, Tel +1 303-724-2616, Fax +1 303-724-2627, Email [email protected]
Objective: COVID-19, coinciding with the opioid epidemic in the United States, has had significant impacts on health-care utilization. While mixed, early analyses signaled a potential resurgence in opioid use following the pandemic. The primary study objective was to assess the association of the COVID-19 pandemic with opioid utilization among Health First Colorado (Colorado’s Medicaid Program) members and a non-Medicaid managed care cohort who did not have a diagnosis of cancer or sickle cell disease.
Patients and Methods: Using an interrupted time series and segmented regression analysis, this population-level study assessed the association of the COVID-19 pandemic on prescribed utilization of long- and short-acting opioid analgesics among Health First Colorado members and a random sample of non-Medicaid managed care members. Pharmacy claims data for both cohorts were assessed between October 1, 2018, and September 30, 2021, with April 2020 identified as the interruption of interest. We evaluated the following monthly opioid use measures separately for short-acting and long-acting opioids: number of members filling an opioid, total fills, and total days supplied.
Results: Short- and long-acting opioid utilization was significantly decreasing among Health First Colorado members in the 18 months prior to the start of COVID-19. After the onset of the pandemic, utilization stabilized and slopes were not significantly different from zero. Among the non-Medicaid managed care cohort, short- and long-acting opioid utilization significantly decreased in the 18 months leading up to the onset of the pandemic. After the onset of the pandemic, utilization of long-acting opioids stabilized, while utilization of short-acting opioids significantly increased.
Conclusion: While we observed an increase in opioid utilization measures post-pandemic in the non-Medicaid managed care cohort, a similar increase was not observed in Health First Colorado members suggesting that thoughtful opioid policies put in place pre-pandemic may have been effective at controlling potential inappropriate opioid utilization.
Keywords: interrupted time series, segmented regression, pain management, health care utilization, Medicaid, managed care, opioids
Introduction
On March 13, 2020, the President of the United States declared that the COVID-19 pandemic was a national emergency and the face of healthcare delivery was forever transformed. Direct access to medical providers, elective procedures, and even prescription medications was extremely limited and reduced.1,2 To help address these significant healthcare delivery challenges, the Secretary of the Department of Health and Human Services waived certain requirements of Social Security Act Titles XVIII, XIX, and XXI. These waivers eased the usual restrictions placed upon state Medicaid programs and allowed easier access to prescription medications through modifications in prior authorization, allowance for early refills, increased quantity limits, and expansion of telehealth.1 In the State of Colorado, the Department of Health Care Policy and Financing (HCPF) manages, administers, and delivers the statewide Medicaid benefit, also known as Health First Colorado. The Department took action to defer prior authorization requirements on all drugs for which there was an existing 12-month prior authorization approval in place so that each prior authorization could be extended once every 90 days on a case-by-case basis.3 In the case of opioid analgesics, the Department, like other state Medicaid programs, allowed pharmacists to enter overrides at the point of sale granting early refill of opioids with refill tolerance of greater than 50% of the previous fill utilized, so as not to disrupt access to pain medications.3 As the opioid overdose pandemic in the United States was occurring in parallel with the COVID-19 pandemic, the expanded potential for abuse or diversion combined with an increase in opioid prescribing and utilization with the easing of opioid restrictions, was a major concern.3–5
Prior to the pandemic, HCPF had already implemented many safe guards and novel programs to enhance appropriate prescribing of opiates and deter potential abuse and diversion.6 These policies, which remained in place during the pandemic, consisted of quantity limits on short-acting opioids, coverage of telemedicine, safety review high morphine milligram equivalent prescriptions, limits on concomitant prescribing of opioids and benzodiazepines, and days’ supply limitations for those newly initiated on opioids (opioid naïve). In tandem, the Department, in collaboration with the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, had already developed a unique opioid pain teleconsultation service that allowed for provider-to-provider consultations with a medical pain specialist. These consultations were triggered for Health First Colorado members based on the above-mentioned policies and morphine milligram equivalent cutoffs.7
While opioid overdose admissions and deaths following the beginning of the pandemic have been widely reported, limited data exist on opioid prescribed utilization pre- and post-COVID specifically within the United States Medicaid population that includes some of the nation’s most socially and economically vulnerable citizens.8–13 This study was designed to evaluate opioid prescribed utilization trends in Health First Colorado members and a cohort of non-Medicaid managed care enrollees before and after the COVID-19 pandemic through evaluation of pharmacy claims of both short- and long-acting opioids, thus evaluating the potential efficacy of current opioid prescribing safeguards and programs in Colorado.
Materials and Methods
Study Design
Leveraging a quasi-experimental study design, namely an interrupted time series (ITS), we retrospectively assessed the effect of the emergence of COVID-19 on opioid prescribed utilization among Health First Colorado Medicaid members and a national cohort of non-Medicaid managed care members represented in a large, United States managed care database. Using these two distinct cohorts allows for a comparison of trends at the state versus national level, as well as, the impact from the perspective of a highly vulnerable versus a fully insured and employed population.
Data Source and Study Population
Two data sources were leveraged for this observational study: Health First Colorado member claims and the IQVIA PharMetrics® Plus for Academics claims database. IQVIA PharMetrics® Plus for Academics is an insurance claims database that includes paid medical and pharmacy claims for over 112 million unique enrollees across the United States.14 The University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences holds a license for a random sample of approximately 25 million patients from PharMetrics® Plus for Academics. Data are longitudinal and span from January 1, 2006, through June 30, 2022. In each claims data source available, claims-level variables include medications filled (specifically medication code, fill date, and days supplied). Patient-level demographic variables include year of birth, sex, and race/ethnicity (Health First Colorado only). The enrollees included in PharMetrics® Plus for Academics are nationally representative in terms of age and sex distributions of patients in the US commercially insured population.
Opioid prescription fill data were obtained from Health First Colorado Medicaid claims and PharMetrics Plus for Academics® from October 1, 2018–September 30, 2021, which allowed for 18 months prior to and 18 months following the interruption of interest (defined as April 2020). We included members of all ages who had at least one fill of a short-acting or long-acting opioid during the study period. Short-acting opioids were defined as any brand name or generic immediate release oral formulation consisting of the following: codeine and its acetaminophen combinations, hydrocodone and its ibuprofen or acetaminophen combinations, hydromorphone, meperidine, morphine, pentazocine, oxycodone and its ibuprofen or acetaminophen combinations, oxymorphone, tapentadol, and tramadol and its acetaminophen combinations. Brand name and generic long-acting opioids consisted of oral longer acting, extended release, or transdermal formulations consisting of the following: buprenorphine patch, fentanyl patch, hydrocodone, hydromorphone, oxycodone, tapentadol, and methadone (due to its long half-life). We excluded members with diagnoses of cancer or sickle cell disease at any time in the available data. PharMetrics® Plus for Academics enrollees with Medicaid or a State Children’s Health Insurance Program were excluded in order to create a non-Medicaid managed care cohort.
Outcome Measures
The unit of time for analysis was defined by calendar month, with April 2020 representing the COVID-19 point of interruption for the purposes of this study. COVID-19 was declared a national emergency on March 13, 2020, and subsequently there was a rollout of infection control and public health measures occurring in the weeks that followed. In Colorado, nonessential medical procedures were suspended effective March 19 with state-wide Stay at Home orders initiated on March 25. Therefore, April 2020 was identified as the month that most closely aligned with the introduction of pandemic-related changes to healthcare service delivery.
Monthly-aggregated outcomes were calculated from October 1, 2018–September 30, 2021, which included 18 months of measures prior to and following the interruption in April 2020. We calculated the following six outcomes on a monthly basis separately for the Colorado Medicaid cohort and the non-Medicaid managed care cohort: (1) number of members filling a short-acting opioid each month; (2) total number of short-acting opioid fills each month (includes duplicated members who filled a short-acting opioid more than once); (3) total short-acting opioid days supplied each month, calculated by adding the total days supplied for all short-acting opioid claims across all patients; (4) number of members filling a long-acting opioid each month; (5) total number of long-acting opioid fills each month (includes duplicated members who filled a long-acting opioid more than once); (6) total long-acting opioid days supplied each month, calculated by adding the total days supplied for all long-acting opioid claims across all patients.
Statistical Analyses
The ITS design for this study was implemented through the use of a segmented regression analysis.15 Segmented regression allows for the assessment and comparison of temporal trends across different time periods. By fitting a regression in the pre- and post-interruption time periods separately, we estimated the slopes during both the pre-period and the post-period and the change in slope from the pre-period to the post-period. We also estimated the level change, which is defined as the difference between the pre-period and post-period predicted values at the time of the interruption. The analyses were conducted at the population level, with no matching of members from the pre-interruption time period to the post-interruption time period. We assessed for auto-correlation and seasonality, neither of which were significant and were therefore not included in the final ITS models. All ITS models were stratified by short-acting and long-acting opioid analgesics, as well as by cohort population, namely Health First Colorado Medicaid and non-Medicaid managed care cohorts. Analyses were generated using SAS software. Copyright © 2016 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Results
During the study period, we identified 248,962 Health First Colorado members and 470,555 non-Medicaid managed care members with at least one opioid fill (Table 1). Approximately 60% of the Medicaid cohort was female and 57% of the non-Medicaid managed care cohort was female. The average age was 35 years old in the Medicaid cohort and 48 years old in the non-Medicaid managed care cohort. The majority of the Health First Colorado members were White (44%) or multiple races (40%). Race/ethnicity information was not available for the non-Medicaid managed care cohort. Demographic characteristics of members in each cohort were similar in the pre-period and the post-period. Note, as a population-level analysis, cohort members could have been included in both time periods, and demographic characteristics were therefore not compared for statistical differences from pre- to post-COVID interruption.
 |
Table 1 Demographic Characterisitcs of the Health First Colorado Cohort and Non-Medicaid Managed Care Cohort, Stratified by Time Peroid |
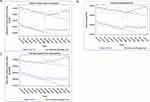
Prior to the COVID interruption, prescribed utilization of short-acting opioids was significantly decreasing in the non-Medicaid managed care cohort (Table 2, Figure 1). Specifically, the number of non-Medicaid managed care members filling a short-acting opioid was decreasing by approximately 294 members per month (slope = −294.8, p < 0.01) and the total number of short-acting opioid fills was decreasing by 242 fills per month (slope = −241.8, p < 0.05). Prescribed utilization of long-acting opioids was also significantly decreasing in the non-Medicaid managed care cohort prior to the interruption (Table 2, Figure 2). During the period after the COVID interruption, prescribed utilization of long-acting opioids remained stable for non-Medicaid managed care members (p > 0.05). However, prescribed utilization of short-acting opioids significantly increased during the period following the COVID interruption. The number of members filling a short-acting opioid (slope = 262.46, p < 0.01), the total number of short-acting opioid fills (slope = 458.49, p < 0.01), and the total days supplied of short-acting opioids (slope = 4660.0, p < 0.01) all had significantly positive slopes after the interruption.
 |
Table 2 Interrupted Time Series Segmented Regression Analysis of Opioid Utilization Outcomes Before and After Emergence of the COVID-19 Pandemic |
As with the non-Medicaid managed care cohort, prescribed utilization of short-acting opioids was significantly decreasing prior to the COVID interruption for Health First Colorado members (Table 2, Figure 1). For example, the number of Health First Colorado members filling a short-acting opioid was decreasing by approximately 327 members per month (slope = −327.20, p < 0.01). Prescribed utilization of long-acting opioids was also significantly decreasing prior to the COVID interruption (Table 2, Figure 2). We estimated a significant level increase at the time of the interruption (ie, difference between the pre-period and post-period predicted values at the time of the interruption) for each prescribed utilization outcome for long-acting opioids. For example, the level change of predicted Health First Colorado members filling a long-acting opioid increased by 185 members from just before the COVID interruption to just after the COVID interruption (level change = 184.61, p < 0.05). After this immediate increase, prescribed utilization of long-acting opioids in the Health First Colorado cohort remained stable. In contrast to the significantly increasing prescribed utilization of short-acting opioids after the COVID interruption in the non-Medicaid managed care cohort, utilization remained stable among Health First Colorado members, with slopes for each of the three prescribed utilization measures for short-acting opioids being non-significant (p > 0.05).
Discussion
To our knowledge, this is the first evaluation describing changes in prescribed opioid utilization before and after the onset of COVID-19, specifically in a Medicaid population. Based on our ITS analysis, we unexpectedly observed an initial increase in prescribed utilization of short- and long-acting opioids in our Health First Colorado population immediately following the onset of the pandemic; however, the utilization of both types of opioids stabilized and remained unchanged in the 18 months following the COVID interruption. This trend was verified in a nationwide, non-Medicaid managed care cohort, which saw similar trends for long-acting opioids. However, an increase in utilization of short-acting opioids, which could be reflective of acute use, was noted in the non-Medicaid managed care cohort following the COVID interruption. Within our Health First Colorado cohort, we hypothesize this stabilization may be due to opioid prescribing safeguards and programs put in place prior to the pandemic.7
Our findings somewhat mirror the findings of Rikin et al, who also evaluated the effect on outpatient prescribing of opioids in a single health system in New York City pre- and post-COVID interruption using an ITS study design.13 Unlike our study, these investigators stratified opioid utilization based on acuity in which “chronic use” was defined as the patient having been prescribed an opioid in excess of 90 days and “non-chronic use” was defined as less than or equal to 90 days. Similar to our study, Rikin et al found that prior to the pandemic both chronic and non-chronic opioid prescriptions were decreasing (slope −0.8 prescriptions per week; 95% confidence interval (CI): −0.5, 1.1; slope −0.4 prescriptions per week; 95% CI: −0.7, −0.1, respectively). However, for chronic use during the initial restriction period, there was an immediate increase by 7.5% compared to their predicted estimates (34.8 prescriptions, 95% CI: 8.0, 61.7) with no other significant changes in prescriptions during the remainder of the study period. In the case of non-chronic use during the COVID restriction phase, there was an immediate decrease by 34.1% compared to predicted (−83.9 prescriptions, 95% CI: −125, −38.8) with a slope increase occurring during re-opening compared to the restriction period (6.4 prescriptions per week, 95% CI: 2.2, 10.7).
Within our ITS study, we evaluated opioid utilization at both a state (Health First Colorado cohort) and national (non-Medicaid managed care cohort) level with a more granular perspective of number of members filling an opioid, total fills, and total days supplied stratified by short- and long-acting opioids and contextualized our Colorado Medicaid findings with those of a nation-wide non-Medicaid cohort. While our findings for both study cohorts are similar to the Rikin’s pre-interruption period, we found a stabilization in opioid utilization during the post-period for the Health First Colorado Medicaid cohort, which remained unchanged in the 18 months following the COVID-19 interruption independent of the type of opioid used. However, if we consider utilization of short-acting opioids as a surrogate for non-chronic pain and long-acting opioids for chronic use, our analysis at the national level in non-Medicaid members mirrors Rikin et al’s findings. Nonetheless, our evaluation of opioid utilization for both of our study cohorts adds to the literature and provides lessons learned from a health policy perspective that can be potentially applied if, or when, the next pandemic does occur.
The national non-Medicaid, managed care cohort from the IQVIA PharMetrics® Plus database was used such that several comparisons and observations could be made. First, while the Medicaid benefit is jointly funded by both the federal government and each state, healthcare services and prescription benefits are created, administered, and monitored by each individual, respective state. Second, the Medicaid benefit is designed to provide healthcare coverage and prescription benefits for the nation’s most vulnerable, low-income individuals and families, making it possible for millions of low-income children, parents, pregnant women, people with disabilities, and seniors to receive health care. During the study period, both cohorts had access to prescription opioids; however, regulation is determined by specific criteria set by each state as is the case for Medicaid members and by pharmacy benefit managers for each individual third-party insurance plan for the managed care cohort. In the case of Health First Colorado members, access to opioids was actually increased during the pandemic as pharmacists could allow for early opioid refills with refill tolerance of greater than 50% of the previous fill utilized.3
This evaluation has several limitations. As with all pharmacy and medical claim analyses, we can only infer opioid prescription acquisition and not administration. Also, we did not evaluate opioid-related overdose deaths or admissions during the study period for several reasons. First, HCPF does not have access to specific death data for their members, only the termination date of benefits. Second, the opioid overdose epidemic in the United States has been described as occurring in four waves: wave 1: rise in prescription opioid overdose deaths (1999–2010), wave 2: rise in heroin overdose deaths (2010–2013), wave 3: rise in non-prescription synthetic opioid overdose deaths, and wave 4: rise in polysubstance deaths, including methamphetamine and synthetic, illegal fentanyl (2013-present).16 Nationwide, the COVID-19 pandemic occurred during the fourth wave of the opioid overdose epidemic, meaning that the majority of overdose deaths were primarily driven by non-prescription, illegally obtained, synthetic opiates. Between 2019 and 2020, Colorado did experience a 54% increase in drug overdoses and a 38% increase in drug overdose deaths; however, these increases were primarily related to illegally obtained, synthetic non-prescription opioids such as fentanyl, heroin, and methamphetamine and, to a much lesser extent, to prescription opioids.17 Therefore, opioid overdose emergency room or hospital admissions in Colorado are confounded by polysubstance use, and illegally obtained synthetic opiates would not be captured in pharmacy claims. Nonetheless, our findings from this ITS study corroborate these statistics as we did not see a significant increase in prescription opioid utilization post-COVID-19. While not diminishing the importance that prescription opioids play in the overall overdose epidemic, state health policy implementing safe guards and programs for appropriate prescribing is one measure that can be directly controlled in order to limit the volume of prescription opioids that enter into the community and could potentially contribute to this epidemic. Finally, within the managed care, non-Medicaid cohort, we did not have access to specific opioid regulation policies from the 80 plus insurance plans included.
Conclusion
With the COVID-19 interruption, opioid utilization and prescribing for both short- and long-acting opioids remained stable in the Health First Colorado population, even in the face of improved prescription access during the pandemic. However, in the non-Medicaid managed care population, an increase in short-acting opioids was demonstrated across all utilization measures following the onset of COVID-19. Even within the most vulnerable population, these findings suggest that established safeguards and programs set forth by HCPF such as access to telemedicine, provider to provider pain consultations, opioid quantity and day supply limits, and safety review of high morphine milligram equivalent prescriptions may be effective in controlling potential inappropriate opioid utilization. Overall, the COVID-19 pandemic allowed for the evaluation of current opioid policies and interventions. Nonetheless, the interventions described within can serve as a model for other state Medicaid programs and health systems. Building on these data, future research should be focused on linking overdose death data with opioid utilization to fully appraise and contextualize the impact of these health policy interventions on the opioid epidemic during the COVID-19 pandemic.
Abbreviations
HCPF, Department of Health Care Policy and Financing; ITS, Interrupted time series; CI, Confidence interval.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are not publicly available. The pharmacy claims data generated belong to the Colorado Department of Health Care Policy and Finance (HCPF), were collected as part of its routine clinical and administrative activities, and approved for use by Dr. Jim Leonard, who is author on this manuscript and the Deputy Director of HCPF Pharmacy Office. The University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences has a data agreement with HCPF to house all pharmacy and medical claims, as well as, conducts analytic evaluations for drug utilization review. For IQVIA PharMetrics® Plus for Academics claims database, the Skaggs School of Pharmacy and Pharmaceutical Sciences has a data agreement with PharMetrics® to use their database. This analysis and manuscript has been approved by HCPF, the Colorado Data Review/Safe Harbor Committee, and IQVIA PharMetrics®.
Ethics Approval and Informed Consent
This study was reviewed and approved as exempt by the University of Colorado, Anschutz Medical Campus Institution Review Board (February 1, 2022), as all patient information were de-identified, and the Colorado Data Review Board/Safe Harbor Committee from the State of Colorado.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This research was funded through the Colorado Department of Health Care Policy and Financing, Denver, Colorado, USA.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Department of Health and Human Services. Office of the Inspector General. Changes made to state’s Medicaid programs to ensure beneficiary access to prescriptions during the COVID-19 pandemic; 2020. Available from: https://oig.hhs.gov/oas/reports/region6/62004007.pdf.
2. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi:10.15585/mmwr.mm6936a4
3. Centers for Medicaid and Medicare. National Medicaid Fee-For-Service (FFS), FFY 2020 Drug Utilization Review (DUR) Annual Report. Available from: https://www.medicaid.gov/medicaid/prescription-drugs/downloads/2020-dur-ffs-summary-report.pdf.
4. Alexander GC, Stoller KB, Haffajee RL, Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann Intern Med. 2020;173(1):57–58. doi:10.7326/M20-1141
5. O’Donnell J, Gladden RM, Mattson CL, et al. Vital signs: characteristics of drug overdose deaths involving opioids and stimulants — 24 States and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep. 2020;69(35):1189–1197. doi:10.15585/mmwr.mm6935a1
6. Colorado Department of Health Care Policy and Financing: pain management resources and opioid use; 2023. Available from: https://hcpf.colorado.gov/pain-management-resources-and-opioid-use.
7. Anderson HD, Patterson V, Wright G, et al. Evaluation of an opioid pain teleconsultation service to address the opioid overdose epidemic in Colorado: a Health First Colorado demonstration project. J Am Pharm Assoc. 2023;63(1):301–308. doi:10.1016/j.japh.2022.11.009
8. Auty SG, Griffith KN. Medicaid expansion and drug overdose mortality during the COVID-19 pandemic in the United States. Drug Alcohol Depend. 2022;232:109340. doi:10.1016/j.drugalcdep.2022.109340
9. Friedman JR, Hansen H. Evaluation of increases in drug overdose mortality rates in the US by race and ethnicity before and during the COVID-19 pandemic. JAMA Psychiatry. 2022;79(4):379–381. doi:10.1001/jamapsychiatry.2022.0004
10. Slavova S, Rock P, Bush HM, et al. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. doi:10.1016/j.drugalcdep.2020.108176
11. Center for Disease Control. Center for Preparedness and Response. Increase in fatal drug overdoses across the United States driven by synthetic opioids before and during the COVID-19 pandemic. Center for Disease Control and Prevention; 2020. Available from: https://emergency.cdc.gov/han/2020/han00438.asp.
12. Burgess-Hull AJ, Smith KE, Panlilio LV, et al. Nonfatal opioid overdoses before and after COVID-19: regional variation in rates of change. PLoS One. 2022;17(3):e0263893. doi:10.1371/journal.pone.0263893
13. Rikin S, Perez HR, Zhan C, et al. Changes in outpatient opioid prescribing during the COVID-19 pandemic: an interrupted time series analysis. J Prim Care Commun Health. 2022;13:1–6. doi:10.1177/21501319221076926
14. IQVIA. IQVIA PharMetrics plus for academics users guide & data dictionary; 2017.
15. Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi:10.1046/j.1365-2710.2002.00430
16. Jenkins RA. The fourth wave of the US opioid epidemic and its implications for rural US: a federal perspective. Prev Med. 2021;152(Pt 2):106541. doi:10.1016/j.ypmed.2021.106541
17. Colorado Health Institute. A parallel epidemic: more overdose deaths more overdose deaths in 2020, fentanyl fatalities spike; 2022. Available from: https://www.coloradohealthinstitute.org/research/2020overdose_dashboard.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.